4 Fast Facts About the Gut-Brain Connection
Discover the fascinating bidirectional communication between your gut and brain.
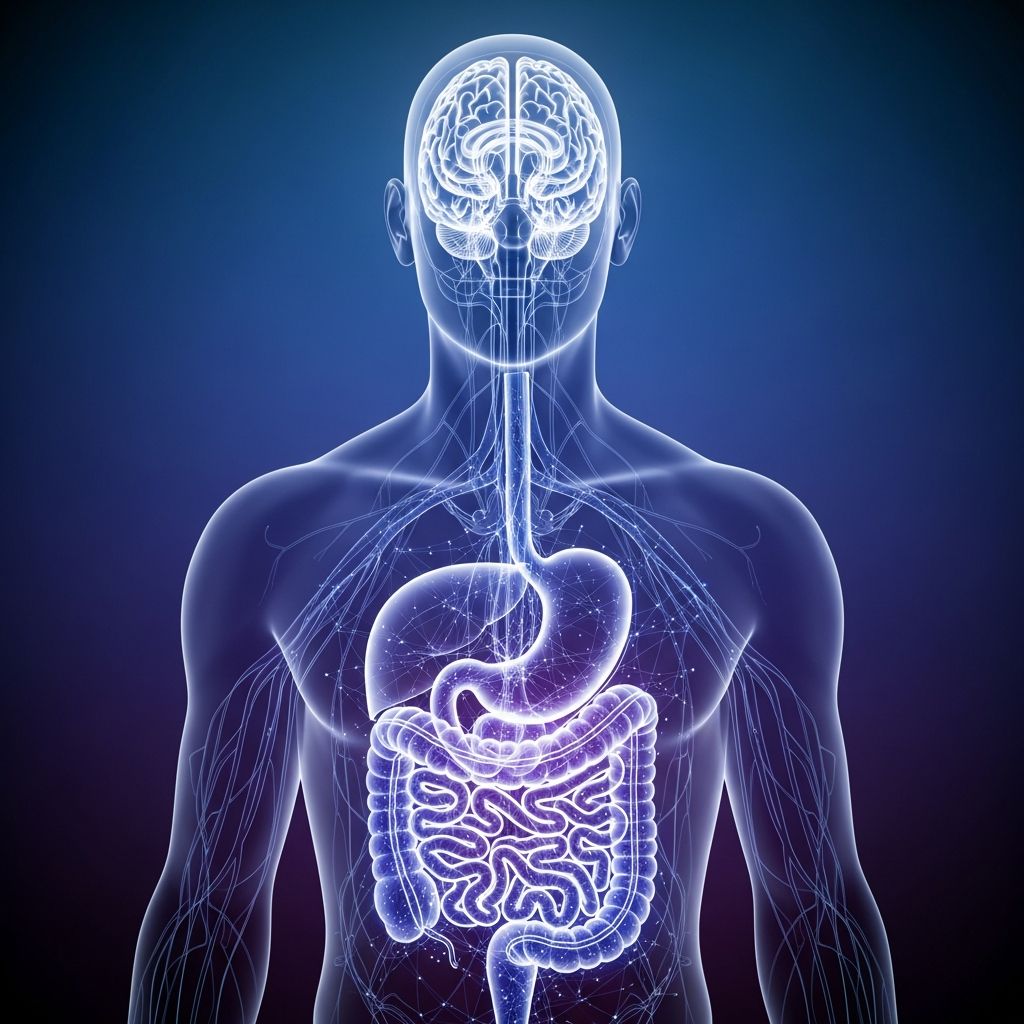
The relationship between your gut and your brain is far more intimate than you might think. Recent scientific research has revealed that your digestive system and central nervous system are in constant communication through multiple pathways, creating what scientists call the gut-brain axis. This bidirectional communication network influences everything from your mood and cognitive function to your digestive health and immune response. Understanding the fundamentals of this connection can help you appreciate how interconnected your body truly is and why maintaining gut health is crucial for overall wellness.
Fact 1: The Vagus Nerve Creates a Direct Physical Connection
One of the most remarkable discoveries about the gut-brain connection is the role of the vagus nerve, which serves as the primary physical highway between your digestive system and your brain. This nerve is one of your 12 cranial nerves and is the longest cranial nerve in your body, extending from your brain through your neck, chest, and abdomen.
Your gut contains what scientists call the enteric nervous system, often referred to as the “second brain.” This complex network contains approximately 168 million neurons, which is more than the number of neurons in your spinal cord. The vagus nerve directly connects this “second brain” to your central nervous system, creating a two-way communication channel that constantly transmits information.
