Carcinoma Cuniculatum
Rare, locally aggressive squamous cell carcinoma variant often misdiagnosed as warts, primarily affecting foot soles.
Authoritative facts about carcinoma cuniculatum from DermNet New Zealand, synthesized with peer-reviewed sources for comprehensive clinical insights.
What is carcinoma cuniculatum?
Carcinoma cuniculatum (CC), also known as verrucous carcinoma or cuniculatum epithelioma, is a rare variant of well-differentiated squamous cell carcinoma (SCC). Unlike typical SCC linked to ultraviolet (UV) exposure, CC primarily arises from chronic trauma and inflammation, most commonly on the soles of the feet. It features a distinctive pattern of deep, keratin-filled burrows or sinus tracts that give it a ‘rabbit burrow’ appearance, from which the Latin term ‘cuniculatum’ derives, meaning ‘rabbit-like’.
This low-grade malignancy grows slowly but exhibits locally aggressive behavior, invading surrounding soft tissues and bone if untreated. Metastasis is exceedingly rare, occurring in fewer than 1% of cases, distinguishing it from higher-grade SCCs. First described in 1954, CC accounts for a small fraction of cutaneous SCCs, with fewer than 100 cases well-documented in medical literature.
CC’s exophytic, wart-like presentation often leads to misdiagnosis as benign conditions like verruca vulgaris (plantar warts), delaying definitive treatment. Early recognition is crucial to prevent extensive local destruction requiring amputation in advanced stages.
Who gets carcinoma cuniculatum?
Carcinoma cuniculatum predominantly affects adults over 50 years, with a mean age of diagnosis around 60-70 years. Males are slightly more commonly affected than females, possibly due to occupational trauma exposure.
Key risk factors include:
- Chronic mechanical trauma: Repeated pressure or friction on weight-bearing areas like the heel or metatarsal heads, common in manual laborers or athletes.
- Long-standing inflammation: Associated with chronic wounds, ulcers, or infections.
- Human papillomavirus (HPV): Some cases link to beta-HPV types, though less directly than in typical warts.
- Immunosuppression: Higher incidence in immunocompromised patients, including organ transplant recipients or those with HIV.
- Arsenic exposure: Historical links to chronic arsenic ingestion via contaminated water or medications.
Unlike actinic SCC, CC shows no strong association with UV radiation or fair skin types. It is exceptionally rare in children and on sun-exposed sites.
What causes carcinoma cuniculatum?
The pathogenesis of CC involves a combination of chronic irritation and genetic alterations promoting keratinocyte proliferation. Persistent trauma induces hyperkeratosis and epithelial hyperplasia, creating a nidus for malignant transformation.
Molecular insights reveal disruptions in key pathways:
- Notch signaling pathway: Impaired cell differentiation leads to unchecked proliferation.
- RAS-RAF-MEK-ERK pathway: Enhances cell survival and invasion.
- p53 dysfunction: Beta-HPV E6 proteins inhibit UV-induced apoptosis, though UV is not primary.
Immunosuppression exacerbates susceptibility by impairing tumor surveillance, depleting Langerhans cells, and shifting immune responses. Unlike high-grade SCC, CC retains well-differentiated features with minimal cytological atypia, explaining its low metastatic potential.
What are the clinical features of carcinoma cuniculatum?
CC typically presents as a slow-growing, exophytic plaque on the sole of the foot, often the heel. Lesions measure 1-10 cm, with a verrucous, hyperkeratotic surface resembling a giant wart.
Hallmark features include:
- Sinus tracts: Multiple deep, sinuous burrows discharging foul-smelling, yellow keratin debris, mimicking infection.
- Local invasion: Pain, swelling, and ulceration as it erodes into dermis, subcutaneous fat, and bone.
- Secondary infection: Erythema, pus, and malodor from bacterial superinfection.
- Neglected growth: Patients often ignore early lesions due to painless onset.
Rare sites include the oral cavity, nail bed, or upper extremities. Advanced cases show bone involvement on X-ray, with cortical erosion.
