Allergy Treatment Options: Evidence-Based Guide
Comprehensive guide to modern allergy treatments, from avoidance to immunotherapy and emerging therapies for lasting relief.

Allergy Treatment Options: From Avoidance to Advanced Therapies
Allergies affect millions worldwide, triggering symptoms from sneezing and itching to life-threatening anaphylaxis. Effective treatment begins with identifying triggers through testing and progresses to layered strategies including medications, immunotherapy, and emerging biologics. This guide covers all major approaches, emphasizing evidence-based options for seasonal, food, skin, and respiratory allergies.
Avoidance Measures: The First Line of Defense
The cornerstone of allergy management is minimizing exposure to allergens. While complete avoidance isn’t always feasible, targeted strategies significantly reduce symptom severity.
- For pollen allergies: Stay indoors during high pollen counts (typically midday), use HEPA air filters, and shower after outdoor exposure to remove pollen from skin and hair.
- For dust mites: Encase mattresses in allergen-proof covers, wash bedding weekly in hot water (>130°F), and maintain indoor humidity below 50%.
- For pet dander: Keep pets out of bedrooms, use HEPA vacuums, and consider allergen-reducing shampoos.
- For food allergies: Strict label reading, carrying epinephrine auto-injectors, and creating allergy action plans with healthcare providers.
These measures, when combined with medical therapy, can reduce reliance on medications by up to 50% in many patients.
Over-the-Counter Medications
OTC options provide rapid symptom relief for mild to moderate allergies. Key categories include:
| Medication Type | Examples | Best For | Common Side Effects |
|---|---|---|---|
| Antihistamines (2nd/3rd gen) | Loratadine (Claritin), Cetirizine (Zyrtec), Fexofenadine (Allegra) | Sneezing, itching, runny nose | Drowsiness (minimal), dry mouth |
| Nasal saline rinses | Neti pot, saline sprays | Nasal congestion | None |
| Decongestants | Pseudoephedrine (Sudafed) | Stuffy nose (short-term use) | Increased blood pressure, insomnia |
| Eye drops | Ketorolac, Naphazoline | Itchy, watery eyes | Rebound redness with overuse |
Second-generation antihistamines are preferred due to lower sedation risk compared to first-generation options like diphenhydramine.
Prescription Medications
For persistent symptoms, prescription therapies offer targeted relief:
- Intranasal corticosteroids: Fluticasone (Flonase), Budesonide (Rhinocort)—gold standard for allergic rhinitis, reducing inflammation for 24-hour control.
- Montelukast (Singulair): Leukotriene inhibitor effective for asthma-allergy overlap; recent FDA warning notes rare neuropsychiatric side effects.
- Intranasal antihistamines: Azelastine—faster onset than steroids for acute symptoms.
- Combination therapies: Fluticasone-furoate/vilanterol for severe cases.
Guidelines from the American Academy of Allergy, Asthma & Immunology recommend starting with intranasal steroids for moderate-persistent rhinitis.
Immunotherapy: Building Long-Term Tolerance
Allergen immunotherapy (AIT) modifies the immune response, providing durable relief often lasting years post-treatment. Four main forms exist for allergies.
Subcutaneous Immunotherapy (SCIT)
Injections of gradually increasing allergen doses administered weekly then monthly. Highly effective for pollen, dust mites, and pet allergies (70-80% symptom reduction). Risks include systemic reactions; performed in medical settings.
Oral Immunotherapy (OIT)
FDA-approved Palforzia (peanut powder) for ages 4-17 desensitizes to peanut exposure. Involves daily dosing with up-dosing phases. Nearly 70% tolerate 600mg peanut protein post-treatment. Best for peanut allergy; ongoing research for tree nuts, milk.
Sublingual Immunotherapy (SLIT)
Tablets or drops under the tongue (e.g., Odactra for dust mites, Oralair for grass pollen). Safer profile than SCIT with fewer systemic reactions. FDA-approved options show 30-40% symptom improvement.
Epicutaneous Immunotherapy (EPIT)
Viaskin Peanut patch delivers allergen through intact skin. Phase 3 trials show promise for young children; minimal side effects like mild itching.