How the Vagus Nerve Works:
- Sends sensory signals from your gut to your brain about digestive conditions
- Carries motor signals from your brain back to your gut, controlling digestive functions
- Communicates information about nutrient absorption and food movement
- Transmits signals related to fullness, hunger, and digestive comfort
- Relays information about the gut microbiome’s status to your brain
The vagus nerve plays a crucial role in regulating higher-order cognitive functions such as anxiety, depression, learning, and memory. When you experience stress or emotional changes, your brain sends signals through the vagus nerve that directly affect your digestive processes. Conversely, the state of your digestive system can influence your emotional well-being and cognitive performance.
Fact 2: Neurotransmitters Bridge the Chemical Gap
Beyond the physical connection of nerves, your gut and brain communicate through chemical messengers called neurotransmitters. These molecules are produced in both your brain and your gut and play essential roles in regulating mood, behavior, and cognitive function. The chemical communication between these two systems is remarkably sophisticated and influences numerous aspects of your health.
Key Neurotransmitters in the Gut-Brain Axis:
Serotonin is one of the most important neurotransmitters in this system. Interestingly, approximately 90% of your body’s serotonin is produced not in your brain but in your gut. Specifically, the enterochromaffin cells of your small intestine produce the highest concentration of serotonin. This neurotransmitter is involved in bowel function, nausea management, appetite regulation, mood, learning, memory, and sleep. When your gut microbiota is imbalanced, serotonin production can be disrupted, potentially affecting your mood and sleep quality.
Your gut microbes also produce gamma-aminobutyric acid (GABA), a neurotransmitter that plays a critical role in reducing anxiety and promoting feelings of calm. GABA helps regulate fear responses and anxiety levels, and when your gut microbiota is healthy and balanced, GABA production supports mental wellness. Studies have shown that probiotics can influence GABA production, suggesting a direct link between gut health and anxiety management.
Beyond individual neurotransmitters, the gut microbiota produces numerous other chemical compounds that affect brain function. These include short-chain fatty acids, bile acid metabolites, and amino acid derivatives, all of which can cross the blood-brain barrier or exert systemic effects that influence neurological function.
Fact 3: Gut Microbiota Directly Influences Brain Function
Your gut is home to trillions of microorganisms, collectively known as the gut microbiota or microbiome. These bacteria, viruses, and fungi are not invaders to be feared but essential partners in maintaining your health. Recent research has established that the composition and diversity of your gut microbiota directly affect your brain function, behavior, and mental health.
The gut microbiota influences your brain through several mechanisms. First, these microbes produce short-chain fatty acids (SCFAs) such as butyrate, propionate, and acetate by digesting dietary fiber. These SCFAs have multiple effects on brain function, including reducing appetite, supporting cognitive processes, and maintaining the integrity of the blood-brain barrier, which is crucial for protecting your brain from harmful substances.
Butyrate, in particular, plays a vital role in supporting brain health. It strengthens the blood-brain barrier and influences neuroinflammation, potentially protecting against neurodegenerative conditions. When you consume adequate fiber, your gut microbes produce more butyrate, which creates a protective effect for your brain.
The gut microbiota also metabolizes bile acids and amino acids to produce other bioactive compounds that affect brain function. Additionally, research has revealed genetic overlap between gastrointestinal disorders and psychiatric disorders, suggesting a shared biological basis for the gut-brain connection. This means that the health of your microbiota can influence your susceptibility to mental health conditions.
How Microbiota Affects Specific Conditions:
- Anxiety and depression: Imbalances in microbiota composition correlate with increased anxiety and depressive symptoms
- Stress resilience: A healthy microbiota supports better stress management and emotional regulation
- Cognitive function: Certain bacterial strains enhance learning, memory, and concentration
- Neurodegenerative diseases: Alterations in microbiota composition have been linked to Parkinson’s disease and other neurodegenerative conditions
- PTSD and trauma: The microbiota influences how the brain processes and responds to traumatic stress
Fact 4: The Gut-Brain Connection is Bidirectional
A critical aspect of the gut-brain axis is that communication flows in both directions. Your brain doesn’t simply receive messages from your gut; it also actively influences gut function. This bidirectional relationship means that stress, emotions, and mental states can directly alter your digestive processes, while your digestive health can influence your mood and cognition.
Brain-to-Gut Communication:
When you experience stress, your brain activates the parasympathetic nervous system and sends signals through the vagus nerve that alter stomach acid production, digestive enzyme secretion, and gut motility. This is why stress can cause stomach upset, heartburn, or constipation. Research has even established a direct link between stress and stomach ulcer formation, with brain regions involved in emotion regulation (the rostral insula and medial prefrontal cortex) directly controlling digestive function.
Gut-to-Brain Communication:
Simultaneously, your gut sends information to your brain about nutrient availability, immune status, and microbial composition. When your gut is inflamed or dysbiotic (having an imbalance of microorganisms), your brain receives these distress signals, which can trigger anxiety, brain fog, or mood disturbances. Conversely, a healthy, diverse microbiota sends positive signals that support optimal brain function.