Differential diagnosis
| Condition | Key Distinguishing Features |
|---|---|
| Verruca vulgaris | Smaller, multiple warts; no deep burrows; HPV-positive; resolves with treatment. |
| Plantar fibromatosis | Firm nodules without keratin tracts; no malignancy. |
| Chronic osteomyelitis | Sinus tracts with pus, not keratin; systemic signs; imaging shows sequestra. |
| Other SCC variants | More atypia, ulceration; UV association. |
| Blastomycosis | Fungal elements on biopsy; satellite lesions. |
Pathology of carcinoma cuniculatum
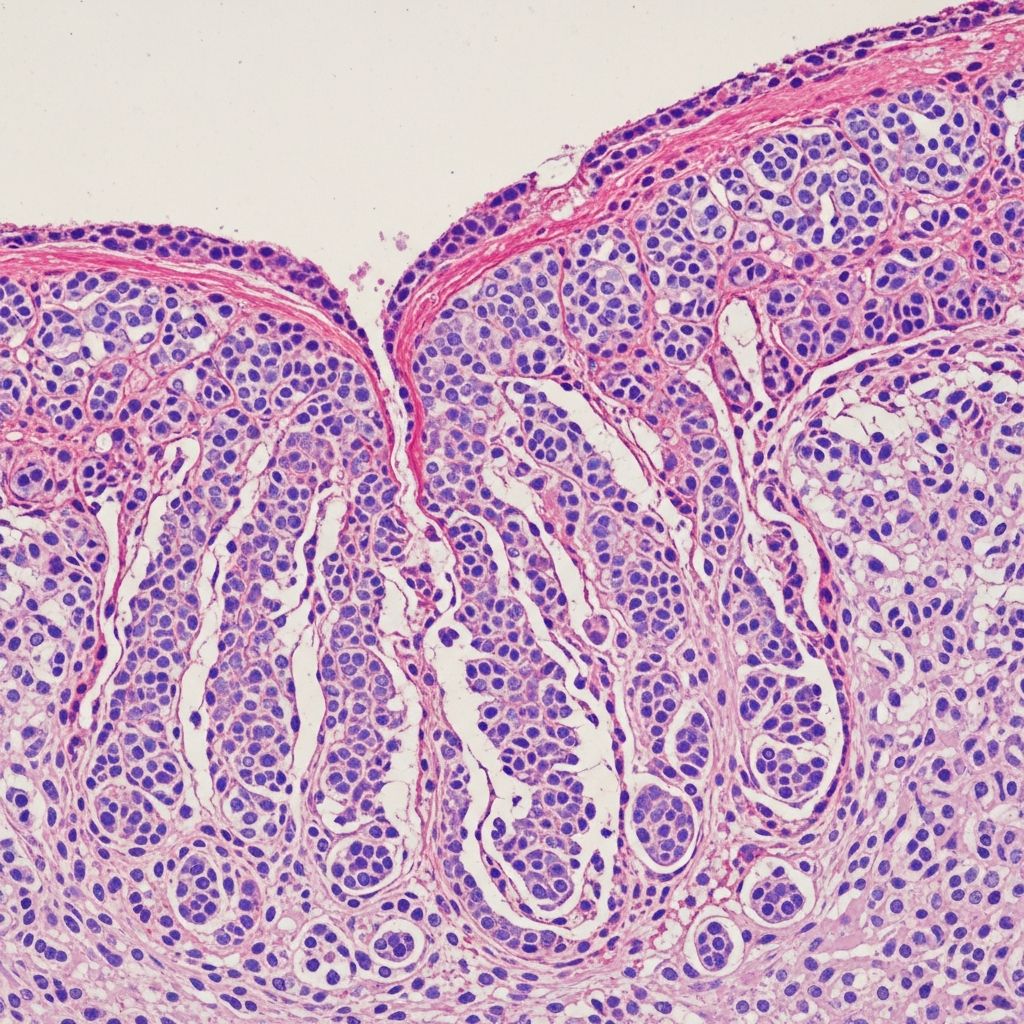
Histopathology confirms diagnosis, revealing broad, bulbous papillary projections of well-differentiated SCC extending into deep dermis. Minimal cytological atypia: large keratinocytes with abundant cytoplasm, sharp stratification, and keratin pearls filling ‘cuniculi’ burrows.
Key microscopic features:
- Exophytic growth: Pushing borders without jagged invasion.
- Keratin-filled tracts: Horizontal and vertical sinuses lined by squamous epithelium.
- Stromal inflammation: Dense lymphocytic infiltrate.
- No/ minimal atypia: Rare mitoses; low Ki-67 index.
- Bone invasion: Reactive osteoclastic activity in advanced cases.
Immunohistochemistry shows p63 positivity and low p53 expression. Biopsy must include deep burrows to avoid sampling error.
How is carcinoma cuniculatum diagnosed?
Diagnosis combines clinical suspicion, imaging, and biopsy:
- Clinical exam: Persistent wart-like lesion unresponsive to therapy.
- Imaging: X-ray/MRI for bone/soft tissue invasion; sinus tracts visible.
- Deep biopsy: Punch or incisional, targeting burrows.
- Microbiology: Rule out infection.
Podiatric or dermatologic referral is essential.
What is the treatment for carcinoma cuniculatum?
Surgical excision is the cornerstone, given poor response to nonsurgical therapies:
- Wide local excision (WLE): 5-10 mm margins, including burrows; primary closure or graft.
- Mohs micrographic surgery (MMS): Preferred for tissue sparing and clearance confirmation; high cure rates (95%).
- Amputation: For extensive bone involvement.
Radiotherapy is ineffective due to low vascularity; chemotherapy reserved for metastasis (rare). Recurrence risk: 10-20% if margins incomplete; follow-up with imaging.
What is the prognosis for carcinoma cuniculatum?
Excellent with complete excision: 5-year survival near 100%. Local recurrence possible but metastasis rare (inguinal nodes in <1%). Early intervention prevents morbidity.
Frequently Asked Questions (FAQs)
Q: Is carcinoma cuniculatum cancerous?
A: Yes, it is a low-grade squamous cell carcinoma, but rarely metastasizes.
Q: Can carcinoma cuniculatum be mistaken for a wart?
A: Frequently; deep biopsy differentiates it from verruca vulgaris.
Q: Does it spread to other parts of the body?
A: Metastasis is extremely rare; local invasion is the main concern.
Q: What if it’s on the foot sole?
A: Surgical excision with margins; Mohs ideal for functional preservation.
Q: How preventable is it?
A: Minimize chronic foot trauma; treat persistent lesions promptly.
References
- Squamous Cell Carcinoma and Its Rare Variant Carcinoma Cuniculatum — PubMed Central. 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11988111/
- Carcinoma cuniculatum: a case metastasizing to skin and lymph nodes — Clinical and Experimental Dermatology, Oxford Academic. 1981-11-01. https://academic.oup.com/ced/article/6/6/613/6632036
- Carcinoma cuniculatum (verrucous carcinoma of the skin) — Cancer, Wiley. 1982-06-01. https://acsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/1097-0142(19820601)49:11%3C2395::AID-CNCR2820491129%3E3.0.CO;2-3
- Verrucous carcinoma – Primary Care Dermatology Society — PCDS. Recent update. https://www.pcds.org.uk/clinical-guidance/verrucous-carcinoma
Read full bio of Sneha Tete