Immunotherapy protocols typically span 3-5 years, with maintenance phases promoting sustained tolerance.
Biologics and Monoclonal Antibodies
Targeted therapies revolutionize severe allergy management:
- Omalizumab (Xolair): Anti-IgE monoclonal antibody FDA-approved for chronic hives and allergic asthma. Adjunct to OIT reduces reactions; ongoing trials for multi-food allergies.
- Dupilumab (Dupixent): IL-4/IL-13 inhibitor for eczema and asthma with nasal polyps.
- Tezepelumab: Emerging TSLP blocker for broad allergic pathways.
These require injections every 2-4 weeks; costs $3,000+/month but covered for qualifying conditions. Omalizumab + OIT trials show 80% success in reaching maintenance doses.
Treatment for Specific Allergy Types
Seasonal Allergic Rhinitis (Hay Fever)
Combine avoidance, intranasal steroids, and second-line antihistamines. SLIT tablets offer season-long protection.
Food Allergies
OIT leads; epinephrine remains emergency cornerstone. Emerging: monoclonal antibodies for broad desensitization.
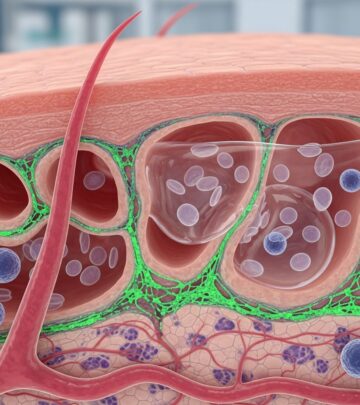
Skin Allergies (Hives, Eczema)
Topical steroids, calcineurin inhibitors, biologics for refractory cases.
Insect Sting Allergies
SCIT highly effective (95% protection post-treatment).
Emerging and Experimental Therapies
- DNA vaccines and nanoparticle delivery for precise immune modulation.
- Microbiome therapies targeting gut-allergy axis.
- Chinese herbal formulations like FAHF-2 showing preclinical promise.
Clinical trials emphasize personalized medicine based on biomarkers.
Lifestyle and Complementary Approaches
- Probiotics may reduce eczema risk in at-risk infants (Cochrane review).
- Acupuncture shows modest rhinitis benefits.
- Butterbur and quercetin as natural antihistamines (limited evidence).
Always consult providers before alternatives.
Frequently Asked Questions (FAQs)
What is the most effective allergy treatment?
Immunotherapy provides longest-lasting relief; medications control symptoms short-term.
Is allergy immunotherapy safe for children?
Yes, with proper monitoring; OIT approved for ages 4+, SLIT for 5+.
How long does immunotherapy take?
3-5 years for full course, with benefits persisting post-treatment.
Can allergies be cured?
Not always, but immunotherapy achieves tolerance in 70-90% of cases.
What if OTC meds don’t work?
See an allergist for prescriptions, testing, or immunotherapy referral.
Choosing the Right Treatment Plan
Personalized plans consider allergy type, severity, age, and comorbidities. Start with primary care, escalate to specialists. Track symptoms via apps for optimization. Regular follow-ups ensure efficacy and safety.
Advancements like FDA-approved OIT mark progress, but research continues for broader cures.
References
- New and emerging concepts and therapies for the treatment of food allergies — Kim EH, et al. PMC. 2022-04-01. https://pmc.ncbi.nlm.nih.gov/articles/PMC9007422/
- Guidelines for the Diagnosis and Management of Food Allergy in the United States — NIAID. 2010 (updated 2024 review). https://www.niaid.nih.gov/diseases-conditions/food-allergy
- Allergen Immunotherapy: A Practice Parameter Third Update — Cox L, et al. Journal of Allergy and Clinical Immunology. 2011-01. https://doi.org/10.1016/j.jaci.2010.09.149
- Omalizumab for Food Allergy — Wood RA, et al. New England Journal of Medicine. 2020-08-20. https://www.nejm.org/doi/full/10.1056/NEJMoa1912680
- Palforzia (peanut allergen powder-dnfp) FDA Approval — FDA. 2020-01-31. https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-treatment-peanut-allergy
Read full bio of medha deb