This bidirectional communication explains why both stress management and dietary choices matter for overall health. You can improve your gut health through nutrition and lifestyle, which sends beneficial signals to your brain. Similarly, managing stress and optimizing mental health through practices like meditation, therapy, or exercise can improve your gut function and microbiota composition.
The Gut-Brain Connection in Health and Disease
Understanding the gut-brain axis has profound implications for how we approach health and disease treatment. Traditional medicine often treats the brain and digestive system as separate systems, but emerging research reveals they are fundamentally interconnected. This understanding opens new therapeutic possibilities for conditions that were previously considered purely neurological or purely gastrointestinal.
Conditions linked to the gut-brain axis include anxiety disorders, depression, irritable bowel syndrome, inflammatory bowel disease, neurodegenerative diseases like Parkinson’s disease, post-traumatic stress disorder, and even long-COVID syndrome neurological symptoms. This broader understanding suggests that treatment strategies should consider both the brain and the gut, addressing the root causes of dysfunction rather than treating symptoms in isolation.
Optimizing Your Gut-Brain Connection
Given the profound influence of the gut-brain axis on your health, optimizing this connection should be a priority. Several evidence-based strategies can support a healthy gut-brain relationship.
Dietary Approaches:
- Increase fiber intake to promote short-chain fatty acid production
- Include omega-3 fatty acids from sources like fatty fish and flaxseeds
- Consume fermented foods such as yogurt, kefir, sauerkraut, and kimchi
- Add polyphenol-rich foods like berries, green tea, and colorful vegetables
- Consider probiotic-rich foods or supplements to support microbial diversity
Lifestyle Approaches:
- Practice stress-reduction techniques like meditation, deep breathing, or yoga
- Maintain regular physical activity, which supports both brain and gut health
- Ensure adequate sleep, crucial for both neurological and digestive function
- Limit alcohol consumption, which can damage the gut barrier and microbiota
- Reduce processed foods and artificial additives that disrupt microbiota composition
Frequently Asked Questions
Q: How quickly can changes to my diet affect my gut-brain connection?
A: Research suggests that changes in diet can begin affecting your microbiota composition within days to weeks. However, more substantial improvements in mood and cognitive function typically require 4-8 weeks of consistent dietary changes as your microbiota adapts and establishes new patterns.
Q: Can stress really cause digestive problems?
A: Yes, absolutely. Stress activates your brain’s emotional centers, which directly control digestive functions through the vagus nerve. This is why stress can cause symptoms like stomach upset, diarrhea, constipation, or reduced appetite. The connection between stress and ulcers demonstrates this relationship at the physiological level.
Q: Are probiotics effective for mental health?
A: Research on psychobiotics (probiotics that affect mental health) is promising but still emerging. While certain probiotic strains have shown benefits for anxiety and depression in some studies, results are not universal. The best approach is to support overall microbiota health through diverse fiber intake and fermented foods rather than relying solely on supplements.
Q: How does the blood-brain barrier relate to the gut-brain axis?
A: The blood-brain barrier is a selective filter that protects your brain from harmful substances. Short-chain fatty acids produced by your gut microbiota, particularly butyrate, help maintain the integrity of this barrier. When your microbiota is unhealthy, barrier function can deteriorate, potentially allowing harmful substances to reach your brain.
Q: Can improving my gut health help treat anxiety or depression?
A: While gut health optimization should not replace professional mental health treatment, it can be a valuable complementary approach. Since the gut produces neurotransmitters like serotonin and GABA that affect mood, improving microbiota health through diet, probiotics, and lifestyle changes may support mental health outcomes when combined with other evidence-based treatments.
Q: What is dysbiosis and how does it affect the brain?
A: Dysbiosis is an imbalance in your gut microbiota composition, often characterized by reduced microbial diversity or an overgrowth of harmful bacteria. Dysbiosis can impair the production of beneficial neurotransmitters and short-chain fatty acids, increase gut inflammation, and trigger systemic inflammation that reaches the brain, potentially worsening mood, cognition, and stress responses.
References
- Gut–brain axis and neuropsychiatric health: recent advances — Nature Scientific Reports. 2025-01-15. https://www.nature.com/articles/s41598-025-86858-3
- The Gut-Brain Connection: How it Works and The Role of Nutrition — Healthline. 2024. https://www.healthline.com/nutrition/gut-brain-connection
- The gut-brain connection — Mental Health America. 2024. https://mhanational.org/resources/gut-brain-connection/
- What Is the Gut-Brain Connection? — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/body/the-gut-brain-connection
- Rat Research Suggests How the Brain and Gut Are Connected — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024. https://www.nccih.nih.gov/research/research-results/rat-research-suggests-how-the-brain-and-gut-are-connected-points-to-stressulcer-link
- Gut-Brain Communication — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024. https://www.nccih.nih.gov/training/videolectures/20/2
- What is the gut-brain connection activity? — Guts UK. 2024-07-01. https://gutscharity.org.uk/2024/07/what-is-the-gut-brain-connection-activity/
Read full bio of medha deb