Causes of Atopic Dermatitis
Unraveling the genetic, immune, and environmental factors driving atopic dermatitis and eczema flares.
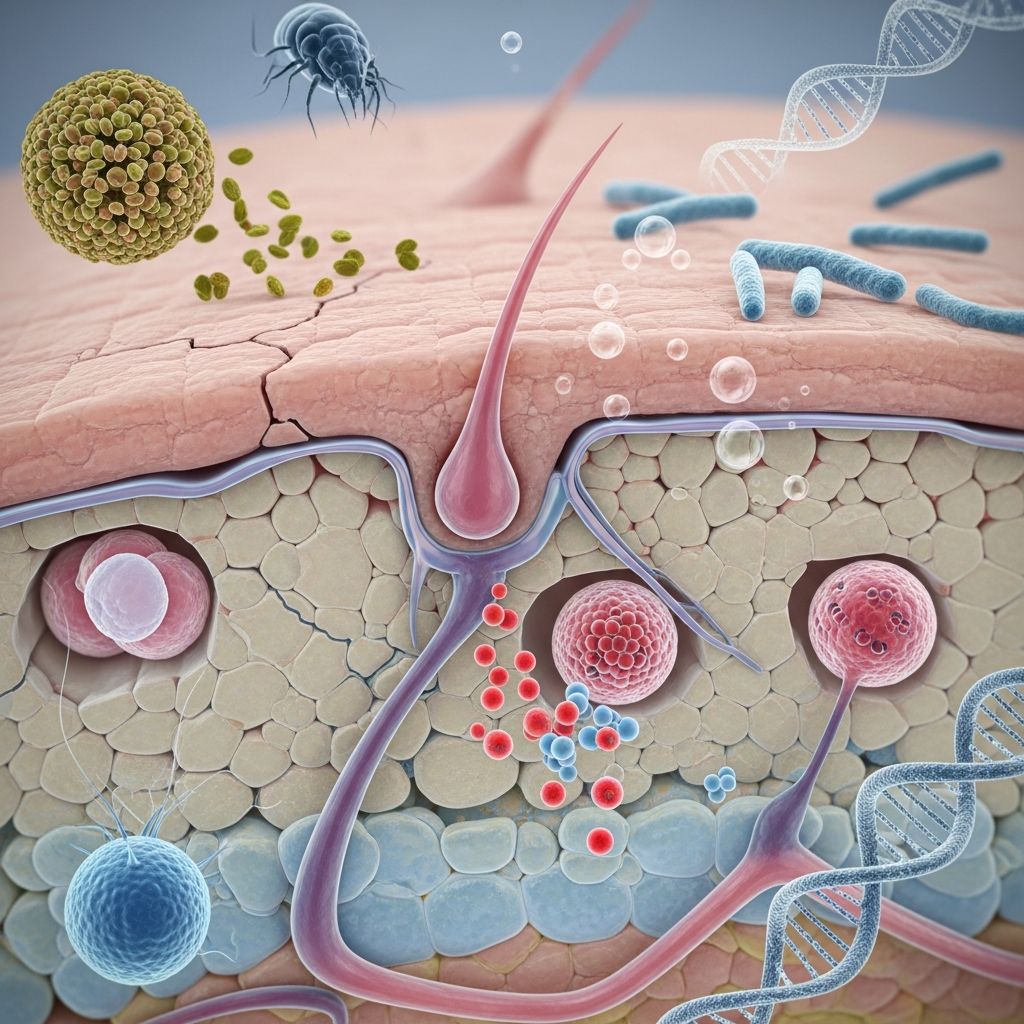
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition characterized by itchy, red, and dry skin. Its exact etiology remains multifactorial, involving a complex interplay of genetic predispositions, immune system dysregulation, impaired skin barrier function, microbial factors, and environmental triggers. While no single cause has been identified, research consistently points to these elements as key contributors to disease onset and flares.
Genetic Factors
Genetics play a pivotal role in atopic dermatitis susceptibility. Family history significantly increases risk; individuals with a parent or sibling affected are more likely to develop the condition. Mutations in the filaggrin gene (FLG), which encodes a protein essential for maintaining the skin’s protective barrier, are among the most well-established genetic links. Filaggrin helps form a robust stratum corneum, retaining moisture and blocking irritants, allergens, and microbes. Loss-of-function mutations in FLG lead to a defective skin barrier, heightened transepidermal water loss, and increased penetration of harmful substances, predisposing individuals to inflammation and itch.
Studies show FLG mutations are present in up to 20-30% of atopic dermatitis patients, particularly those with early-onset and severe disease. These mutations not only impair barrier integrity but also enhance allergic sensitization. Beyond FLG, other genes regulating immune responses, such as those involved in T-cell differentiation and cytokine production (e.g., IL-4, IL-13 pathways), contribute to the Th2-skewed immune profile characteristic of atopic dermatitis. Twin studies further support heritability, with concordance rates higher in monozygotic twins (up to 77%) compared to dizygotic ones (23-64%).
- Key genetic associations:
- Filaggrin (FLG) mutations: Primary defect in epidermal barrier.
- Genes for immune regulation: Promote Th2 inflammation.
- Family atopy history: Includes eczema, asthma, hay fever.
Immune System Dysregulation
The immune system in atopic dermatitis patients exhibits a hyperreactive state, particularly a Th2-dominant response that drives chronic inflammation. This dysregulation leads to overproduction of pro-inflammatory cytokines like IL-4, IL-13, and IL-31, which amplify itch, barrier disruption, and eosinophil recruitment. In acute phases, this manifests as intense pruritus and weeping lesions; chronically, it results in skin thickening (lichenification).
