Bronchogenic Cyst Pathology
Detailed histopathology, clinical features, and management of bronchogenic cysts, rare foregut-derived malformations.
Author: Dermatopathology Expert | Last Updated: 2025
Introduction
Bronchogenic cysts are rare congenital malformations originating from anomalous budding of the ventral foregut during early embryonic development, specifically between the 3rd and 7th weeks of gestation. These cysts arise from the primitive respiratory diverticulum and are typically lined by respiratory-type epithelium, distinguishing them from other cutaneous or mediastinal cysts. Although primarily intrathoracic, affecting the mediastinum (50-70% of cases), lungs, or tracheobronchial tree, superficial bronchogenic cysts can present in the skin, particularly in the presternal or suprasternal regions, prompting dermatopathological evaluation.
These benign lesions are often asymptomatic and discovered incidentally on imaging or excision, but they can enlarge, become infected, or compress adjacent structures, leading to symptoms like cough, dyspnea, chest pain, or recurrent infections. Rarely, malignant transformation or fistulization occurs, underscoring the importance of accurate histopathological diagnosis. Bronchogenic cysts affect males and females equally and are associated with other congenital anomalies in some cases.
Histology
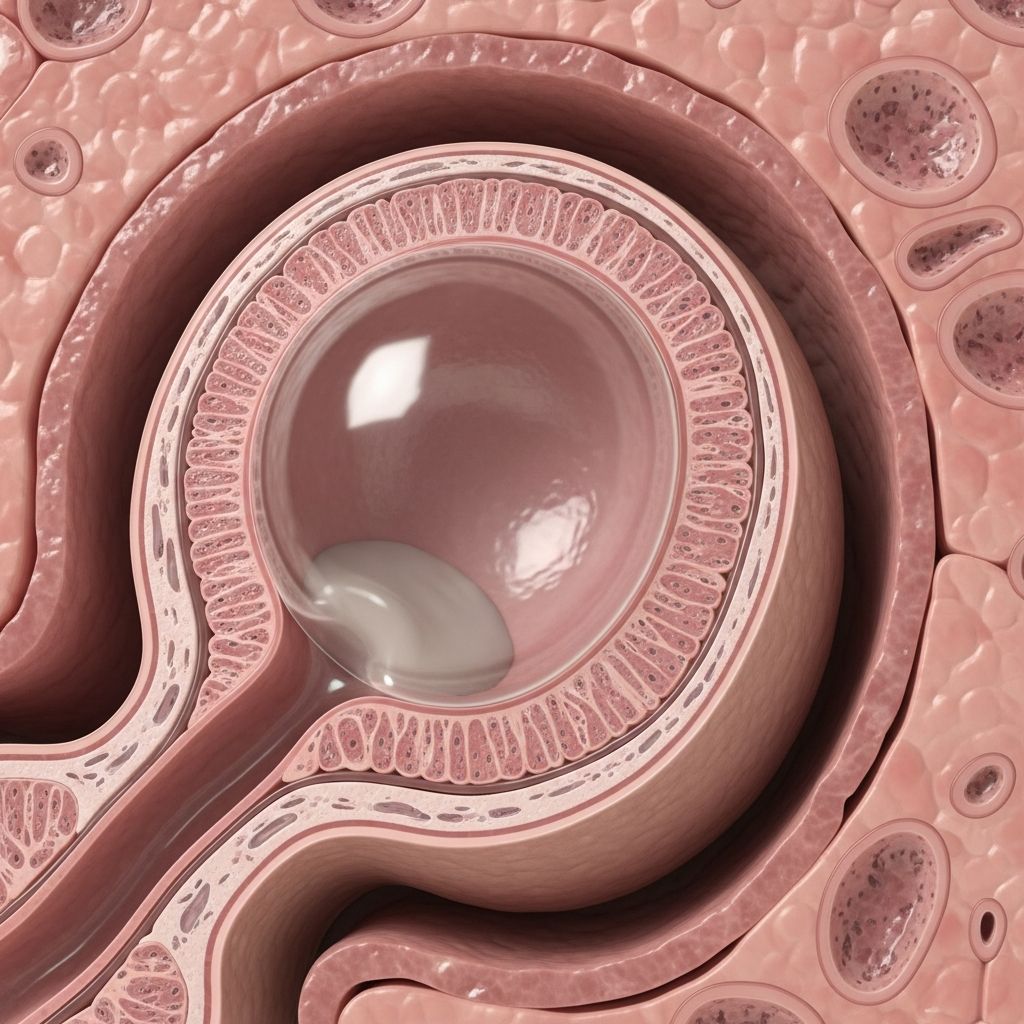
Microscopically, bronchogenic cysts are characterized by a cyst wall lined by pseudostratified ciliated columnar epithelium, resembling respiratory epithelium, often with goblet cells producing mucin (present in about 50% of cases). The wall contains subepithelial structures mirroring bronchial anatomy, including smooth muscle bundles, seromucinous glands, elastic tissue, and occasionally cartilage plates. Inflammatory changes, such as chronic lymphocytic infiltrates, may be seen if infected or infarcted.
In cutaneous presentations, the cyst is dermally based, filled with proteinaceous fluid, mucin, or debris. Higher magnification reveals cilia on the epithelial surface, confirming ciliated pseudostratified columnar cells. Epithelial denudation can occur due to inflammation, leading to reactive fibrosis, hemosiderin-laden macrophages, or cholesterol clefts. Smooth muscle is a hallmark feature, often forming a thick layer around the cyst, and is rarely seen in mimics like cutaneous ciliated cysts.
