Is Blood Like Your Waistline? The Thinner The Better
Understanding how waist circumference impacts cardiovascular and metabolic health outcomes.
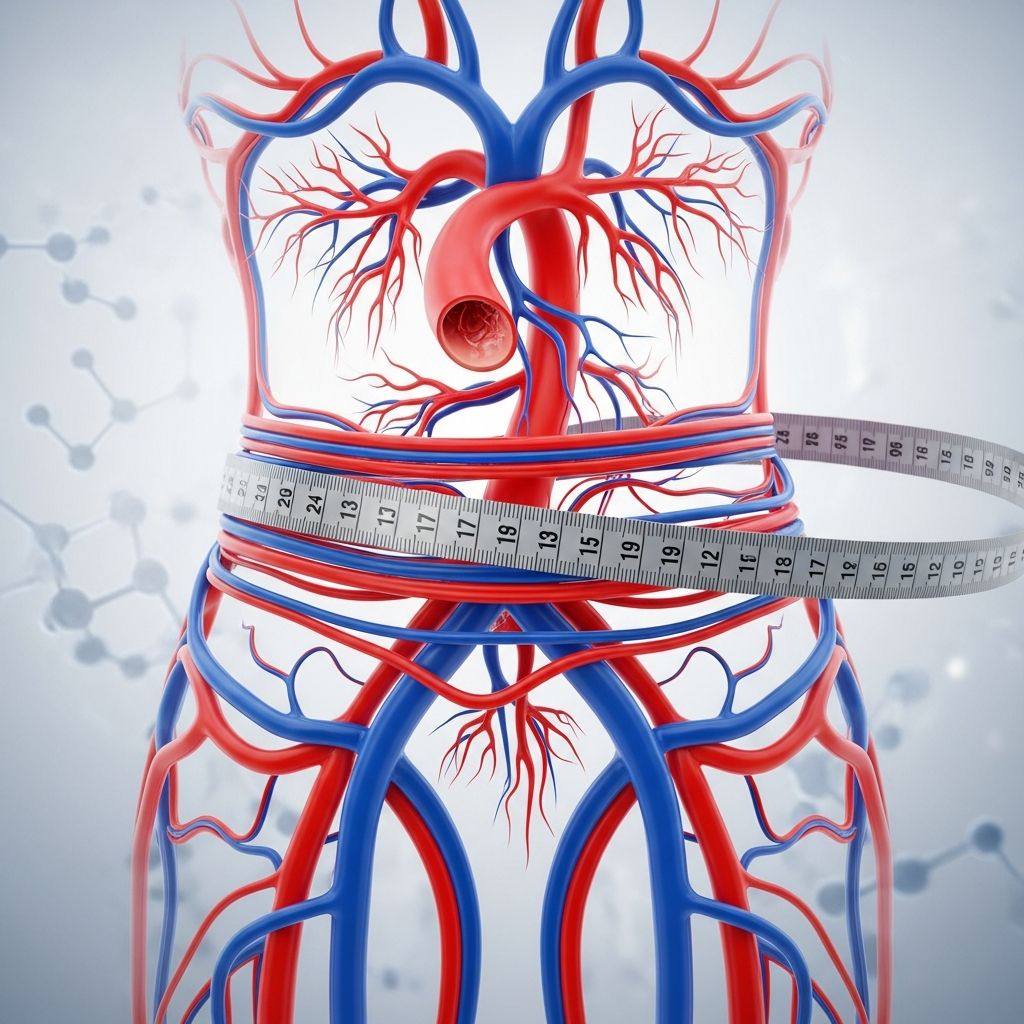
When it comes to health metrics, most people focus on their weight or body mass index (BMI). However, emerging research suggests that where you carry your weight may be just as important—if not more important—than how much you weigh overall. The analogy comparing blood to your waistline reveals a profound truth: just as thinner blood flows more efficiently through your arteries, a thinner waistline may indicate better metabolic health and lower disease risk. This article explores the surprising connection between waist circumference and serious health conditions, demonstrating why your waist measurement deserves careful attention.
Understanding Waist Circumference and Health Risk
For decades, healthcare providers relied primarily on BMI to assess whether someone was overweight or obese. BMI, calculated by dividing a person’s weight in kilograms by their height in meters squared, provides a general estimate of body fat. However, BMI has significant limitations: it doesn’t distinguish between muscle and fat, and it fails to account for the critical difference between where fat is stored on your body.
Waist circumference, by contrast, provides a direct measurement of abdominal fat, particularly visceral fat that surrounds vital organs. This type of fat is metabolically active and significantly more dangerous than fat stored elsewhere on the body. Researchers increasingly consider waist circumference to be a better indicator of health risk than BMI alone, as it addresses the specific health threats posed by visceral abdominal fat.
