25 Breast Health Facts Everyone Should Know
Essential facts about breast anatomy, cancer risks, screening guidelines, and prevention strategies for optimal breast health.
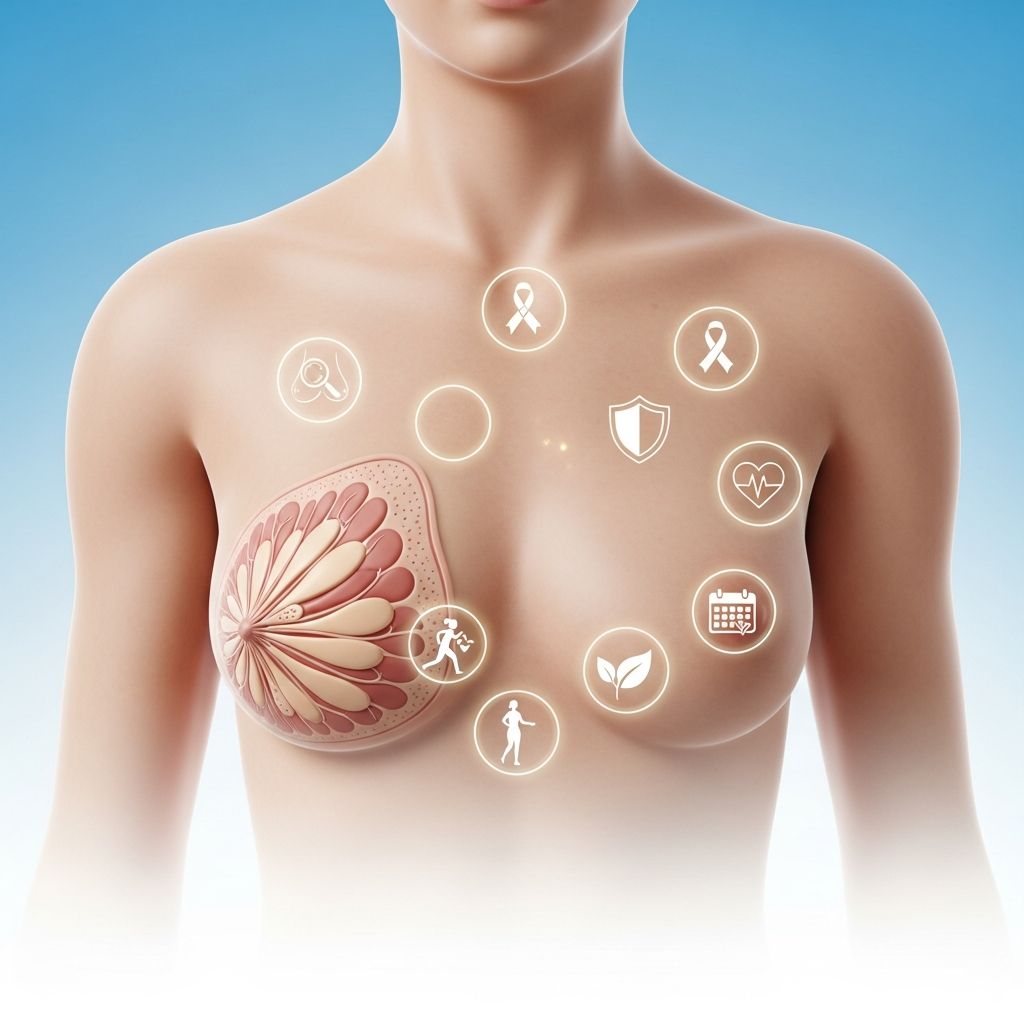
Breasts play a vital role in women’s health, reproduction, and self-image. Understanding key facts about breast anatomy, function, cancer risks, screening methods, and prevention strategies empowers individuals to take proactive steps toward optimal breast health. This comprehensive guide covers 25 essential breast health facts backed by medical authorities, helping you navigate common concerns and make informed decisions.
Breast Anatomy and Function
Breasts are complex glands consisting of glandular tissue, fat, connective tissue, blood vessels, nerves, and lymphatics. They undergo significant changes throughout life stages like puberty, pregnancy, and menopause.
- Fact 1: Adult women have 14-18 milk-producing lobules per breast, arranged like orange slices radiating from the nipple.
- Fact 2: Breasts contain 15-20 major ducts that open at the nipple, responsible for milk ejection during lactation.
- Fact 3: Only 10-15% of breast tissue is glandular; the rest is fatty and supportive tissue, explaining size variations.
- Fact 4: Montgomery glands (small bumps around the nipple) secrete lubricating oils during breastfeeding and pregnancy.
- Fact 5: Breast size correlates more with fat content than milk production capacity—larger breasts don’t mean more milk.
Breast Changes Throughout Life
Hormonal fluctuations cause normal breast changes that can mimic concerning symptoms. Knowing what’s typical helps distinguish normal variations from potential issues.
- Fact 6: Cyclical breast pain (mastalgia) affects 50-70% of women, peaking mid-cycle due to estrogen and progesterone surges.
- Fact 7: Pregnancy causes breasts to increase 1-3 cup sizes as lobules and ducts proliferate for milk production.
- Fact 8: Menopause reduces breast density as glandular tissue converts to fat, often making mammograms easier to read.
- Fact 9: Lumpy breasts are normal in 50% of women, especially during menstrual cycles, due to fibrocystic changes.
- Fact 10: Breast asymmetry (one breast larger) occurs in 25% of women and is usually harmless unless new or progressive.
