Are Sunstroke and Heatstroke the Same?
Discover the key differences between sunstroke and heatstroke and learn how to prevent heat-related illnesses.
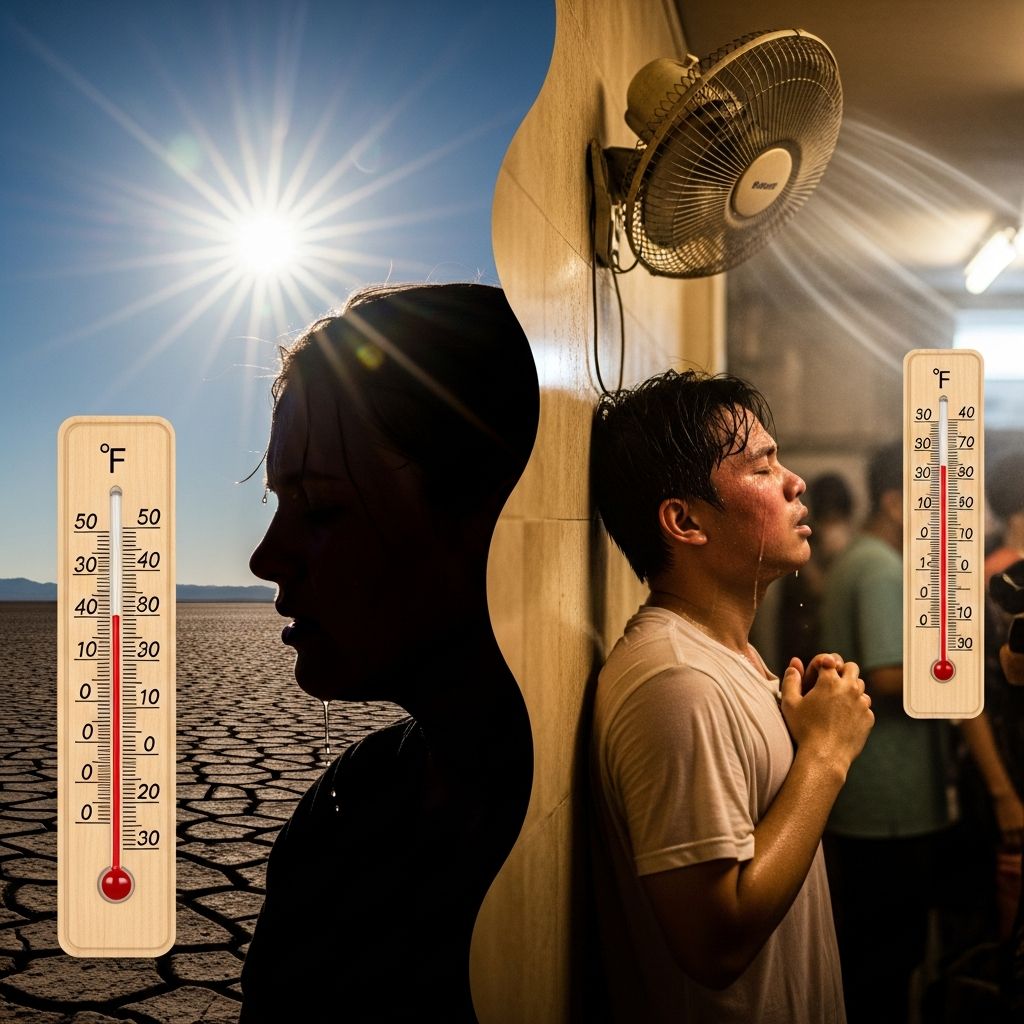
When temperatures soar during summer months, heat-related illnesses become a significant health concern. Many people use the terms “sunstroke” and “heatstroke” interchangeably, but understanding whether these conditions are truly the same is crucial for proper prevention and treatment. The answer is more nuanced than a simple yes or no, and recognizing the distinctions can literally save lives.
Understanding the Terminology
Sunstroke and heatstroke are often used synonymously in everyday conversation, and for practical purposes, they refer to the same dangerous medical emergency. Heat stroke, also commonly called sunstroke, is a life-threatening condition that occurs when core body temperature exceeds 104°F (40°C) accompanied by central nervous system dysfunction. The terms are essentially interchangeable because both describe the same physiological breakdown of the body’s temperature regulation system.
However, the terminology distinction can sometimes reflect the cause of the condition. Sunstroke may emphasize exposure to direct sunlight, while heatstroke is a broader term encompassing any scenario where the body’s cooling mechanisms fail. Regardless of terminology, the medical urgency and treatment approach remain identical.
Heat-Related Illness Progression
To fully understand whether sunstroke and heatstroke are the same, it’s important to recognize that heat-related illnesses exist on a spectrum. The progression typically begins with heat exhaustion and can escalate to heat stroke if not properly managed.
