Cholestasis: Definition, Symptoms, Treatment, Causes
Understanding cholestasis: causes, symptoms, diagnosis, and treatment options for bile flow disorders.
Cholestasis: Definition, Symptoms, Treatment, and Causes
What Is Cholestasis?
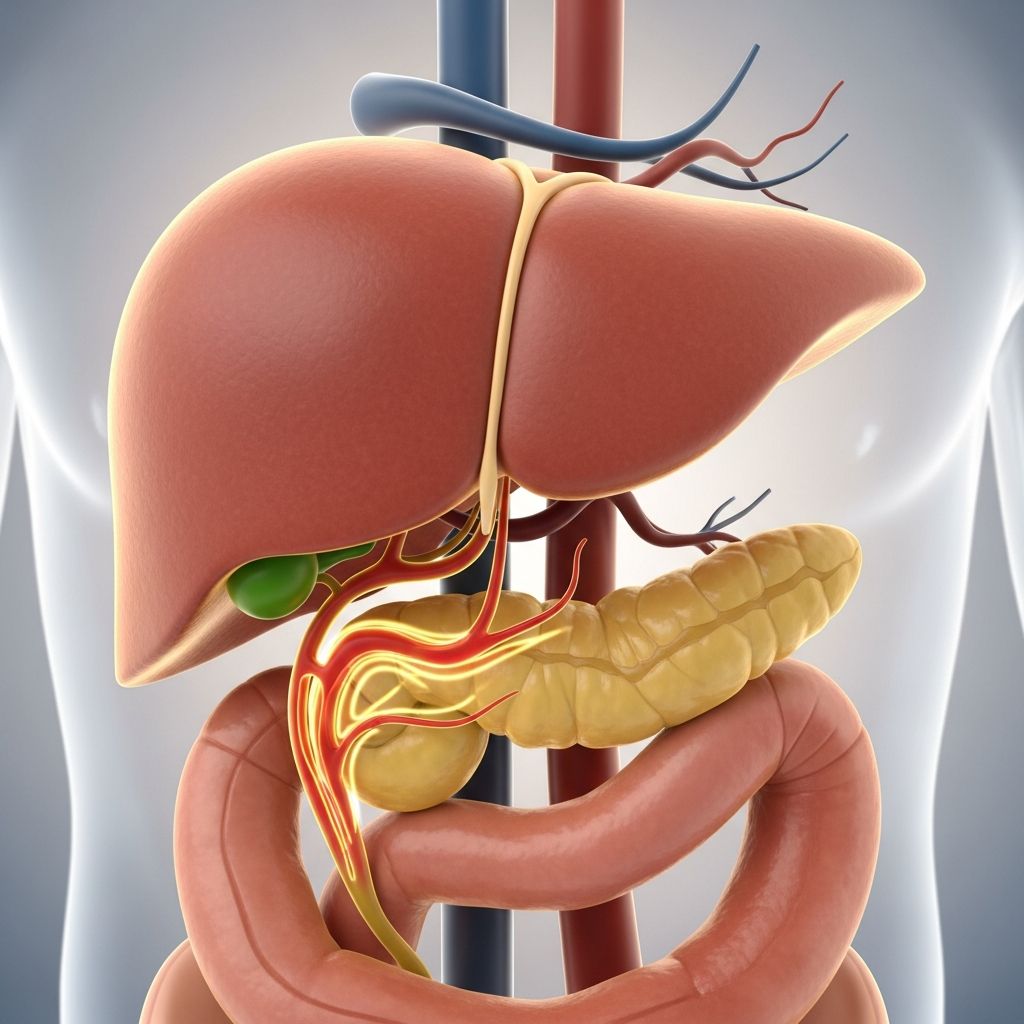
Cholestasis is a medical condition characterized by the slowing or stalling of bile flow through your biliary system. This disruption can occur at various points along the bile pathway, either within your liver itself or in your bile ducts that carry bile from the liver to the small intestine. When bile flow is compromised, bile accumulates in the liver and bloodstream, leading to a variety of symptoms and potential complications. Understanding this condition is essential for recognizing warning signs and seeking appropriate medical care.
Types of Cholestasis
Cholestasis can be classified into two main categories based on where the obstruction or dysfunction occurs:
Intrahepatic Cholestasis
Intrahepatic cholestasis refers to problems within the liver itself. This occurs when the liver cells fail to properly excrete bile into the bile ducts. Various factors can contribute to this type, including pregnancy-related hormonal changes, certain medications, viral infections, and inherited genetic conditions. The liver’s inability to process and move bile effectively results in its accumulation within liver tissue.
Extrahepatic Cholestasis
Extrahepatic cholestasis involves obstructions in the bile ducts outside the liver. Physical blockages such as gallstones, tumors, strictures, or scar tissue can prevent bile from flowing properly through the ductal system. This type of cholestasis is often more amenable to mechanical correction through medical or surgical intervention.
Common Causes of Cholestasis
Cholestasis can result from numerous underlying conditions and factors. Understanding these causes is crucial for proper diagnosis and treatment planning.