According to clinical guidelines published by the National Heart, Lung, and Blood Institute (NHLBI) in cooperation with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), a healthy waist limit for women is 35 inches and for men is 40 inches. These measurements are taken at the navel line while standing upright.
The Landmark Nurses’ Health Study
One of the most compelling pieces of evidence linking waist circumference to mortality comes from the Nurses’ Health Study, one of the largest and most comprehensive investigations of its kind. Researchers followed more than 44,000 women over 16 years, tracking their health history and lifestyle factors.
The findings were striking: women with waist sizes of 35 inches or larger were approximately twice as likely to die from heart disease compared with women with waist sizes less than 28 inches. The same pattern held for cancer deaths—women with larger waistlines faced double the risk. Most remarkably, these increased risks persisted even among women with normal BMI, meaning that normal-weight women who carried excess weight around their waist faced elevated health dangers.
In fact, normal-weight women with a waist circumference of 35 inches or higher had three times the risk of death from heart disease compared with normal-weight women whose waists were smaller than 35 inches. This finding fundamentally challenges the notion that weight alone determines health outcomes.
How Visceral Fat Affects Your Body
Understanding why abdominal fat is so dangerous requires examining its biological effects. Visceral fat is not inert tissue; it actively produces hormones and inflammatory substances that influence metabolic function throughout the body.
Cardiovascular Impact: As visceral fat breaks down, it releases fatty acids directly into the bloodstream, increasing cholesterol levels and raising the risk of heart disease. Proteins derived from visceral fat can also inflame blood vessel walls and narrow blood vessels, increasing blood pressure and further compromising cardiovascular health.
Insulin Resistance and Diabetes: Abdominal fat makes your body more resistant to insulin, the hormone responsible for regulating blood sugar. This insulin resistance can lead to type 2 diabetes or pre-diabetes, conditions that dramatically increase risk for other serious health complications.
Neurological Concerns: Recent research has identified links between excess visceral fat and Alzheimer’s disease, suggesting the health implications of abdominal obesity extend beyond metabolic and cardiovascular systems.
Measuring Your Abdominal Fat: Beyond Simple Numbers
While waist circumference remains the most straightforward measurement, researchers have developed several methods to assess abdominal fat and associated health risks:
Waist Circumference
This remains the simplest and most practical measurement. To measure your waist circumference, stand upright and wrap a tape measure around your waist at the navel line, keeping the tape snug but not compressing your skin. The measurement should be taken in inches or centimeters and compared against the NHLBI guidelines: less than 35 inches for women and less than 40 inches for men indicates lower risk.
Waist-to-Hip Ratio (WHR)
Waist-to-hip ratio measures the proportional relationship between your waist and hip circumference. To calculate WHR, measure your waist at the navel line and your hip at the widest part of your buttocks. Then divide your waist measurement by your hip measurement. The World Health Organization defines abdominal obesity in men as a WHR greater than 0.90 and in women as greater than 0.85. Some researchers believe WHR may be superior to waist circumference alone because it accounts for variations in body frame size. However, large studies have found waist circumference and WHR to be equally effective at predicting mortality risk.
Waist-to-Height Ratio (WHtR)
Waist-to-height ratio (WHtR) represents another valuable screening tool for assessing visceral abdominal fat. To determine your WHtR, divide your waist circumference in inches by your height in inches. A measurement of 0.5 or higher indicates health risks related to visceral obesity and has been shown to predict cardiometabolic risk factors such as hypertension and early death, even when BMI falls within a healthy range.
Metabolic Syndrome: When Multiple Risk Factors Converge
Abdominal fat frequently occurs alongside other metabolic abnormalities, creating a dangerous condition called metabolic syndrome. According to health experts, a large waist size is one of five key indicators of metabolic syndrome, the others being high triglycerides, elevated cholesterol, high blood pressure, and elevated blood sugar.
When three or more of these factors occur together, the condition is formally diagnosed as metabolic syndrome. This clustering of risk factors dramatically increases the likelihood of developing heart disease, type 2 diabetes, and stroke. The presence of metabolic syndrome essentially multiplies the health risks associated with any single component, creating a compounding effect that demands immediate medical attention.
Why Normal Weight Isn’t Always Healthy Weight
One of the most important insights from recent research is that normal body weight does not guarantee good health if that weight is concentrated around the midsection. The Nurses’ Health Study demonstrated this clearly: many women with BMI in the normal range still faced significantly elevated mortality risk if their waist circumference exceeded 35 inches.
This phenomenon, sometimes called “normal-weight central obesity,” reveals the inadequacy of BMI as a sole health metric. A person can have a normal weight according to BMI calculations while simultaneously carrying dangerous levels of visceral fat. This explains why some people who appear to have a normal figure still face health risks that traditional weight-based assessments would miss.