Heat Exhaustion: The Warning Stage
Heat exhaustion represents the body’s struggle to maintain proper temperature regulation through sweating and blood flow redistribution. During this stage, prolonged exposure to high temperatures causes significant water and salt loss through sweating, leading to dehydration and circulatory strain. The body’s cooling mechanisms—especially sweating and blood flow to the skin—still function but become overwhelmed by excessive heat exposure.
Common symptoms of heat exhaustion include:
- Profuse sweating and pale, clammy skin
- Weakness or dizziness
- Headache and muscle cramps
- Nausea, vomiting, or fainting
- Rapid, shallow breathing
- Weak but fast pulse
These symptoms develop gradually after prolonged heat exposure, such as working outdoors, exercising in hot weather, or staying in poorly ventilated areas. Critically, if heat exhaustion is not recognized and treated quickly, the condition can rapidly progress to heat stroke.
Heat Stroke: The Medical Emergency
Heat stroke, whether called sunstroke or heatstroke, represents a complete failure of the body’s thermoregulatory system. At this stage, core body temperature exceeds 104°F (40°C), and the central nervous system becomes severely compromised. The body stops sweating as the cooling mechanism collapses entirely, and internal heat builds up uncontrollably, potentially damaging the brain, heart, kidneys, and muscles.
Typical symptoms of heat stroke include:
- Extremely high body temperature (above 104°F)
- Hot, red, and dry skin (no sweating)
- Rapid, strong pulse
- Confusion, slurred speech, or loss of consciousness
- Seizures or delirium
- Nausea and vomiting
Key Differences Between Heat Exhaustion and Heat Stroke
While heat exhaustion and heat stroke exist on the same spectrum, several critical differences distinguish them:
| Characteristic | Heat Exhaustion | Heat Stroke |
|---|---|---|
| Core Body Temperature | 37.8°C–40°C (100–104°F) | Above 40°C (104°F) |
| Sweating | Heavy, profuse | Little to no |
| Skin Condition | Cool, moist, clammy | Hot, flushed, dry |
| Mental Status | Weakness, fainting | Confusion, seizures, coma |
| Pulse | Fast but weak | Fast and strong |
| Treatment | Rest and rehydration | Immediate emergency care |
Neurological Differences
One of the most significant distinctions between these conditions lies in neurological symptoms. During heat exhaustion, individuals may experience mild confusion, dizziness, or irritability. However, heat stroke produces severe disorientation, hallucinations, seizures, or coma. This difference reflects the severity of central nervous system dysfunction occurring in each condition.
Skin and Sweating Differences
The skin condition provides an important diagnostic clue. During heat exhaustion, skin remains moist because the body still attempts to cool itself through sweating. In contrast, heat stroke causes skin to become hot and dry because sweating stops when the thermoregulatory system fails. Additionally, blood flow redistributes away from the skin toward vital organs, further compromising skin perfusion and appearance.
Why the Distinction Matters for Treatment
Understanding whether you’re dealing with heat exhaustion or heat stroke is not merely academic—it directly determines the urgency and type of treatment required. Heat exhaustion can typically be managed by removing the person from the heat, cooling them with water or fans, and providing fluids with electrolytes. Rest and rehydration are usually sufficient for recovery.
Heat stroke, including sunstroke, is a medical emergency requiring immediate professional intervention. While waiting for emergency services, first aid involves moving the person to a cool location, removing excess clothing, and attempting to cool them with water, fans, ice packs, or cold wet towels. However, professional emergency medical care is absolutely essential because heat stroke can lead to permanent organ damage or death. The longer treatment is delayed, the higher the risk for serious complications.
Risk Factors and Causes
Both heat exhaustion and heat stroke result from similar underlying causes, though the triggers may vary in intensity or duration:
- High environmental temperature with humidity above 60%
- Excessive physical exertion without adequate hydration
- Wearing tight or dark clothing that traps heat
- Dehydration worsened by alcohol or excessive caffeine intake
- Illnesses causing fever
- Poor airflow or confined spaces
- Age-related vulnerability in very young children or older adults
- Certain medical conditions or medications affecting heat tolerance
- Lack of air conditioning or cooling access
Higher humidity levels are particularly dangerous because they prevent effective evaporative cooling through sweating. When humidity exceeds 60%, the body’s natural cooling mechanism becomes increasingly inefficient, accelerating the progression from heat exhaustion to heat stroke.
Onset and Progression Timeline
The timeline for developing heat-related illness varies based on conditions and individual factors. Heat exhaustion typically develops over several hours of continuous heat exposure. However, heat stroke can develop rapidly—often within 10 to 15 minutes if cooling and rehydration efforts fail or if an individual remains in extreme heat conditions without intervention.
This rapid onset emphasizes why recognizing early warning signs of heat exhaustion is crucial. Early identification and treatment of heat exhaustion can prevent the potentially fatal progression to heat stroke.
