Blackwood
Comprehensive guide to Blackwood: causes, clinical features, diagnosis, and management of this rare hypersensitivity reaction.

Author: Dr. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Reviewed and updated January 2026.
What is Blackwood?
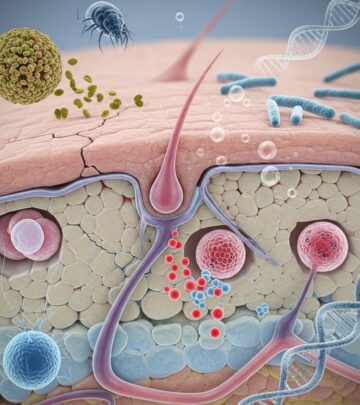
Blackwood is a rare cutaneous hypersensitivity reaction characterized by the development of blue-black discoloration predominantly on the sides of the neck. It arises from contact with specific chemicals, most notably cobalt and chromate compounds found in dyes, metals, and industrial materials. This condition was first described in the 1960s among workers in the wood processing industry, particularly those handling blackwood timber preservatives. The name ‘Blackwood’ derives from the dark pigmentation it produces, resembling wood staining, and its initial observation in forestry workers.
The reaction involves a type IV delayed hypersensitivity mechanism, where T-lymphocytes respond to haptens penetrating the skin barrier. Unlike typical allergic contact dermatitis, Blackwood features persistent hyperpigmentation rather than acute inflammation. It affects individuals with genetic predispositions to metal sensitivities, and cases have been reported globally, though rare in modern settings due to improved workplace regulations.
Who gets Blackwood?
Blackwood primarily affects adults occupationally exposed to chromate and cobalt-containing substances. High-risk groups include:
- Woodworkers and timber processors using chromated copper arsenate (CCA) preservatives.
- Metalworkers handling cobalt alloys or chrome-plated tools.
- Dyers and textile workers exposed to pigment dyes.
- Construction workers dealing with cement (contains hexavalent chromate).
- Plumbers and mechanics using anti-corrosive primers.
Prevalence is higher in males aged 30-60 years due to occupational demographics. Atopic individuals or those with prior metal allergies are more susceptible. Family history of contact dermatitis increases risk. In non-occupational settings, hobbyists like jewelers or artists may develop it from casual exposure.
Causes of Blackwood
The primary triggers are water-soluble cobalt and chromate salts that act as haptens, binding to skin proteins to elicit an immune response. Key sources include:
| Chemical | Common Sources | Exposure Route |
|---|---|---|
| Cobalt chloride | Hard metal alloys, paints, dyes | Skin contact, inhalation |
| Potassium dichromate | Wood preservatives, cement, leather tanning | Dermal absorption |
| Copper chromate | Pressure-treated lumber | Direct handling |
These chemicals penetrate compromised skin barriers, such as from sweat, microtrauma, or occlusion under collars. Repeated low-level exposure leads to sensitization, with manifestations appearing weeks to months later.
Clinical features of Blackwood
The hallmark is bilateral blue-black macules on the lateral neck, often sparing the central area. Lesions are asymptomatic but may itch mildly. Progression includes:
- Early phase: Erythema and slight induration (1-4 weeks post-exposure).
- Pigmented phase: Slate-blue to black patches, 2-10 cm in size, with sharp margins.
- Chronic phase: Post-inflammatory hyperpigmentation lasting months to years.
Associated findings: Occasionally, similar discoloration on axillae, wrists, or eyelids from sweat transfer. No systemic symptoms unless concurrent irritant dermatitis.
Diagnosis of Blackwood
Diagnosis relies on clinical history and patch testing:
- History: Occupational exposure to suspects, temporal relation to onset.
- Examination: Characteristic neck distribution differentiates from acanthosis nigricans or drug eruptions.
- Patch tests: Positive to cobalt (0.5%) and chromate (0.5%) in TRUE Test series. Reactions peak at day 4-7.
- Differential: Excludes Addison disease, argyria, or minocycline pigmentation via biopsy if needed (shows lichenoid infiltrate, hemosiderin deposits).
Wood’s lamp reveals yellowish fluorescence in affected areas.
Management and treatment of Blackwood
Treatment focuses on avoidance and symptom relief:
- Primary: Eliminate exposure via protective clothing, gloves, ventilation. Workplace reassignment if severe.
- Topical: Mid-potency corticosteroids (e.g., clobetasol 0.05%) twice daily for 2 weeks to reduce inflammation. Calcineurin inhibitors (tacrolimus 0.1%) for maintenance.
- Depigmentation: Hydroquinone 4% + tretinoin for persistent hyperpigmentation, under supervision.
- Camouflage: Medical-grade concealers for cosmetic concerns.
Prognosis: Pigmentation fades over 6-24 months with strict avoidance. Recurrence common on re-exposure.
Prevention of Blackwood
Preventive strategies mirror occupational dermatitis protocols:
- Skin protection: Barrier creams, cotton liners under collars.
- Education: Worker training on hazards.
- Surveillance: Regular patch testing in high-risk industries.
- Substitution: Chromate-free alternatives in cement and wood treatments.
Public Health Ontario guidelines emphasize hand care programs to maintain skin integrity.
Frequently asked questions about Blackwood
Q: Is Blackwood contagious?
A: No, Blackwood is not contagious. It is a hypersensitivity reaction limited to the affected individual.
Q: Can Blackwood be cured completely?
A: While pigmentation resolves slowly, complete avoidance prevents recurrence. Some residual marks may persist.
Q: What if patch tests are negative?
A: Consider combined hapten effects or alternative diagnoses like occupational vitiligo. Repeat testing or biopsy may be warranted.
Q: Are there legal implications for affected workers?
A: Yes, recognized as occupational disease; compensation available under workers’ regulations in many countries.
Q: How to differentiate from other neck pigmentations?
A: History of chemical exposure and bilateral lateral distribution distinguish Blackwood from endocrine or drug-induced causes.
Related topics on DermNet
- Allergic contact dermatitis
- Chromate dermatitis
- Cobalt contact dermatitis
- Occupational dermatitis
- Postinflammatory hyperpigmentation
References
- Dermatology Handbook 2021-2022 — Scottish Dermatological Nursing Society. 2021-12-01. https://www.scribd.com/document/716716845/Dermatology-Handbook-2021-2022
- Recommendations for the Prevention, Detection and Management of Occupational Contact Dermatitis — Public Health Ontario. 2019-06-01. https://www.publichealthontario.ca/-/media/documents/g/2019/guide-occupational-dermatitis.pdf
- Dermatological conditions in skin of colour — DermNet NZ. 2024-01-01. https://dermnetnz.org/topics/skin-conditions-in-skin-of-colour
- Skin Conditions A-Z — DermNet NZ. 2026-01-01. https://dermnetnz.org/topics
- Dermatology practice guidelines — DermNet NZ. 2025-01-01. https://dermnetnz.org/topics/dermatology-practice-guidelines
Read full bio of medha deb