Acid Reflux & GERD: Symptoms, Causes, and Treatment
Comprehensive guide to understanding GERD, its symptoms, causes, and effective treatment options.
Understanding Acid Reflux and GERD
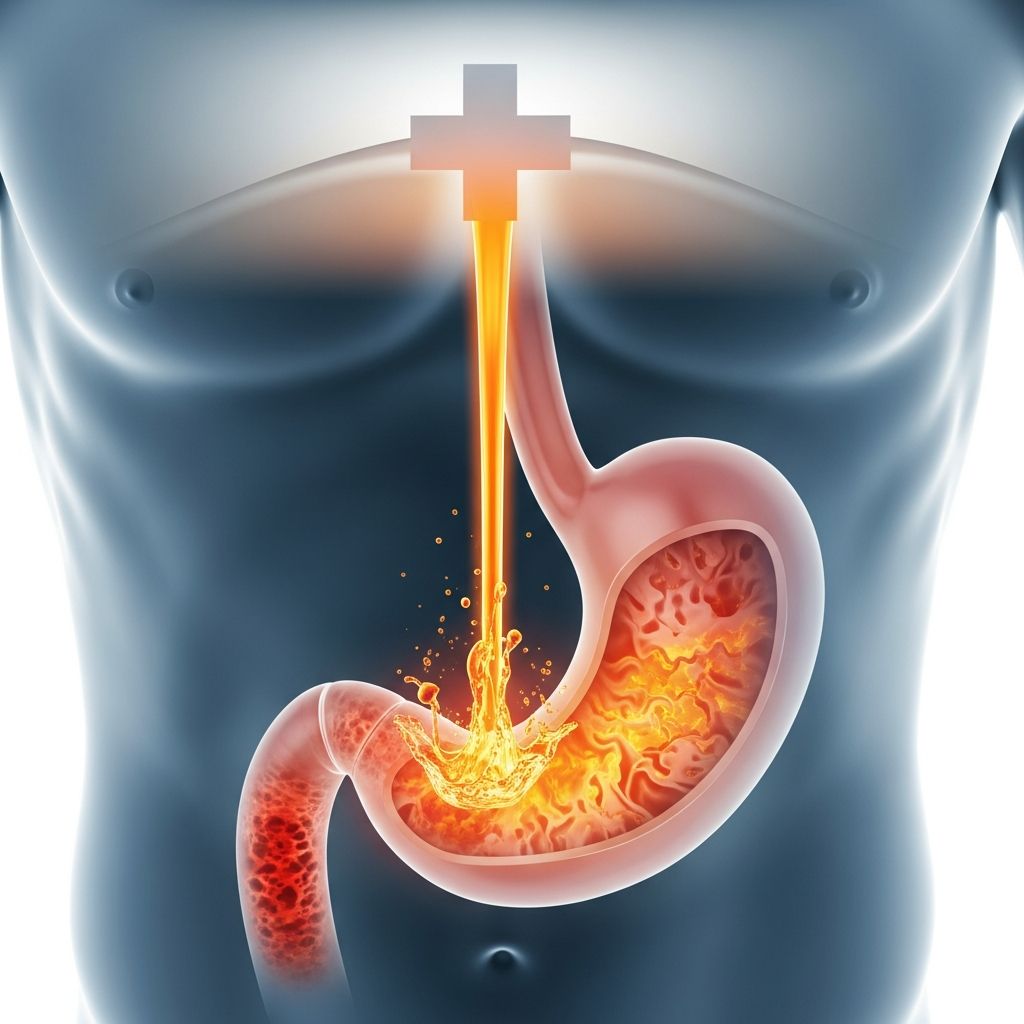
Acid reflux occurs when stomach acid rises into your esophagus, causing a sensation of heartburn and other uncomfortable symptoms. This happens when the valve at the bottom of your esophagus, called the lower esophageal sphincter (LES), opens when it shouldn’t. When this occurs, the contents of your stomach—including acid, digestive juices, and food—begin moving backward into your esophagus, causing irritation and discomfort.
It’s important to understand that acid reflux and heartburn are not the same thing. Heartburn is a symptom of acid reflux, specifically the burning sensation you feel in your chest. Most people can experience up to an hour of reflux per day without even noticing it. However, when reflux becomes problematic and occurs frequently, it can cause noticeable heartburn and other symptoms.
GERD stands for gastroesophageal reflux disease (sometimes spelled GORD for gastro-oesophageal reflux disease). This is a chronic condition where you experience consistent acid reflux with intensified symptoms. Acid reflux is considered chronic when you’ve had it at least twice a week for several weeks. GERD represents a more severe form of acid reflux, where the persistent backflow of stomach acid can lead to inflammation, irritation, and even damage to your esophagus lining.