Gallstone-Related Causes
Gallstones represent one of the most common causes of cholestasis. These calcified deposits form in the gallbladder and can migrate into the bile ducts, creating physical obstructions. Conditions such as acute cholecystitis, choledocholithiasis, and acute cholangitis result from gallstone-related blockages. These conditions typically present with acute symptoms requiring prompt medical attention.
Liver Diseases
Several primary liver diseases can cause cholestasis, including primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC). These autoimmune and fibrotic conditions progressively damage bile ducts, reducing the liver’s ability to excrete bile effectively. Cirrhosis, whether from alcohol use, viral hepatitis, or other causes, can also result in cholestasis as liver function deteriorates.
Medication-Induced Cholestasis
Certain medications and substances can trigger cholestasis as an adverse effect. Drug-induced cholestasis can manifest in acute or chronic forms, ranging from bland cholestasis without inflammation to conditions with significant bile duct injury. Common culprits include anabolic steroids, estrogen-containing medications, antibiotics, and antifungal agents. Herbal supplements and over-the-counter products can also contribute to this condition.
Pregnancy-Related Cholestasis
Intrahepatic cholestasis of pregnancy (ICP) represents a unique form of cholestasis occurring during pregnancy. This condition typically emerges in the third trimester and involves hormonal influences on bile acid metabolism. While usually resolving after delivery, ICP carries implications for both maternal health and fetal well-being, requiring careful monitoring and management throughout pregnancy.
Infections and Sepsis
Bacterial infections, viral hepatitis, and other infectious processes can precipitate cholestasis. In critically ill patients, sepsis-induced cholestasis may develop as a consequence of systemic infection and inflammation. Treating the underlying infection is essential for resolving cholestasis in these cases.
Malignancies
Cancer, whether primary liver cancer or metastatic disease involving the liver, can obstruct bile flow. Hepatocellular carcinoma and cholangiocarcinoma directly affect biliary drainage, while metastatic tumors may compress bile ducts. Additionally, some cancers can cause cholestasis as a paraneoplastic syndrome without direct hepatic involvement.
Nutritional Support Complications
Total parenteral nutrition (TPN), while essential for patients unable to eat normally, can cause cholestasis. This complication typically reverses after TPN is discontinued, though prolonged use may lead to progressive liver disease.
Symptoms and Signs
The clinical presentation of cholestasis varies depending on severity and underlying cause. Patients may experience one or several characteristic symptoms:
Primary Symptoms
Jaundice, the yellowing of skin and sclera (whites of the eyes), represents one of the most visible signs of cholestasis. This occurs due to elevated bilirubin accumulation in blood and tissues. Severe itching, medically termed pruritus, affects many patients and can significantly impact quality of life, often being intractable and difficult to manage.
Gastrointestinal Symptoms
Patients commonly report nausea, vomiting, and abdominal pain or discomfort. These symptoms may vary in intensity and frequency, sometimes correlating with eating or specific triggers. Right upper quadrant pain is particularly common in conditions involving the gallbladder or bile ducts.
Metabolic and Nutritional Effects
Reduced bile flow impairs fat digestion and absorption of fat-soluble vitamins (A, D, E, and K). This can lead to nutritional deficiencies, steatorrhea (fatty stools), and vitamin deficiency symptoms. Prolonged cholestasis may result in bone health issues due to vitamin D deficiency and clotting abnormalities from vitamin K insufficiency.
Secondary Symptoms
Pale or clay-colored stools may develop due to reduced bile reaching the intestines. Dark urine can occur from elevated bilirubin being filtered by the kidneys. Fatigue and weakness often accompany prolonged cholestasis due to metabolic disturbances and nutritional deficiencies.
Diagnostic Approach
Proper diagnosis of cholestasis requires a systematic approach combining clinical evaluation, laboratory testing, and imaging studies.
Laboratory Tests
Blood tests form the foundation of cholestasis diagnosis. Elevated liver enzymes, particularly alkaline phosphatase and gamma-glutamyl transferase (GGT), indicate hepatic dysfunction. Elevated bilirubin levels correlate with jaundice severity. Liver function tests including albumin and prothrombin time assess overall liver synthetic function. Testing for specific antibodies helps identify autoimmune causes like PBC.
Imaging Studies
When blood tests suggest cholestasis, imaging studies visualize the biliary system to identify the cause. Abdominal ultrasound serves as an initial, noninvasive option that effectively shows physical obstructions in bile ducts and inflammation in organs. Computed tomography (CT) scans provide detailed cross-sectional images useful for identifying tumors or strictures. Abdominal ultrasound and CT can both indicate where problems originate in the biliary system.
Advanced Imaging
Magnetic resonance cholangiopancreatography (MRCP) has gained acceptance as a diagnostic tool, providing detailed visualization of the biliary tree without requiring endoscopic intervention. This imaging technique helps identify strictures, dilations, and other structural abnormalities characteristic of conditions like primary sclerosing cholangitis.
