Amputation Stump Dermatoses: Causes, Types, and Management
Understanding skin diseases affecting amputation stumps and effective prevention strategies.
What Are Amputation Stump Dermatoses?
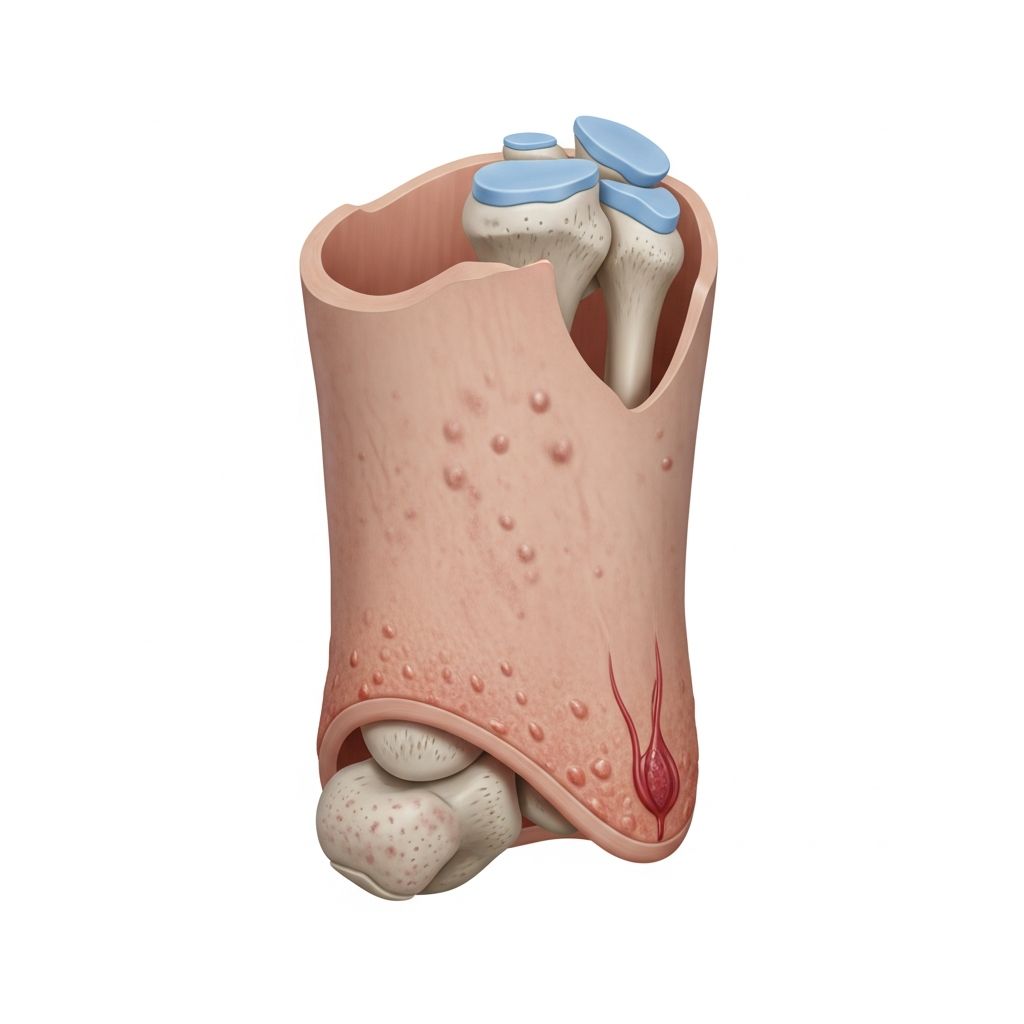
Amputation stump dermatoses are skin diseases that develop on the stump following the amputation of a limb. These conditions, also called amputation-related dermatoses, can emerge immediately after surgery or may not manifest until many years later. The stump skin undergoes significant physiological changes after amputation, making it particularly vulnerable to various dermatological complications that can substantially impact the quality of life for amputees.