Common Symptoms of Acid Reflux and GERD
Acid reflux can manifest in various ways. The most common symptom is heartburn, which is characterized by a burning sensation in your chest that may extend to your throat. You might also experience a sour or acidic taste in your mouth. Additionally, GERD can cause other symptoms including:
- A feeling of a lump in the back of your throat
- Chronic cough
- Difficulty swallowing
- Regurgitation of food or liquids
- Hoarseness or throat irritation
In some cases, acid reflux mostly affects your esophagus, though sometimes it can extend into your windpipe or even your airways. A small amount of acid may cause only momentary discomfort, but larger quantities can injure these sensitive organs and lead to more serious complications.
What Causes Acid Reflux and GERD?
Several factors can contribute to the development of acid reflux and GERD. Understanding these causes can help you manage your condition more effectively.
Contributing Factors
Low pressure in the lower esophageal sphincter is a primary cause of acid reflux. Additionally, poor mixing of acid with food material in the proximal stomach can create concentrated acid pockets that are more likely to reflux. Increased gastroesophageal junction distensibility allows stomach contents to move more easily into the esophagus. Obesity significantly increases the risk of GERD, as excess weight puts additional pressure on the stomach. Delayed gastric emptying, where food stays in your stomach longer than it should, can also contribute to reflux symptoms.
Lifestyle Triggers
Certain lifestyle habits and foods can trigger acid reflux. Large, rich meals are common culprits, as are fatty or fried foods. Spicy dishes, acidic fruits, and beverages like alcohol and caffeine can all worsen symptoms. Eating too close to bedtime or lying down immediately after eating often triggers reflux. Additionally, tobacco use and excessive alcohol consumption can weaken the LES and increase acid production.
When to Seek Medical Attention
While occasional heartburn is manageable at home, chronic acid reflux requires professional evaluation. If you find that your symptoms of heartburn start to worsen and you begin to notice additional symptoms, you should talk to a healthcare provider. A gastroenterologist will evaluate your esophagus to diagnose GERD and determine the appropriate treatment plan.
Diagnosis of GERD
GERD is mainly a clinical diagnosis based on typical symptoms of heartburn and acid regurgitation. However, if your symptoms persist or if your healthcare provider suspects complications, several diagnostic tests may be recommended:
Diagnostic Tests
- Upper Endoscopy: A thin, flexible tube with a camera is passed down your esophagus to visualize any damage or inflammation. Biopsies may be taken to rule out other conditions such as eosinophilic esophagitis.
- pH Testing: This test measures the acid exposure in your esophagus over a 24 to 48-hour period, confirming whether abnormal acid reflux is occurring.
- pH and Impedance Testing: This advanced test detects all types of reflux, including acidic, weakly acidic, and weakly alkaline secretions.
- High-Resolution Manometry: This test measures the pressure in your esophagus and the function of your LES.
Current guidelines indicate that patients with typical symptoms should first try a proton pump inhibitor (PPI). If reflux symptoms persist after 8 weeks on a PPI, endoscopy of the esophagus is recommended, with biopsies taken to rule out eosinophilic esophagitis and other conditions.
Treatment Options for Acid Reflux and GERD
Treatment approaches vary depending on the severity of your condition. Occasional acid reflux is often manageable with lifestyle changes and over-the-counter medications, while chronic GERD typically requires professional medical management.
Lifestyle Modifications
Many people find they can reduce acid reflux with lifestyle adjustments. Healthcare providers encourage this approach as a first-line treatment. Key lifestyle changes include:
- Changing eating habits to avoid trigger foods
- Eating smaller, more frequent meals
- Reducing or eliminating alcohol consumption
- Quitting tobacco use
- Losing weight if overweight
- Elevating your head while sleeping
- Waiting at least three hours after eating before lying down
Over-the-Counter Medications
Several OTC medicines can provide relief for acid reflux symptoms:
- Antacids: These neutralize stomach acid quickly and provide rapid relief.
- H2 Blockers: These reduce acid production in the stomach.
- Proton Pump Inhibitors (PPIs): These are very effective at reducing stomach acid production.
Prescription Medications
For chronic GERD, healthcare providers recommend medicines to reduce your stomach acid, so reflux is less damaging. These medicines are easily available and highly effective for GERD. Prescription options include stronger formulations of PPIs and other acid-reducing medications that work by different mechanisms. An 8-week course of therapy is typically needed to allow for healing, and patients should not be considered as not responding to treatment until after this period.