Unlike healthy skin, where immune responses resolve post-threat, atopic skin sustains activation. This ‘immune confusion’ allows allergens and irritants to provoke exaggerated reactions. Research from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) highlights how genetic defects expose the immune system to environmental insults, perpetuating the cycle. Additionally, impaired regulatory T-cells fail to dampen inflammation, contributing to persistence.
Skin Barrier Dysfunction
A hallmark of atopic dermatitis is the compromised skin barrier, often described as ‘leaky skin.’ The stratum corneum, the outermost layer, normally acts as a ‘brick-and-mortar’ structure: corneocytes (bricks) embedded in lipids (mortar). In atopic dermatitis, this structure weakens due to reduced ceramide production, abnormal lipid processing, and filaggrin deficiency, leading to increased permeability.
Consequently, the skin loses moisture (xerosis), becomes prone to cracking, and allows ingress of allergens, bacteria, and irritants. This triggers itch-scratch cycles, further damaging the barrier and inviting secondary infections. Mayo Clinic notes that weak barrier function directly elicits immune responses, causing inflamed, symptomatic skin. pH imbalances (more alkaline skin surface) also exacerbate protease activity, degrading barrier proteins.
| Normal Skin Barrier | Atopic Dermatitis Skin |
|---|---|
| Intact filaggrin and lipids retain moisture | FLG mutations cause dry, permeable skin |
| Resists irritants and microbes | Allows penetration, leading to inflammation |
| Neutral pH protects integrity | Alkaline pH worsens degradation |
Microbial Factors
Skin dysbiosis, particularly overgrowth of Staphylococcus aureus (S. aureus), is a critical driver in atopic dermatitis. Healthy skin hosts a balanced microbiome, but in atopic dermatitis, S. aureus colonizes up to 90% of lesional skin, displacing commensals like Staphylococcus epidermidis. This bacterium produces toxins (e.g., superantigens) that supercharge immune responses, exacerbate inflammation, and promote barrier breakdown via proteases.
NIAMS research indicates that bacterial dominance disrupts barrier function, fostering a vicious cycle of infection and flares. Viral infections (e.g., herpes simplex) and fungal elements can compound this, but S. aureus remains predominant. Antibiotic stewardship and bleach baths target this effectively.
Environmental Triggers
While not primary causes, environmental factors provoke flares in genetically susceptible individuals. Common triggers disrupt the already fragile barrier or ignite immune responses.
- Climate: Low humidity, extreme cold/heat, dry air cause xerosis.
- Irritants: Soaps, detergents, fragrances, wool/synthetic fabrics.
- Allergens: Dust mites, pollen, pet dander, mold.
- Lifestyle: Sweat, stress, tobacco smoke, pollutants.
Children’s Hospital guide emphasizes avoiding bubble baths and harsh laundry products. Stress elevates cortisol, impairing barrier repair.
Other Contributing Factors
Atopic dermatitis often clusters in the ‘atopic march,’ progressing from eczema to asthma, allergic rhinitis, and food allergies, sharing genetic and immune underpinnings. Food allergens (e.g., milk, eggs in infants) trigger some, though less common in adults. Occupational exposures like wet work heighten hand dermatitis risk. Psychological factors, including anxiety, worsen via neuro-immune axes.
Frequently Asked Questions (FAQs)
Q: Is atopic dermatitis genetic?
A: Yes, strongly; filaggrin mutations and family history of atopy increase risk significantly.
Q: Can infections cause atopic dermatitis?
A: Not directly, but S. aureus overgrowth worsens flares by disrupting the skin barrier and fueling inflammation.
Q: What are the most common triggers?
A: Irritants like soaps, dry air, allergens (dust mites, pollen), stress, and sweat.
Q: Does diet play a role?
A: In some infants with allergies, but not primary for most; breastfeeding may protect high-risk babies.
Q: Is atopic dermatitis contagious?
A: No, it’s not infectious; secondary bacterial infections can occur from scratching.
Pathophysiology Overview
Atopic dermatitis arises from epidermal barrier defects (genetic, lipid abnormalities) allowing allergen/microbe entry, triggering Th2 immunity (IL-4/13/31), itch, scratching, and further barrier loss. S. aureus amplifies via toxins. This ‘outside-in’ and ‘inside-out’ failure perpetuates chronicity.
Recent advances implicate IL-4Rα signaling and JAK-STAT pathways as therapeutic targets, validating these mechanisms. Prevalence is rising in industrialized nations, possibly due to hygiene hypothesis—reduced early microbial exposure skews immunity.
Management hinges on restoring barrier (emollients), suppressing inflammation (topicals, biologics), eradicating microbes, and trigger avoidance. Early intervention prevents atopic march.
References
- Atopic Dermatitis: Causes, Symptoms, and Treatment — Feinstein Dermatology. 2023. https://feinsteindermatology.com/blog/atopic-dermatitis-causes-symptoms-and-treatment/
- Atopic dermatitis (eczema) – Symptoms and causes — Mayo Clinic. 2023-10-27. https://www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273
- Atopic Dermatitis – A Guide for Your Family — Boston Children’s Hospital. 2025-02. https://www.childrenshospital.org/sites/default/files/2025-02/atopic-dermatitis-guide-english.pdf
- Atopic Dermatitis–Eczema Symptoms & Causes — NIAMS, NIH. 2023. https://www.niams.nih.gov/health-topics/atopic-dermatitis
- Atopic Dermatitis: Causes, Symptoms, Diagnosis — National Eczema Association. 2023. https://nationaleczema.org/types-of-eczema/atopic-dermatitis/
- Atopic Dermatitis — Physicians Committee for Responsible Medicine Nutrition Guide. 2023. https://nutritionguide.pcrm.org/nutritionguide/view/Nutrition_Guide_for_Clinicians/1342028/all/Atopic_Dermatitis
Read full bio of Sneha Tete