The Prevalence of Abdominal Obesity in America
The scope of abdominal obesity in the United States is substantial. In 2004, over half of U.S. adults had abdominal obesity by NHLBI standards, indicating that millions of Americans face elevated health risks from excess midsection fat regardless of their overall BMI classification.
This widespread prevalence underscores the importance of individual awareness and action. Since abdominal obesity represents a modifiable risk factor, individuals who learn about their waist circumference can take steps to reduce health risks through lifestyle modifications.
Gender Differences in Waist Circumference Risk
While the most extensive research on waist circumference and mortality comes from studies of women, the underlying biological mechanisms affecting men are similar. The NHLBI has established different waist circumference thresholds for men (40 inches) compared to women (35 inches), reflecting known physiological differences in how men and women distribute body fat.
Men typically accumulate more visceral fat than women at similar levels of total body fat, contributing to their higher baseline cardiovascular risk. However, the fundamental principle remains constant across genders: excess abdominal fat represents a serious health threat that warrants intervention.
Taking Action: Reducing Abdominal Fat
Understanding the health risks associated with excess waist circumference is the first step. The critical next step involves taking action to reduce abdominal fat through evidence-based approaches:
Dietary Modifications: Research shows that reducing refined carbohydrate consumption and added sugar intake can preferentially reduce visceral fat accumulation. Increasing fiber intake and emphasizing whole grains, vegetables, and lean proteins supports metabolic health.
Physical Activity: Regular exercise, particularly aerobic activity combined with resistance training, effectively reduces visceral fat even without substantial weight loss. Studies demonstrate that individuals who maintain consistent physical activity accumulate less abdominal fat over time.
Medical Consultation: For individuals with waist circumference above recommended thresholds, especially those with additional metabolic risk factors, consulting with a healthcare provider is essential. Medical professionals can assess overall health status and recommend personalized interventions.
Frequently Asked Questions
Q: Is waist circumference a better measure of health than BMI?
A: For predicting disease risk and early mortality, waist circumference provides superior information because it directly measures abdominal fat, which is metabolically active and associated with serious health conditions. However, both measurements offer valuable information when used together.
Q: Can someone with a normal BMI still have health risks from excess waist circumference?
A: Yes. The Nurses’ Health Study demonstrated that normal-weight women with waist circumferences of 35 inches or larger faced three times the risk of heart disease compared with normal-weight women with smaller waistlines. Weight distribution matters significantly for health outcomes.
Q: What is the difference between visceral fat and subcutaneous fat?
A: Visceral fat surrounds internal organs in the abdominal cavity and is metabolically active, releasing fatty acids and inflammatory compounds that affect health. Subcutaneous fat lies beneath the skin and, while also contributing to weight, poses less metabolic danger than visceral fat.
Q: How often should I measure my waist circumference?
A: Measuring waist circumference annually or semi-annually provides reasonable monitoring. Those working to reduce abdominal fat may benefit from more frequent measurements to track progress.
Q: Is there a waist circumference measurement that is too small or unhealthy?
A: While excessively large waist circumference poses clear health risks, extremely small waist measurements can indicate insufficient body fat for normal physiological function. Health professionals recommend measurements within established normal ranges rather than pursuing minimal measurements.
Conclusion: Taking Your Waist Measurement Seriously
The comparison between blood and waistline proves surprisingly apt: just as blood vessel health depends on physical properties like viscosity that allow proper circulation, metabolic health depends significantly on where the body stores fat. The extensive research chronicled here, particularly the Nurses’ Health Study following over 44,000 women for 16 years, demonstrates conclusively that waist circumference represents a critical health metric deserving attention equal to or exceeding that given to BMI.
The evidence is clear: thinner truly is better when it comes to your waistline. Normal-weight individuals with excess abdominal fat face significantly elevated risks for heart disease, cancer, and premature mortality. By understanding your waist circumference, recognizing the dangers of excess visceral fat, and taking action through lifestyle modifications, you can substantially improve your long-term health outcomes and reduce your risk for serious chronic diseases.
References
- Excess Fat Around the Waist May Increase Death Risk for Women — National Institute of Child Health and Human Development (NICHD), National Institutes of Health. 2008-04-07. https://www.nichd.nih.gov/newsroom/releases/april07_2008
- Body Fat – The Nutrition Source: Measuring Fat — Harvard T.H. Chan School of Public Health, Department of Nutrition. https://nutritionsource.hsph.harvard.edu/healthy-weight/measuring-fat/
- How Your Waist Affects Your Health — WebMD. https://www.webmd.com/diet/ss/slideshow-how-waist-affects-health
- Metabolic Syndrome – Symptoms & Causes — Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
Read full bio of medha deb












