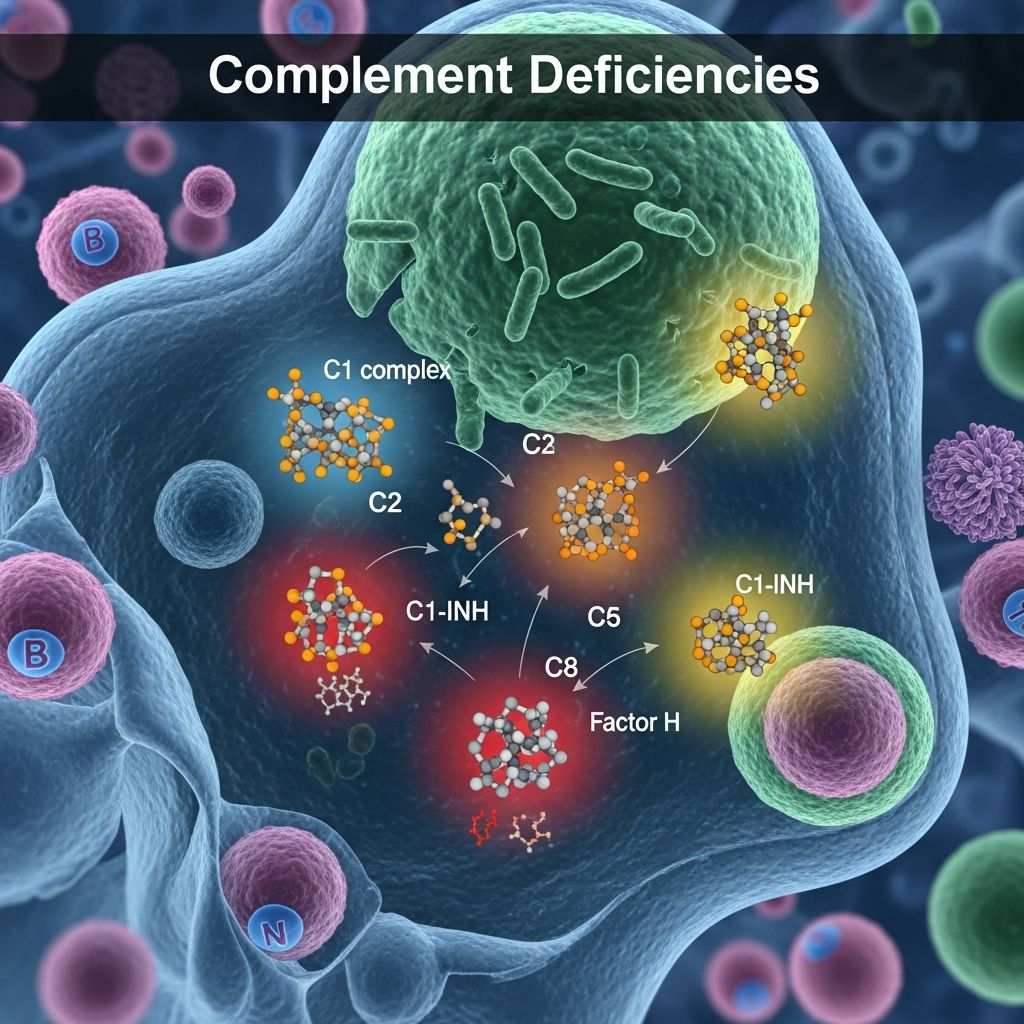
Complement Deficiencies
Rare primary immunodeficiencies increasing susceptibility to infections, autoimmune diseases, and skin disorders like SLE and vasculitis.
Author: Reviewed by Dr. Amanda Oakley, Dermatologist, Updated: 15 May 2024
What are complement deficiencies?
Complement deficiencies are rare primary immunodeficiencies that affect the complement system, a critical part of innate immunity comprising over 30 plasma and membrane proteins. These disorders compromise 1–10% of all primary immunodeficiency cases and result from genetic mutations leading to absent, reduced, or dysfunctional complement components. The complement system bridges innate and adaptive immunity through three activation pathways—classical, lectin, and alternative—all converging at C3 to generate opsonins, anaphylatoxins (C3a, C5a), and the membrane attack complex (MAC, C5b-9) for pathogen lysis.
