Cholesterol Emboli Pathology
Detailed microscopic and clinical insights into cholesterol emboli pathology, from dermal manifestations to diagnostic challenges.
Author: Dr. Duncan Lamont, Waikato Hospital, Hamilton, New Zealand.
What is cholesterol emboli pathology?
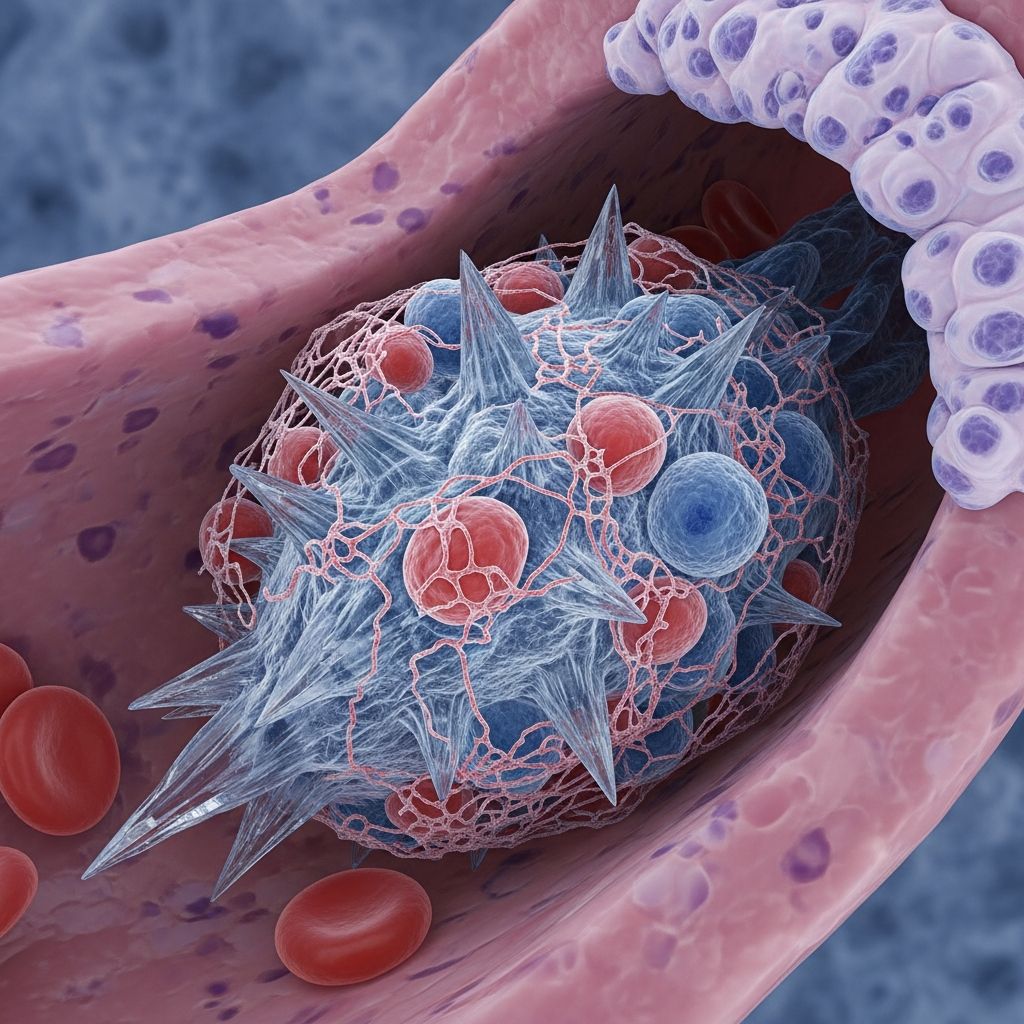
Cholesterol emboli, also known as atheroemboli, represent a critical pathological process where cholesterol crystals dislodge from atherosclerotic plaques and occlude small- to medium-sized arteries in the skin and internal organs. This phenomenon disrupts blood flow, leading to ischemia, tissue necrosis, and a cascade of inflammatory responses. Pathologically, it is characterised by the presence of needle-shaped cholesterol clefts within vessel lumens, often accompanied by fibrin thrombi and surrounding tissue damage.
The condition arises primarily from destabilisation of atheromatous plaques in large proximal arteries, such as the aorta, with emboli showering distally. While spontaneous occurrences exist, most cases are iatrogenic, precipitated by vascular interventions. Understanding the pathology is essential for dermatologists, pathologists, and clinicians managing multisystem involvement, as early recognition can prevent further embolic events.
Who gets cholesterol emboli?
Cholesterol emboli predominantly affect individuals with advanced atherosclerosis, a hallmark of generalised vascular disease. Risk factors mirror those of atherosclerosis: advanced age (typically over 50 years), male gender, Caucasian ethnicity, hypertension, diabetes mellitus, smoking history, hyperlipidaemia, obesity, and aortic aneurysms.
Precipitating events are crucial: up to 1-4% of patients undergoing vascular procedures like angiography, angioplasty, coronary artery bypass grafting (CABG), thrombolysis, or anticoagulation therapy develop cholesterol emboli syndrome (CES). Trauma to the abdominal aorta can also trigger embolisation. In hospital settings, nephrologists report CES in 5-10% of acute renal failure cases post-intervention.
Clinical features of cholesterol emboli
Cutaneous manifestations occur in over one-third of cases and serve as vital diagnostic clues. Common skin findings include:
- Livedo reticularis: A net-like purplish mottling, often on the legs, feet, or trunk, reflecting arteriolar occlusion.
- Purpura: Non-blanching purple patches due to dermal vessel thrombosis.
- Blue toe syndrome: Painful cyanotic toes from distal emboli, without large-vessel occlusion.