Surgical and Procedural Treatments
While medicine can reduce the symptoms and the effects of GERD, it doesn’t stop the condition from happening. A severe case of GERD may continue to cause complications despite medication. When this occurs, a more definitive treatment may be needed, usually involving a procedure to tighten your LES. These are minor, outpatient procedures that are very effective. In rare cases, more extensive surgery may be recommended, particularly for patients with severe erosive esophagitis or large hiatal hernia.
Complications of Untreated GERD
Long-term, untreated GERD can cause serious complications. Persistent backflow of stomach acid can lead to inflammation and ulcers in the esophagus, a condition called reflux esophagitis. Over time, this can damage your esophagus tissues. In some cases, chronic GERD can increase the risk of esophageal cancer. Additionally, GERD can cause extraesophageal symptoms such as chronic cough, asthma-like symptoms, laryngitis, and voice changes. These complications emphasize the importance of proper diagnosis and treatment.
GERD Management and Ongoing Care
Managing GERD is an ongoing process that may require adjustments over time. If you have symptoms that don’t respond well to initial treatment, your healthcare provider may recommend additional testing. For patients with partial or no relief from PPI therapy, pH testing to detect acid reflux should be performed off PPI therapy. In patients with objective evidence of GERD who have refractory symptoms, pH impedance testing on PPI may be performed to detect the amount of reflux, whether acidic, weakly acidic, or nonacidic.
If results of pH and impedance testing are normal, the most common causes of continued symptoms are reflux hypersensitivity and functional heartburn. Reflux hypersensitivity is a heightened response to nonpathologic reflux, while functional heartburn is the presence of symptoms without any evidence of abnormal acid exposure. Patients with these conditions should be reassured that their condition is benign, and they may be started on a pain modulator such as a selective serotonin reuptake inhibitor or tricyclic antidepressant.
Frequently Asked Questions About Acid Reflux and GERD
Q: What’s the difference between heartburn and GERD?
A: Heartburn is a symptom—the burning sensation you feel. Acid reflux is the actual condition where stomach acid moves backward into your esophagus. GERD is when acid reflux becomes chronic, occurring at least twice a week for several weeks, and causes more serious symptoms and potential damage to your esophagus.
Q: Can acid reflux go away on its own?
A: Occasional acid reflux can resolve with lifestyle changes and over-the-counter treatments. However, chronic acid reflux (GERD) typically requires ongoing management through medication and lifestyle modifications. Some severe cases may need procedural intervention.
Q: How long does it take for GERD treatment to work?
A: An 8-week course of therapy is typically needed to allow for healing when taking prescription medications like PPIs. You should not consider yourself a non-responder until after this period, unless you have alarm symptoms.
Q: Is GERD dangerous?
A: While occasional heartburn is uncomfortable but not dangerous, untreated chronic GERD can cause serious complications including inflammation and ulcers of the esophagus, increased risk of esophageal cancer, and extraesophageal symptoms. Proper treatment and management are important to prevent these complications.
Q: Can weight loss help with GERD?
A: Yes, losing weight if you’re overweight can significantly reduce GERD symptoms. Obesity increases pressure on the stomach and weakens the lower esophageal sphincter, contributing to reflux. Weight loss is one of the most effective lifestyle modifications for managing acid reflux.
Q: Should I stop taking PPIs?
A: You should not stop taking prescribed PPIs without consulting your healthcare provider. While long-term PPI therapy has some considerations, they are highly effective for GERD management. Your doctor will help you determine the appropriate duration and dosage for your specific situation.
References
- Acid Reflux & GERD: Symptoms, What It Is, Causes, Treatment — Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd
- Heartburn, Acid Reflux and GERD Differences — Cleveland Clinic Health. https://health.clevelandclinic.org/whats-the-difference-between-heartburn-acid-reflux-and-gerd
- GERD: A practical approach — Cleveland Clinic Journal of Medicine, 2020. https://www.ccjm.org/content/87/4/223
- Evaluation and management of gastroesophageal reflux disease — Cleveland Clinic Journal of Medicine. https://www.ccjm.org/content/89/12/700
- Why GERD Can Often Go Undiagnosed — Cleveland Clinic Newsroom, November 2025. https://newsroom.clevelandclinic.org/2025/11/24/why-gerd-can-often-go-undiagnosed
- 6 Lifestyle Remedies for Acid Reflux Relief — Cleveland Clinic Health. https://health.clevelandclinic.org/heartburn-lifestyle-changes-to-reduce-acid-reflux-symptoms
- GERD Diet: Foods To Eat and Avoid — Cleveland Clinic Health. https://health.clevelandclinic.org/gerd-diet
Read full bio of medha deb











