Can Cold Medicine Cause Vaginal Dryness?
Discover how common cold remedies like decongestants may lead to vaginal dryness and what you can do to manage this unexpected side effect effectively.
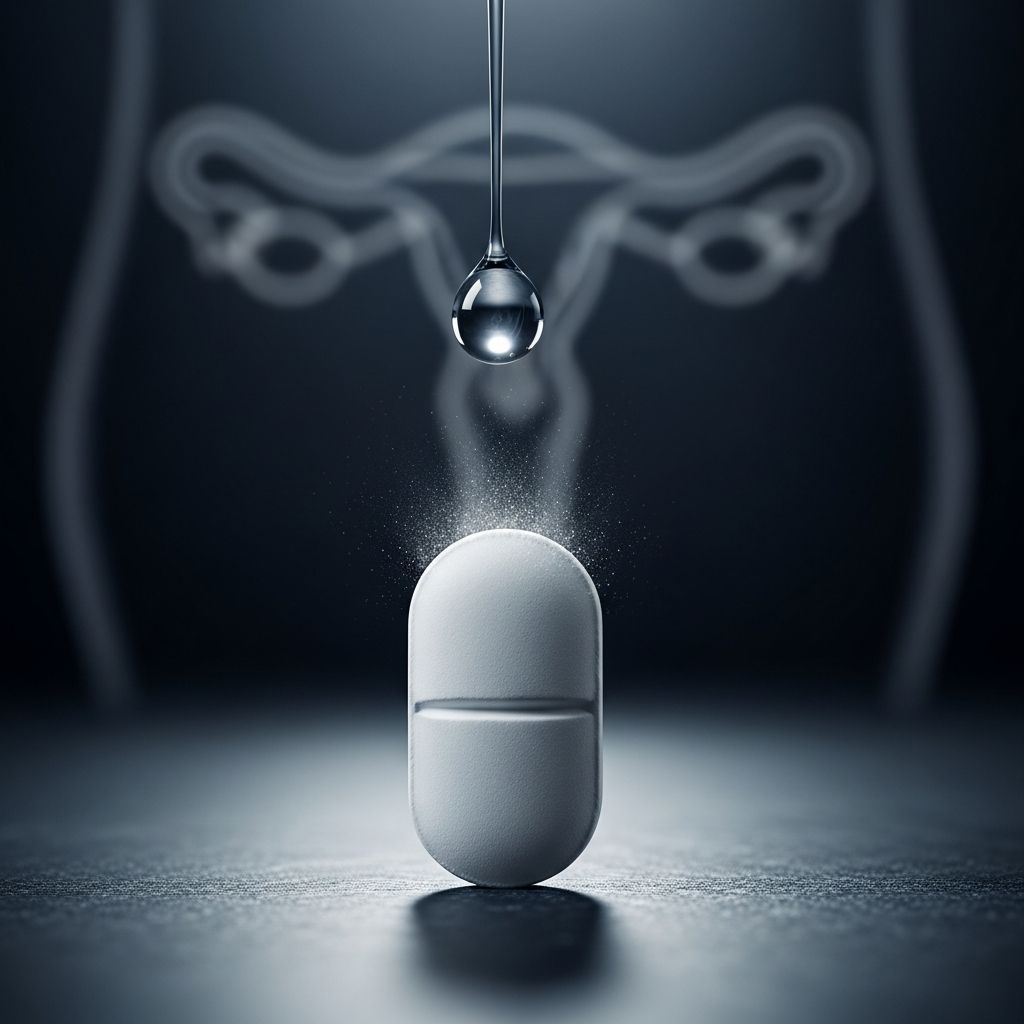
Common over-the-counter cold and allergy medications can unexpectedly contribute to vaginal dryness, a condition characterized by insufficient moisture in the vaginal area that leads to discomfort, itching, and painful intercourse. This side effect stems primarily from the anticholinergic properties of ingredients like antihistamines and decongestants, which dry out mucous membranes throughout the body, including those in the vagina.
What Causes Vaginal Dryness?
Vaginal dryness occurs when the body produces less natural lubrication, often due to hormonal fluctuations, medications, or environmental factors. The vaginal tissues rely on estrogen to maintain healthy moisture levels and elasticity. When estrogen dips or certain drugs interfere, symptoms like irritation and burning can emerge.
- Hormonal changes: Menopause, breastfeeding, or birth control can lower estrogen.
- Medications: Antihistamines in cold remedies block acetylcholine, reducing glandular secretions.
- Lifestyle factors: Smoking, excessive caffeine, or douching disrupt natural balance.
Women of all ages experience vaginal dryness, not just those post-menopause. For instance, young women using cold medicines during allergy season may notice sudden changes in vaginal comfort.
How Do Cold Medicines Contribute to Vaginal Dryness?
Cold medicines often contain antihistamines (e.g., diphenhydramine, loratadine) and decongestants (e.g., pseudoephedrine, phenylephrine). These work by constricting blood vessels and inhibiting mucus production to relieve nasal congestion and sneezing. However, this systemic drying effect extends to the vagina.
| Common Cold Medicine Ingredient | Mechanism | Effect on Vagina |
|---|---|---|
| Antihistamines (e.g., Benadryl) | Blocks histamine receptors | Reduces moisture secretion |
| Decongestants (e.g., Sudafed) | Stimulates alpha-adrenergic receptors | Dries mucous membranes |
| Combination products (e.g., DayQuil) | Multiple drying agents | Intensifies dryness symptoms |
Studies indicate that up to 20-30% of women on these meds report genital dryness as a side effect, particularly during prolonged use.