Endoscopic Procedures
Endoscopic retrograde cholangiopancreatography (ERCP) allows direct visualization of bile ducts through an endoscope, a tiny camera on a flexible tube inserted through the mouth. This procedure is both diagnostic and therapeutic, enabling healthcare providers to identify problems and perform interventions simultaneously. Endoscopic ultrasound may also be helpful in specific cases, particularly when standard ultrasound findings are inconclusive.
Liver Biopsy
A liver biopsy involves obtaining a small tissue sample to examine under a microscope. This test can confirm specific liver diseases, assess the degree of fibrosis or cirrhosis, and help identify certain causes of cholestasis that imaging cannot reveal. While invasive, liver biopsy remains valuable for definitive diagnosis in selected cases.
Treatment Approaches
Treatment of cholestasis focuses on addressing the underlying cause and managing symptoms. The specific approach depends on whether cholestasis is acute or chronic and what has caused it.
Addressing Underlying Causes
When medications are responsible, discontinuing the offending agent or switching to alternatives often resolves cholestasis. Infections require appropriate antibiotic or antiviral therapy. Physical obstructions can be treated through endoscopic procedures like ERCP, where healthcare providers remove blockages and open narrowed passageways using stents. Surgical intervention may be necessary for some anatomical problems or when endoscopic approaches are unsuccessful.
Symptomatic Management
For intractable itching, various medications and therapies help improve quality of life. Nutritional supplementation addresses deficiencies in fat-soluble vitamins and other nutrients. Dietary modifications may reduce gastrointestinal symptoms in some patients. Supportive care becomes particularly important in patients awaiting definitive treatment or those with conditions requiring long-term management.
Disease-Specific Treatments
Autoimmune liver diseases like PBC and PSC may require immunosuppressive or disease-modifying medications. Ursodeoxycholic acid, a naturally occurring bile acid, is commonly prescribed to improve bile flow and slow disease progression in cholestatic liver diseases. In advanced cases with cirrhosis and liver failure, liver transplantation may be necessary.
Prognosis and Outcomes
The prognosis of cholestasis depends significantly on the underlying cause and how quickly it is identified and treated. Acute cholestasis from reversible causes typically resolves completely with appropriate intervention. Chronic progressive cholestasis may require long-term management and monitoring to prevent complications including cirrhosis and liver failure. Early detection and treatment generally lead to better outcomes and reduced morbidity.
Frequently Asked Questions
Q: Can cholestasis resolve on its own?
A: Some causes of cholestasis may partially resolve independently, particularly medication-induced cholestasis after drug discontinuation or pregnancy-related cholestasis after delivery. However, most cases require medical intervention to address the underlying cause and prevent complications.
Q: Is cholestasis the same as jaundice?
A: No, cholestasis is the underlying condition affecting bile flow, while jaundice is a visible symptom of cholestasis. Jaundice can result from cholestasis, but it can also occur from other causes of elevated bilirubin in the blood.
Q: How long does it take to recover from cholestasis?
A: Recovery time varies widely depending on the cause and severity. Acute cholestasis from reversible causes may improve within weeks, while chronic conditions like primary biliary cholangitis require ongoing management potentially throughout life.
Q: Can cholestasis cause permanent liver damage?
A: Untreated or chronic cholestasis can lead to progressive liver damage, cirrhosis, and eventual liver failure. Early diagnosis and appropriate treatment are essential to prevent permanent complications.
Q: What dietary changes help with cholestasis?
A: A low-fat diet may help reduce symptoms like nausea and fatty stools. Fat-soluble vitamin supplementation (A, D, E, K) addresses nutritional deficiencies common in cholestasis. Your healthcare provider can recommend specific dietary modifications based on your situation.
Q: Is cholestasis of pregnancy dangerous?
A: Intrahepatic cholestasis of pregnancy requires careful monitoring due to potential risks to the fetus. While maternal prognosis is generally favorable, increased fetal surveillance and possible early delivery may be recommended to reduce fetal complications.
References
- Cholestasis: Definition, Symptoms, Treatment, Causes — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/diseases/24554-cholestasis
- A Comprehensive Review of Cholestasis of Pregnancy and Its Management — National Institutes of Health. 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11109475/
- Gallbladder and Biliary Tract Disease — Cleveland Clinic. 2024. https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/gallbladder-biliary-tract-disease
- Primary Biliary Cirrhosis / Primary Sclerosing Cholangitis — Cleveland Clinic. 2024. https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/primary-biliary-cirrhosis-primary-sclerosing-cholangitis
- Cholestasis Of Pregnancy: Causes, Symptoms & Treatment — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/diseases/17901-cholestasis-of-pregnancy
- Pediatric Cholestatic Liver Disease: Successful Transition of Care — Cleveland Clinic Journal of Medicine. 2019. https://www.ccjm.org/content/86/7/454
- Taming Itching in Progressive Familial Intrahepatic Cholestasis — Cleveland Clinic. 2024. https://consultqd.clevelandclinic.org/taming-itching-in-progressive-familial-intrahepatic-cholestasis
Read full bio of Sneha Tete