Stump dermatoses are reported to affect between 34–74% of amputees, with prevalence varying according to study design, population samples, and assessment methods employed. Research demonstrates that skin problems tend to persist long-term, as documented in war veterans experiencing complications 38 years after amputation. Among these conditions, pressure ulcers and skin breakdown account for 39% of cases, while infections represent 25% of reported dermatoses, with up to one quarter of amputees affected more than 50% of the time.
Factors Contributing to Stump Vulnerability
The skin of an amputation stump is fundamentally different from intact skin and is not naturally designed to withstand the physical insults encountered within a prosthetic device. Several interconnected factors increase the stump’s vulnerability to dermatological disease:
- Prosthetic use: Although dermatoses may arise before prosthesis fitting, the primary contributing factors are the degree of activity and use of a prosthesis, which creates friction, pressure, and occlusion against the delicate stump skin
- Physical trauma: Repeated frictional forces, pressure points, and mechanical irritation from the prosthetic socket compromise skin integrity
- Reduced sensation: Altered or absent sensory nerve function prevents the patient from recognizing early warning signs of skin damage
- Compromised circulation: Peripheral vascular disease and circulatory impairment affect wound healing capacity and nutrient delivery to stump tissues
- Moisture retention: Occlusion within the prosthetic socket creates a warm, moist environment conducive to bacterial and fungal growth
- Underlying conditions: Diabetes mellitus, vasculitis, and other systemic diseases significantly increase susceptibility to protracted skin problems
Common Types of Amputation Stump Dermatoses
Amputation stump skin diseases manifest in diverse forms, each requiring specific management approaches. The most frequently encountered dermatological conditions include:
Pressure-Related Disorders
- Pressure ulcers: Result from chronic pressure or repeated frictional forces on stump skin, particularly over bony prominences
- Callosities: Thickened skin areas developing in response to repeated pressure, occurring in approximately 18.3% of amputees
- Corns: Localized hyperkeratotic lesions forming on areas of concentrated pressure
- Lichenification: Thickening and hardening of the skin surface, documented in approximately 10.9% of cases
Infectious Complications
- Bacterial infections: Include furuncles, boils, and cellulitis resulting from compromised skin integrity and poor hygiene, affecting 10.3% of amputees
- Fungal infections: Dermatophytic infections occur due to warm, moist conditions within the prosthetic socket, present in 2.9% of documented cases
- Folliculitis: Inflammation of hair follicles caused by shaving, friction, or sweat accumulation
Pigmentation Changes
- Hyperpigmentation: The most common dermatological change, affecting 26.4% of amputees, characterized by increased skin darkening at the stump
- Hypopigmentation: Loss of skin pigmentation affecting approximately 7.4% of cases
Inflammatory and Traumatic Conditions
- Scaling: Abnormal skin shedding present in 16.7% of amputees, often associated with dryness and irritation
- Cutaneous atrophy: Thinning of the epidermis and dermis occurring in 11.5% of cases due to prolonged pressure or poor circulation
- Traumatic ulcers: Lesions resulting from physical injury to the stump skin, documented in 10.3% of amputees
- Hypertrophic scars: Excessive scar tissue formation at the amputation site, affecting 8.1% of patients
- Frictional eczema: Inflammatory skin reaction to friction, present in 1.1% of documented cases
- Intertriginous dermatitis: Inflammation in skin fold areas caused by moisture and friction, affecting 1.7% of amputees
Rare and Unusual Presentations
- Verrucous hypertrophy: Warty overgrowth of stump tissue occurring in 6.9% of cases
- Allergic contact dermatitis: Reactions to prosthetic materials such as resins, documented in 1.1% of amputees
- Stump edema: Swelling of the residual limb affecting tissue function and skin health in 2.3% of cases
- Phantom limb sensations: Neurological phenomena occurring in 2.3% of amputees
- Keloid formation, cutaneous horns, epidermoid cysts, and gangrene: Rare complications each affecting less than 1% of amputees
Risk Factors for Stump Dermatoses
Multiple factors independently and collectively increase the likelihood of developing amputation stump skin diseases. Research has identified specific variables associated with heightened dermatological risk:
| Risk Factor | Impact |
|---|---|
| Transtibial amputation | Lower leg amputations carry greater dermatological risk due to weight-bearing demands |
| Employment status | Working amputees experience increased prosthesis use and associated skin complications |
| Type of walking aid used | Specific prosthetic designs and socket materials affect skin compatibility |
| Peripheral vascular disease | Compromises wound healing and tissue nutrition |
| Smoking | Impairs circulation and wound healing capacity |
| Younger age | Associated with higher activity levels and prosthesis use intensity |
| Female sex | Increased incidence of skin problems in female amputees |
| Frequent stump washing | Can strip natural skin oils and increase irritation |
| Antibacterial soap use | May disrupt normal skin flora balance |
| Diabetes mellitus | Associated with impaired wound healing, infection susceptibility, abnormal sensation, and fluid balance disruption |
| Traumatic amputation cause | Patients from traumatic amputations show higher dermatological complication rates |
Impact on Quality of Life
Amputation stump dermatoses create significant adverse effects extending beyond physical health. The psychological, emotional, and social consequences substantially diminish wellbeing and quality of life for affected individuals. Chronic skin problems can necessitate extended periods without prosthesis use, leading to social isolation, emotional distress, reduced employment opportunities, and financial hardship. In severe cases, untreated skin complications can prevent prosthesis use entirely, fundamentally limiting mobility and independence. The persistent nature of these conditions—often lasting decades—compounds their cumulative psychological impact on amputees adapting to limb loss.
Prevention and Management Strategies
Daily Stump Care Practices
Effective prevention of amputation stump dermatoses begins with consistent daily care protocols designed to maintain skin integrity and prevent complications:
- Daily inspection: Check the amputation stump thoroughly each day, examining all surfaces for signs of irritation, redness, breakdown, or infection
- Proper cleaning: Wash the stump regularly with mild soap and lukewarm water, ensuring thorough drying afterward
- Moisture management: Change damp socks promptly and ensure complete drying before applying prosthesis, as moisture creates environments favorable for infection
- Protective measures: Shield bony prominences and pressure-sensitive areas from direct trauma and friction
- Avoid irritants: Do not use alcohol-based cleansing products or perfumes that can cause skin drying and cracking
- Minimize shaving: Avoid shaving the stump when possible, as this creates microtrauma and new scar formation
- Socket hygiene: Wash the prosthetic socket regularly and allow it to dry completely before use
Desensitization and Stump Conditioning
Desensitization procedures are performed to eliminate or minimize physical and psychological responses to stimuli during the early post-amputation period. These techniques include gentle massage, light tapping, vibration, constant pressure application, and introduction of various fabric textures to the sensitive stump area. After complete healing, active massage therapy is recommended to prevent skin adhesion and enhance sensory transmission. Research demonstrates that desensitization is significantly effective, with 85% of patients reporting improved pain control after amputation surgery. Although recommended twice to three times daily for at least five minutes, standardized guidelines for desensitization progression remain limited.
Stump Shrinkage and Shaping
Shrinkage and shaping represent the most important components of rehabilitation prior to prosthesis fitting, as improper management can impair blood circulation and wound healing. Four primary methods include application of soft, semi-rigid, or rigid dressings, along with fitting of temporary prostheses. These interventions reduce stump volume fluctuations and facilitate proper prosthetic socket fitting.
Edema Management
Edema management requires particular attention, as untreated swelling can progress to discoloration, blisters, and ulceration. Management strategies include stretching exercises, elastic bandage compression, pneumatic or cooling compression systems, lymphatic massage, and high-voltage pulsed current application. In severe cases, anti-inflammatory medications or corticosteroid injections may be necessary. Temperature control of the stump, bandage, and socket is essential, as heat exacerbates edema.