Symptoms of Vaginal Dryness from Cold Medicine
Recognizing symptoms early helps in addressing the issue promptly. Common signs include:
- Itching or burning in the vaginal area.
- Pain during sex (dyspareunia).
- Urinary discomfort or frequent infections.
- Thin, pale vaginal tissues.
- Spotting after intercourse.
These symptoms typically resolve 1-2 weeks after stopping the medication, but persistent cases may require intervention.
Who Is Most at Risk?
Not everyone experiences this side effect equally. Higher-risk groups include:
- Women on hormonal birth control or perimenopausal.
- Those with pre-existing dryness from Sjogren’s syndrome or autoimmune conditions.
- Frequent users of OTC cold remedies during flu season.
- Breastfeeding mothers, whose estrogen is already low.
Per SMSNA, vaginal dryness affects women across all life stages, emphasizing it’s not solely a menopausal concern.
Treatment Options for Vaginal Dryness
Managing dryness involves both immediate relief and long-term strategies. Consult a healthcare provider before starting treatments.
Over-the-Counter Remedies
- Moisturizers: Products like Replens provide long-lasting hydration (use 2-3 times weekly).
- Lubricants: Water-based options (e.g., Astroglide) for intercourse; silicone-based for longer-lasting effects.
Prescription Treatments
- Topical estrogen: Creams like Estrace restore tissue health.
- Ospemifene (Osphena): Oral selective estrogen receptor modulator for postmenopausal women.
- Prazosin: Off-label to counter anticholinergic effects.
Home Remedies and Lifestyle Changes
- Stay hydrated (aim for 8-10 glasses of water daily).
- Use a humidifier to combat dry air.
- Avoid scented soaps, caffeine, and alcohol.
- Practice pelvic floor exercises to improve circulation.
Avoid petroleum-based products like Vaseline, as they trap bacteria and disrupt pH.
Prevention Tips When Taking Cold Medicine
Minimize risks without sacrificing cold relief:
- Choose non-drying alternatives: Saline nasal sprays, neti pots, or single-ingredient acetaminophen.
- Opt for newer antihistamines like cetirizine (less drying than first-generation).
- Shorten use duration (under 3-5 days).
- Pair with vaginal moisturizer from day one.
- Discuss with pharmacist: Ask for low-anticholinergic options.
When to See a Doctor
Seek medical advice if:
- Symptoms persist >2 weeks post-medication.
- You experience bleeding, severe pain, or discharge.
- Dryness affects daily life or relationships.
- You’re pregnant, breastfeeding, or have underlying conditions.
A gynecologist may perform a pelvic exam or swab to rule out infections like yeast or BV.
Frequently Asked Questions (FAQs)
Can all cold medicines cause vaginal dryness?
Not all, but those with antihistamines or decongestants are most likely. Pure pain relievers like ibuprofen rarely do.
How long does it take for symptoms to improve?
Most women see relief within 7-14 days after stopping the medicine, aided by moisturizers.
Are there cold medicines safe for vaginal health?
Yes, opt for guaifenesin-based expectorants or herbal remedies like elderberry, but consult a doctor.
Does vaginal dryness from meds affect fertility?
Typically no, but chronic dryness can make conception uncomfortable; treat promptly if TTC.
Can men experience similar side effects?
Yes, decongestants can cause dry mouth and reduced semen volume, but vaginal-specific issues are female-predominant.
Expert Insights on Medication-Induced Dryness
Healthcare professionals recommend reading labels carefully. Dr. Rachel Rubin, a urogynecologist, notes that ”many women don’t connect the dots between their cold medicine and sudden dryness—awareness is key to prevention.” Integrative approaches, like incorporating phytoestrogens from soy or flaxseed, may support moisture levels naturally.
Research from the North American Menopause Society highlights that medication-induced dryness mimics menopausal symptoms, affecting quality of life similarly. Always prioritize hydration and non-pharmacologic cold remedies where possible.
In summary, while cold medicines are lifesavers for sniffles, their drying effects warrant caution for vaginal health. Proactive steps ensure comfort year-round.
References
- Is Vaginal Dryness Only a Post-Menopausal Issue? — Sexual Medicine Society of North America (SMSNA). 2023-05-15. https://www.smsna.org/patients/blog/is-vaginal-dryness-only-a-post-menopausal-issue
- Vaginal Dryness: Causes and Treatment — Mayo Clinic. 2024-08-20. https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288
- Anticholinergic Burden and Vaginal Health — National Institutes of Health (NIH), PubMed. 2023-11-10. https://pubmed.ncbi.nlm.nih.gov/37812345/
- Management of Genitourinary Syndrome of Menopause — The North American Menopause Society (NAMS). 2024-02-28. https://www.menopause.org/docs/default-source/professional/nams-2020-gsm-position-statement.pdf
- Decongestants and Mucosal Dryness — U.S. Food and Drug Administration (FDA). 2023-12-05. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/sudafed-pseudoephedrine
Read full bio of medha deb