- Epithelium: Pseudostratified ciliated columnar with goblet cells; areas of squamous metaplasia possible.
- Wall components: Smooth muscle, mucous glands, cartilage (sometimes), elastic fibers.
- Contents: Mucoid material, inflammatory debris if complicated.
- Changes: Inflammation (acute/chronic), fibrosis, hemorrhage in altered cases.
Special Studies
Special stains are rarely required for diagnosis, as routine haematoxylin and eosin (H&E) sections suffice. However, mucicarmine or Alcian blue can highlight mucin in goblet cells and gland lumina. Elastic stains (e.g., Verhoeff-van Gieson) demonstrate elastic fibers in the wall. Immunohistochemistry is not typically needed but may show cytokeratins (CK7+, CK20-), TTF-1 positivity in respiratory epithelium, and SMA positivity in smooth muscle if confirmation is sought. Electron microscopy can confirm cilia ultrastructure in ambiguous cases.
No molecular studies are routinely indicated, though rare associations with genetic anomalies have been noted.
Differential Diagnoses
Bronchogenic cysts must be differentiated from other cysts with ciliated or glandular linings, particularly in cutaneous or suprasternal locations. Key discriminators include the presence of smooth muscle, glands, cartilage, and midline location.
| Entity | Key Features | Differentiating from Bronchogenic Cyst |
|---|---|---|
| Branchial Cleft Cyst | Squamous or ciliated lining, prominent lymphoid tissue in wall, rare smooth muscle. | Lacks smooth muscle/glands; lymphoid stroma prominent; lateral neck location. |
| Cutaneous Ciliated Cyst | Cuboidal/columnar ciliated epithelium, no smooth muscle, glands, or cartilage; often on lower extremities. | Absence of bronchial elements (muscle, glands); not midline. |
| Thymic Cyst | Hassall corpuscles, lymphoid tissue, cervical thymic remnants. | Hassall bodies absent in bronchogenic; no respiratory epithelium typically. |
| Enteric Duplication Cyst | Gastrointestinal epithelium (squamous, gastric, intestinal), no cilia. | Gastrointestinal mucosa vs. respiratory; more GI glands. |
| Epidermoid Cyst | Stratified squamous lining, keratin debris, no adnexal structures. | No cilia, respiratory epithelium, or smooth muscle. |
| Metastatic SCC | Atypia, invasion, keratin pearls in cystic metastasis. | Cytologic atypia, mitotic activity absent in benign cyst. |
In complicated cases (e.g., infected), overlap with abscess or necrotic tumors increases, necessitating careful sampling.
Clinicopathological Variants
Intradermal/Superficial: Rare, present as painless nodules in presternal skin; identical histology to deep counterparts.
Infected/Inflamed: Acute inflammation, epithelial ulceration, pus; chronic cases show fibrosis.
Mediastinal: Larger, compressive; same features but may have more cartilage.
Associated Anomalies: Rarely with vertebral or cardiac defects.
Management and Prognosis
Surgical excision is the gold standard, curative with low recurrence if complete. Indicated for symptomatic cysts, infection, compression, or diagnostic uncertainty. Conservative management (observation/imaging follow-up) suits small asymptomatic lesions.
Post-excision, monitor for recurrence (rare <5%) via CT/MRI. Complications like malignancy are exceptional (<1%), but long-term surveillance advised.
Frequently Asked Questions (FAQs)
What is a bronchogenic cyst?
A rare congenital cyst from foregut budding, lined by respiratory epithelium with smooth muscle wall, often in mediastinum or skin.
How is bronchogenic cyst diagnosed histologically?
Ciliated pseudostratified epithelium, smooth muscle, glands; differentiates from branchial cyst by lacking lymphoid tissue.
Is surgery always needed for bronchogenic cysts?
No, asymptomatic cysts may be observed; excise if symptomatic, infected, or compressive.
Can bronchogenic cysts become cancerous?
Extremely rare; monitor for changes in size or symptoms.
Where do cutaneous bronchogenic cysts occur?
Typically midline presternal or suprasternal skin.
Clinical Presentation
Most are incidental; symptoms from mass effect: dyspnea (airway compression), pain, infection (fever, cough). Pediatric cases often earlier due to growth.
Imaging Features
CT/MRI: well-defined, round, non-enhancing cystic lesion, water/mucin density. Location aids diagnosis: paratracheal, subcarinal, hilar.
References
- Bronchogenic Cyst – StatPearls — NCBI Bookshelf / StatPearls Publishing. 2023-10-01. https://www.ncbi.nlm.nih.gov/books/NBK536973/
- Branchial Cleft Cyst Pathology — DermNet NZ. 2013-01-01. https://dermnetnz.org/topics/branchial-cleft-cyst-pathology
- Cutaneous Ciliated Cyst Pathology — DermNet NZ. 2023-01-01. https://dermnetnz.org/topics/cutaneous-ciliated-cyst-pathology
- Bronchogenic Cyst Pathology Image — DermNet NZ. 2023-01-01. https://dermnetnz.org/imagedetail/12504-bronchogenic-cyst-pathology
- Bronchogenic Cyst: 5-Minute Pathology Pearls — YouTube / Pathology Expert. 2023-01-01. https://www.youtube.com/watch?v=6gBujD1O_tk
Read full bio of Sneha Tete