Breast Cancer Statistics and Risks
Breast cancer remains the most common cancer among women worldwide, but understanding risks enables prevention and early detection.
- Fact 11: About 1 in 8 women in the U.S. will develop invasive breast cancer during their lifetime, per American Cancer Society data.1
- Fact 12: Men account for 1% of breast cancer cases, with ~2,800 new diagnoses yearly in the U.S.
- Fact 13: BRCA1/BRCA2 gene mutations increase lifetime risk to 55-72% (vs. 12% general population).
- Fact 14: Dense breasts (fibroglandular tissue >50%) raise cancer risk 4-6 times and obscure mammogram readings.
- Fact 15: Family history doubles risk if a first-degree relative had breast cancer; triple risk if premenopausal.
Breast Cancer Screening Guidelines
Regular screening dramatically improves outcomes through early detection when treatment success exceeds 99%.
| Age Group | Recommended Screening | Frequency |
|---|---|---|
| 40-49 (average risk) | Discuss with doctor | Annual or biennial mammogram |
| 50-74 | Mammography | Every 2 years2 |
| 75+ | Individualized | Based on health status |
| High risk | Mammogram + MRI | Annual starting age 30 |
- Fact 16: Mammography reduces breast cancer mortality by 20-40% in women 40-74, per USPSTF guidelines.2
- Fact 17: 3D mammography (tomosynthesis) detects 20-65% more invasive cancers than 2D alone.
- Fact 18: Self-exams remain valuable despite controversy; 20% of cancers are found by women themselves.
Breast Self-Examination Technique
Perform monthly self-exams post-menstruation (or same date if postmenopausal) using systematic visual and manual inspection.
- Stand before mirror, arms at sides, overhead, hands on hips—note asymmetry, dimpling, nipple changes.
- Lie down; use opposite hand’s pads (not tips) in quarter-sized circles covering entire breast.
- Examine under shower with soapy hand for easier gliding.
- Check armpit and collarbone areas for swollen lymph nodes.
- Squeeze nipples gently for discharge (clear, bloody requires evaluation).
Common Benign Breast Conditions
Most breast lumps (80-90%) prove benign. Prompt evaluation prevents unnecessary worry.
- Fact 19: Fibroadenomas (solid, rubbery, mobile lumps) affect 9% of women, typically ages 15-35.
- Fact 20: Cysts (fluid-filled sacs) cause painful lumps, common ages 30-50, resolve with aspiration.
- Fact 21: Intraductal papillomas cause bloody nipple discharge; usually benign but require biopsy.
Breast Cancer Symptoms and Signs
Early breast cancer often produces no symptoms, underscoring screening importance. Know these red flags:
- New lump/thickening differing from surrounding tissue
- Pit dimpling, puckering, or scaliness
- Nipple retraction, crusting, or bloody discharge
- Persistent pain (uncommon early sign)
- Swelling of all/part of breast or armpit
- Skin changes resembling orange peel (peau d’orange)
Prevention and Risk Reduction
Lifestyle modifications meaningfully lower risk alongside unavoidable factors like genetics and age.
- Fact 22: Maintaining BMI <25 reduces risk by 20-30%; postmenopause, fat converts to estrogen.3
- Fact 23: Limit alcohol to <1 drink/day (increases risk 7-10% per drink).
- Fact 24: Pregnancy before age 30 and breastfeeding ≥1 year each reduce risk 4-5% per year.
- Fact 25: Prophylactic medications (tamoxifen) reduce risk 30-50% in high-risk women.
Frequently Asked Questions (FAQs)
Does breastfeeding cause breast cancer?
No—breastfeeding reduces risk by suppressing ovulation and removing cells during milk production. WHO recommends 2+ years total across lifetime for protection.3
Are underwire bras dangerous?
No evidence links underwire bras to cancer. The 1970s myth originated from misinterpreted lymph blockage theories, debunked by major cancer organizations.
Does deodorant cause breast cancer?
Aluminum compounds faced scrutiny, but 2014 review of 20+ studies found no causal link. Apply post-shaving to minimize skin absorption anyway.
When to start mammograms?
USPSTF recommends biennial screening ages 50-74 for average risk; begin earlier/discuss annually ages 40-49. High-risk individuals start at 30 with MRI adjunct.
Can men get breast cancer?
Yes—men have breast tissue that can develop cancer, though estrogen exposure is lower. Risk factors mirror women’s: age, family history, radiation.
Final Thoughts on Breast Health
Knowledge serves as the cornerstone of breast health. Regular self-awareness, professional screenings, healthy lifestyle choices, and prompt attention to changes save lives. Consult healthcare providers for personalized risk assessment and screening plans. Early detection transforms breast cancer from fatal diagnosis to manageable condition with excellent prognoses.
References
- Breast Cancer Statistics — American Cancer Society. 2025-01-10. https://www.cancer.org/cancer/types/breast-cancer/about/how-common-is-breast-cancer.html
- Breast Cancer Screening — U.S. Preventive Services Task Force. 2024-04-30. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
- World Cancer Report: Breast Cancer Prevention — World Health Organization. 2024-02-03. https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- Breast Density and Cancer Risk — National Cancer Institute. 2025-06-15. https://www.cancer.gov/types/breast/breast-changes/dense-breasts
- Genetics of Breast and Gynecologic Cancers — National Cancer Institute. 2024-11-20. https://www.cancer.gov/types/breast/hp/breast-ovarian-genetics-pdq
Read full bio of medha deb