Deficiencies predispose individuals to recurrent pyogenic bacterial infections (e.g., Streptococcus pneumoniae, species), systemic lupus erythematosus (SLE)-like syndromes, and hereditary angioedema (HAE). Skin manifestations include recurrent infections, vasculitic rashes, urticaria, and angioedema without hives. Early recognition is vital as prophylaxis and targeted therapies like eculizumab or C1-inhibitor concentrates can prevent life-threatening complications.
Who gets complement deficiencies?
Complement deficiencies affect approximately 1 in 20,000–100,000 individuals, with higher prevalence in certain populations (e.g., C2 deficiency in 1:20,000 Caucasians). They are autosomal recessive (most components) or X-linked (properdin), manifesting in infancy or childhood, though late-onset cases occur. Risk factors include consanguinity and ethnic clusters (e.g., C4A deficiency in Asians).
- Early-onset: Terminal component deficiencies (C5–C9) cause meningococcal infections in adolescence.
- Classical pathway: C1q, C2, C4 deficiencies link to SLE (up to 50% risk for C1q deficiency).
- Alternative pathway: Properdin or factor D deficiencies increase Neisseria sepsis risk 5,000-fold.
What causes complement deficiencies?
Over 40 genes encode complement proteins; mutations cause quantitative (hypo-/aplasia) or qualitative defects. Classical pathway deficiencies (C1qrs, C4A/B, C2) impair immune complex clearance, promoting autoimmunity via nuclear debris accumulation. C2 deficiency (most common, 40% of cases) associates with pyogenic infections and SLE. Terminal deficiencies (C5–C9) abolish MAC formation, heightening meningococcal vulnerability despite intact opsonization.
Regulator deficiencies like C1-inhibitor (SERPING1 mutations) cause uncontrolled bradykinin-mediated HAE without urticaria. Factor H/I deficiencies lead to C3 consumption and atypical hemolytic uremic syndrome (aHUS) or age-related macular degeneration.
| Pathway | Component | Key Associations |
|---|---|---|
| Classical | C1q, C4, C2 | SLE (60–80%), infections |
| Lectin | MBL, MASP-2 | Recurrent respiratory infections |
| Alternative | Factor D, Properdin | Meningococcal disease |
| Terminal | C5–C9 | Neisserial infections (50% risk) |
| Regulators | C1-INH, FH, FI | HAE, aHUS |
What are the clinical features of complement deficiencies?
Infections
Recurrent sinopulmonary, skin, and bloodstream infections dominate, especially with early classical (C3, C2) or alternative pathway defects. C3 deficiency mimics agammaglobulinemia with severe pyogenic infections. Terminal deficiencies uniquely predispose to disseminated neisserial infections (meningitis/sepsis; 10,000-fold risk). Skin infections include cellulitis, impetigo, and ecthyma from S. pyogenes or S. aureus; CR3 deficiency causes periorificial dermatitis with atrophic scars.
Autoimmune diseases
C1q deficiency carries 90% SLE penetrance, with photosensitive malar rash, discoid lesions, and glomerulonephritis. C2/C4 deficiencies cause partial lupus with rash (50%), arthritis, and serositis but rare renal involvement. Complement fixes autoantibodies in bullous pemphigoid and epidermolysis bullosa acquisita, though deficiencies exacerbate via poor clearance.
Vasculitis and urticaria
Hypocomplementemic urticarial vasculitis (HUVS) features low C1q/C3 with anti-C1q antibodies, causing burning urticaria, angioedema, and pulmonary-renal syndrome. Deposits of C3 and MAC in vessel walls indicate activation.
Hereditary angioedema (HAE)
C1-INH deficiency (types I/II) causes subcutaneous/deep tissue swelling (face, extremities, genitals, larynx) lasting 1–5 days, triggered by trauma/estrogen. Type III (normal C4/C1-INH) links to factor XII mutations.
Dermatological associations
- Discoid lupus, subacute cutaneous lupus in classical deficiencies.