Vulnerable Populations
While heat-related illnesses can affect anyone during extreme heat, certain populations face elevated risk. These include:
- Young children whose bodies are still developing efficient thermoregulation
- Older adults whose cooling systems become less effective with age
- Individuals with chronic medical conditions
- People taking medications that affect heat tolerance
- Athletes and outdoor workers during peak heat hours
- Individuals without adequate access to air conditioning
- People experiencing obesity, which can impair heat dissipation
Long-Term Consequences of Heat Stroke
The consequences of heat stroke extend far beyond the acute emergency. Survivors may experience lasting complications affecting multiple organ systems. Some individuals develop chronic neurological problems, while others experience permanently reduced heat tolerance. Research shows that once someone has suffered heat stroke, their body does not regulate temperature as effectively going forward, making them more susceptible to developing heat illness again in future heat exposures.
Heat stroke remains a serious public health concern, particularly as climate change increases the frequency and intensity of extreme heat events. Heat stroke can lead to damage of the brain, heart, kidneys, and muscles, with effects ranging from temporary discomfort to permanent disability or death.
Prevention and Protection Strategies
Preventing heat exhaustion and heat stroke requires proactive measures, especially during hot and humid weather:
- Stay hydrated by drinking water consistently throughout the day
- Avoid peak heat hours (typically 10 AM to 4 PM)
- Wear light-colored, loose-fitting, breathable clothing
- Use air conditioning or spend time in cool environments regularly
- Limit strenuous exercise during extreme heat
- Never leave children or pets in vehicles
- Check on vulnerable neighbors, family members, and friends
- Avoid alcohol and excessive caffeine, which increase dehydration risk
- Take frequent breaks during outdoor work or exercise
Frequently Asked Questions
Q: Is sunstroke the same as heatstroke?
A: Yes, sunstroke and heatstroke are essentially the same condition. Both terms describe a medical emergency where core body temperature exceeds 104°F due to failure of the body’s temperature regulation system. The terms are often used interchangeably, though sunstroke may emphasize direct sun exposure while heatstroke is more general.
Q: Can heat exhaustion turn into heat stroke?
A: Yes, heat exhaustion can rapidly progress to heat stroke if left untreated. This is why recognizing early warning signs and taking immediate cooling and rehydration measures is critical. Heat stroke can develop within 10 to 15 minutes if the person remains in the heat without proper intervention.
Q: How fast does heat stroke develop?
A: Heat stroke can occur suddenly, often within 10 to 15 minutes of untreated heat exhaustion or continuous sun exposure in extreme conditions. However, it may also develop over several hours depending on the intensity of heat exposure and individual factors.
Q: Is sweating still possible in heat stroke?
A: No, sweating typically stops in heat stroke because the body’s cooling mechanism has failed. The absence of sweating in hot weather, combined with extremely high body temperature, is a key diagnostic sign of heat stroke.
Q: What should I do if someone has heat stroke?
A: Call 911 immediately. While waiting for emergency services, move the person to a cool location, remove excess clothing, and cool them with water, fans, ice packs, or cold wet towels. Do not delay professional medical care, as heat stroke is a medical emergency requiring immediate treatment.
Q: Are children and older adults more susceptible to heat stroke?
A: Yes, both young children and older adults have less efficient temperature regulation systems, making them more vulnerable to heat exhaustion and heat stroke. Children are still developing their thermoregulatory abilities, while older adults’ systems become less effective with age.
Conclusion
Sunstroke and heatstroke are the same condition—a life-threatening medical emergency requiring immediate professional treatment. While heat exhaustion and heat stroke represent different points on the heat-related illness spectrum, the important distinction lies in recognizing their differences, understanding the critical difference in treatment urgency, and knowing how to respond appropriately. Early recognition of heat exhaustion symptoms can prevent progression to heat stroke. During extreme heat, prioritize hydration, appropriate clothing, cooling breaks, and regular monitoring of yourself and vulnerable individuals. If heat stroke occurs, immediate emergency medical care is essential for survival and minimizing long-term complications. By understanding these conditions and taking preventive measures, you can significantly reduce your risk of serious heat-related illness.
References
- Heat Exhaustion vs. Heat Stroke: Key Differences & Treatment — Metropolis India. 2024. https://www.metropolisindia.com/blog/preventive-healthcare/heat-exhaustion-vs-heat-stroke
- Heat Exhaustion vs. Heat Stroke: Know the Difference — WSIU/OSF HealthCare. 2023-08-28. https://www.wsiu.org/health/2023-08-28/heat-exhaustion-vs-heat-stroke-know-the-difference
- Heat and Health | Climate, Kids, and Health — Harvard School of Public Health. https://hsph.harvard.edu/research/climate-health-c-change/climate-kids-and-health/heat-and-health/
- Heat Stroke vs. Stroke Infographic — American Stroke Association. https://www.stroke.org/en/professionals/stroke-resource-library/prevention/heat-stroke-vs-stroke
- Improving Public Health Messaging on Heat Stroke — Harvard Public Health. https://harvardpublichealth.org/snapshots/improving-public-health-messaging-on-heat-stroke/
Read full bio of medha deb