Infection Treatment and Prevention
Bacterial infections typically respond to local cleaning combined with topical antibiotics, though severe cases may require dead skin removal and oral antibiotics. The prosthesis should remain unworn until skin infection resolves completely. Fungal infections are treated with over-the-counter antifungal creams. Preventive measures include regular skin and socket washing, proper sock drying, avoidance of alcohol-based cleansers, and maintaining appropriate stump temperature and humidity.
Advanced Treatment Options
Vacuum-assisted socket suspension systems represent innovative technology for managing wounds and ulcers on residual limbs. These systems prevent daily stump volume loss occurring with conventional sockets and minimize skin irritation by reducing shear stress during prosthesis use.
Frequently Asked Questions
Q: What percentage of amputees develop stump dermatoses?
A: Research indicates that stump dermatoses affect between 34–74% of amputees, with prevalence varying based on study methodology, population samples, and assessment techniques.
Q: When can amputation stump dermatoses develop?
A: These conditions can emerge immediately following amputation surgery or may not manifest until many years later, with complications documented decades after initial amputation.
Q: Which dermatoses are most common in amputees?
A: Hyperpigmentation is the most common condition affecting 26.4% of amputees, followed by callosities (18.3%), scaling (16.7%), and cutaneous atrophy (11.5%).
Q: Can stump dermatoses be prevented?
A: While some skin problems are inevitable due to prosthetic use, many complications can be prevented through consistent daily care, proper hygiene, regular inspection, prosthesis adjustment, and prompt medical intervention.
Q: Why is diabetes particularly problematic for amputees?
A: Diabetes mellitus is strongly associated with protracted skin problems due to impaired wound healing, increased infection susceptibility, abnormal sensory nerve function, and disruption of normal tissue fluid balance, requiring more frequent clinical review.
Q: How often should the amputation stump be inspected?
A: Daily inspection of the amputation stump is essential to identify early signs of skin damage, irritation, infection, or breakdown before complications become severe.
Q: What is the most effective approach to prevent stump skin infections?
A: Prevention involves regular cleaning and drying of both the stump and prosthetic socket, changing damp socks promptly, maintaining appropriate temperature and humidity levels, avoiding alcohol-based products, and preventing shaving-related trauma.
Conclusion
Amputation stump dermatoses represent significant complications affecting a substantial proportion of amputees worldwide. These diverse skin conditions range from common pressure-related disorders and infections to rare presentations including keloid formation and cutaneous horns. The development of stump dermatoses depends on multiple interacting factors including prosthesis type and use, underlying systemic diseases, and individual risk factors. Preventing and managing these conditions requires comprehensive daily care protocols, professional desensitization and conditioning procedures, proper edema management, and prompt treatment of infections and other complications. By implementing consistent preventive strategies and seeking early medical intervention for emerging problems, amputees can substantially reduce the incidence and severity of stump dermatoses, thereby improving functional outcomes, maintaining prosthesis use, and enhancing overall quality of life following limb loss.
References
- Dermatological changes of amputation stump — Indian Journal of Dermatology, Venereology, and Leprology. 2023. https://ijdvl.com/dermatological-changes-of-amputation-stump/
- Amputation stump management: A narrative review — PubMed Central (PMC). 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC9131228/
- Amputation stump dermatoses — DermNet NZ. 2024. https://dermnetnz.org/topics/amputation-stump-dermatoses
- Skin Problems in Amputees — Plastic Surgery Key. 2024. https://plasticsurgerykey.com/skin-problems-in-amputees/
- Skin Care of the Residual Limb — MSD Manuals. 2024. https://www.msdmanuals.com/home/special-subjects/limb-prosthetics/skin-care-of-the-residual-limb
Read full bio of medha deb