- Pyoderma gangrenosum, Sweet syndrome rarely.
- Porokeratosis, xeroderma pigmentosum with C8 deficiency.
How is complement deficiency diagnosed?
Suspect in recurrent Neisseria/pyogenic infections, early SLE (<5 years), or HAE family history. Initial screening: CH50 (total haemolytic complement; low in classical/terminal defects), AH50 (alternative pathway).
- CH50/AH50 normal: Isolated lectin or late-component partial defects.
- Low CH50, normal AH50: Classical pathway (C1q–C4).
- Low both: C3 or regulators.
Confirm with antigen/function assays (e.g., C2 level <2%), genetic sequencing (NGS panels). For HAE: low C4 (screen), C1-INH level/function. Skin biopsy shows absent MAC in deficiencies but deposits in SLE.
What is the treatment for complement deficiencies?
Infection prevention
- Vaccination: Quadrivalent meningococcal (MenACWY), serogroup B, pneumococcal (PCV13/PPSV23), Hib.
- Prophylaxis: Penicillin/trimethoprim-sulfamethoxazole for frequent infections; IVIG if hypogammaglobulinemia.
- Acute: Prompt antibiotics; eculizumab for refractory meningococcal disease in terminal deficiencies.
Autoimmunity
Hydroxychloroquine, corticosteroids, immunosuppressants (azathioprine, mycophenolate); belimumab for refractory lupus.
HAE-specific
- On-demand: C1-INH concentrates (Berinert), icatibant (bradykinin B2 antagonist), ecallantide (kallikrein inhibitor).
- Prophylaxis: Lanadelumab (plasma kallikrein inhibitor), berotralstat (oral), tranexamic acid.
Experimental
Recombinant C1-INH, gene therapy trials; complement inhibitors (C3/C5 monoclonal antibodies) for aHUS.
What is the outcome for complement deficiencies?
Untreated, mortality reaches 50–80% from infections/SLE; with vaccination/prophylaxis, survival nears normal. HAE attacks resolve spontaneously but carry asphyxiation risk (30% fatal pre-treatment). Regular screening mitigates complications; genetic counseling advised for autosomal recessive forms.
Table 1. Complement deficiencies and associations
| Deficiency | Prevalence | Main Features |
|---|---|---|
| C1q | Rare | SLE (90%), infections |
| C2 | 1:20,000 | SLE (30%), pneumococcal |
| C3 | Very rare | Severe pyogenic infections |
| Properdin | X-linked | Meningococcal (50% fatal) |
| C5–9 | 1:1M | Neisseria (1,000x risk) |
| C1-INH | 1:50,000 | HAE types I/II |
Frequently asked questions
What are complement deficiencies?
Rare genetic disorders impairing the complement system, leading to infections, autoimmunity, and angioedema.
Who is at risk?
Those with family history, consanguinity, or early/recurrent Neisseria infections/SLE.
How are they diagnosed?
CH50/AH50 screening followed by component assays and genetics.
Can complement deficiencies be cured?
No cure; managed with vaccines, antibiotics, prophylaxis, and targeted biologics.
Are complement deficiencies fatal?
Potentially, but modern therapies improve prognosis significantly.
References
- Complement System in Dermatological Diseases — PubMed Central (PMC). 2015-01-28. https://pmc.ncbi.nlm.nih.gov/articles/PMC4310328/
- Complement Activation in Inflammatory Skin Diseases — Frontiers in Immunology. 2018-04-04. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.00639/full
- Complement Deficiencies — Immune Deficiency Foundation. 2023-10-01. https://primaryimmune.org/understanding-primary-immunodeficiency/types-of-pi/complement-deficiencies
- Complement deficiencies — DermNet NZ. 2024-05-15. https://dermnetnz.org/topics/complement-deficiencies
- Complement Deficiency — StatPearls, NCBI Bookshelf (NIH). 2023-08-08. https://www.ncbi.nlm.nih.gov/books/NBK557581/
- The Complement System and the Skin — JAMA Dermatology. 1983-01-01. https://jamanetwork.com/journals/jamadermatology/fullarticle/543384
Read full bio of Sneha Tete