- Nodular lesions: Tender red-purple nodules on extremities.
- Gangrene and ulceration: In severe cases, leading to digital necrosis or skin breakdown.
Systemic involvement is frequent, forming a classic triad: livedo reticularis, acute renal failure, and eosinophilia. Other organs affected include:
- Renal: Progressive renal insufficiency, often dialysis-dependent (e.g., post-CABG renal decline over months).
- Gastrointestinal: Abdominal pain, diarrhoea, bleeding from mesenteric ischemia.
- Neurological: Transient ischaemic attacks, though stroke is rare.
- Cardiac: Myalgia, rarely infarction.
- Systemic: Fever, weight loss, myalgias mimicking vasculitis.
Laboratory hallmarks include eosinophilia (70-80% of cases, up to 4.18×10^9/L), elevated ESR, modest proteinuria/haematuria, and occasionally hypocomplementaemia.
Pathology of cholesterol emboli
Microscopically, the hallmark is biconvex, needle-shaped cholesterol clefts in arterioles and small arteries of the dermis, subcutis, and affected organs. These clefts represent dissolved cholesterol crystals post-fixation, measuring 20-50 μm in length. Surrounding features include:
- Fibrin thrombi: Often organising around clefts, contributing to occlusion.
- Endothelial damage: With mucin deposition and lymphocytic infiltrates.
- Ischemic necrosis: Extensive in dermis/subcutis, with epidermal atrophy.
- Inflammatory response: Eosinophils, giant cells, and fibrosis in chronic lesions, explaining progressive organ damage.
In renal biopsies, clefts appear in arcuate/interlobular arterioles, with distal infarction and tubular necrosis. Retinal fundoscopy may reveal visible emboli (Hollenhorst plaques). Images from Waikato Hospital demonstrate these clefts vividly in dermal vessels.
Diagnosis of cholesterol emboli
Diagnosis requires high clinical suspicion in at-risk patients post-vascular procedure with cutaneous/systemic signs. Confirmatory biopsy (skin, muscle, kidney) shows pathognomonic clefts.
| Diagnostic Modality | Key Findings | Sensitivity/Specificity |
|---|---|---|
| Skin biopsy | Cholesterol clefts in dermal arterioles + thrombi | High specificity; easiest access |
| Renal biopsy | Arteriolar clefts + infarction | Gold standard for renal CES |
| Blood tests | Eosinophilia, ↑ESR | Supportive (80% eosinophilia) |
| Imaging | Atheromatous aorta on CT | Non-specific |
Non-specific tests like complement levels are often normal. Fundoscopy or muscle biopsy aids when skin is uninvolved.
Differential diagnosis
Cholesterol emboli mimic vasculitides and other emboli:
- Other emboli: Atrial myxoma deposits, calcific emboli, IV drug contaminants, fat emboli, septic emboli, endocarditis vegetations.
- Systemic vasculitis: Polyarteritis nodosa (PAN), ANCA vasculitis – distinguished by biopsy (no clefts).
- Antiphospholipid syndrome: Thrombotic but lacks clefts.
- Cryoglobulinaemia: Similar purpura but different histology.
Biopsy differentiates definitively.
Investigations for cholesterol emboli
Usually, none beyond biopsy are required for diagnosis. Supportive tests:
- Full blood count (eosinophilia).
- ESR/CRP.
- Urinalysis (proteinuria, haematuria).
- Complement levels (often normal).
- Imaging: CT angiography for aortic plaques (avoid invasive procedures).
Management of cholesterol emboli
No curative therapy exists; focus is prevention and supportive care. Strategies include:
- Avoid precipitants: Contraindicate further angiography, anticoagulation, surgery.
- Risk factor control: Statins for hyperlipidaemia, blood pressure management.
- Symptomatic: Iloprost/prostacyclins for vasculopathy, pentoxifylline for microcirculation, steroids for inflammation (limited evidence).
- Organ support: Dialysis for renal failure.
- Prognosis: Guarded; stepwise deterioration common, mortality 30-80% in severe CES.
Prevent atherosclerosis via lifestyle and pharmacotherapy.
Frequently asked questions about cholesterol emboli pathology
Q: What are the hallmark microscopic findings?
A: Biconvex cholesterol clefts in arteriolar lumens with fibrin thrombi and ischemic necrosis.
Q: Is eosinophilia always present?
A: No, but occurs in 70-80%; highly suggestive with triad of livedo, renal failure, eosinophilia.
Q: Can cholesterol emboli occur spontaneously?
A: Yes, though rare; most follow vascular procedures or anticoagulation.
Q: How is it differentiated from vasculitis?
A: Biopsy shows clefts (absent in vasculitis); clinical context post-procedure.
Q: What is the prognosis?
A: Variable; progressive renal failure common, high mortality in multisystem disease.
Related topics
- Cholesterol emboli (view topic)
- Atheroembolism (view topic)
- Livedo reticularis (view topic)
References
- Cholesterol emboli pathology — DermNet NZ. 2023. https://dermnetnz.org/topics/cholesterol-emboli-pathology
- Cholesterol emboli syndrome — National Center for Biotechnology Information (PMC). 1999-04-24. https://pmc.ncbi.nlm.nih.gov/articles/PMC1118850/
- Cholesterol emboli — DermNet NZ. 2023. https://dermnetnz.org/topics/cholesterol-emboli
- Cholesterol emboli pathology image — DermNet NZ. 2023. https://dermnetnz.org/imagedetail/12542-cholesterol-emboli-pathology
- Cholesterol emboli syndrome following angioplasty: A case report and literature review — Cureus (Peer-reviewed). 2024. https://www.cureus.com/articles/351614-cholesterol-emboli-syndrome-following-angioplasty-a-case-report-and-literature-review
Read full bio of Sneha Tete












