6 Things to Know About Complementary Approaches for Seasonal Allergy Relief
Explore evidence-based complementary approaches to manage seasonal allergies naturally and effectively.

6 Things To Know About Complementary Health Approaches for Seasonal Allergy Relief
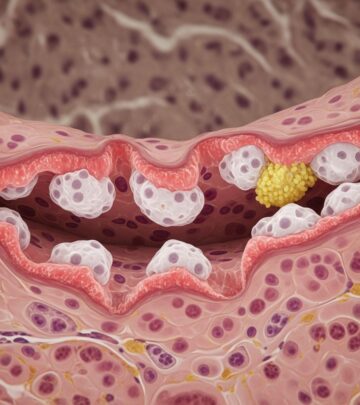
Seasonal allergies, commonly referred to as hay fever or allergic rhinitis, affect millions of people each spring, summer, and fall when trees, weeds, and grasses release pollen into the air. When this pollen reaches your nose and throat, it can trigger uncomfortable symptoms including sneezing, runny nose, coughing, and itchy eyes and throat. Traditional management strategies for seasonal allergies typically include taking medications, avoiding exposure to allergens, or undergoing immunotherapy in the form of allergy shots. However, many people are exploring complementary health approaches as additional tools to manage their allergy symptoms effectively.
If you are considering any complementary health approach for the relief of seasonal allergy symptoms, here are six important things you need to know before making your decision.
1. Nasal Saline Irrigation: A Well-Supported Natural Approach
Nasal saline irrigation, a practice where salt water is gently flushed through one nostril and drained out the other, has emerged as one of the most researched and supported complementary approaches for seasonal allergies. This simple yet effective technique offers a drug-free method to manage allergy symptoms.
There is solid scientific evidence demonstrating that saline nasal irrigation can provide modest improvement of allergy symptoms. A comprehensive systematic review and meta-analysis of 10 studies found that saline nasal irrigation administered regularly over a period of up to 7 weeks produced beneficial effects on nasal symptoms, reduced medicine consumption, improved mucociliary clearance time, and enhanced quality of life in both adults and children with allergic rhinitis. Another 2012 review of nasal saline irrigation in the management of sinonasal disease confirmed that nasal saline irrigation demonstrates modest clinical benefits for allergy sufferers.
The procedure is generally safe and well-tolerated by most people. Common devices used for nasal saline irrigation include neti pots, which originate from the Ayurvedic tradition, as well as modern alternatives such as nebulizers, spray bottles, pump bottles, or squeeze bottles. However, proper use and maintenance of these devices is crucial for safety and effectiveness. It is essential to use sterile or distilled water, follow manufacturer instructions carefully, and clean devices thoroughly after each use to prevent infection.
Key Benefits:
- Reduces nasal congestion and stuffiness
- Decreases medication requirements
- Improves quality of life
- Generally safe when used properly
- Non-invasive and drug-free
- Can be used alongside conventional treatments
2. Butterbur Extract: Herbal Support for Allergy Symptoms
Butterbur, a plant native to Europe and Asia, has been used traditionally in herbal medicine and has gained scientific attention for its potential role in managing allergic rhinitis. The active compounds in butterbur are believed to have anti-inflammatory and antihistamine properties.
A 2007 evaluation of six studies examining butterbur extract for allergic rhinitis, which involved a total of 720 participants, indicated that butterbur may be helpful for reducing seasonal allergy symptoms. The research suggests that butterbur extract may work by reducing inflammation in the nasal passages and modulating immune responses to allergens.
While butterbur shows promise, it is important to note that not all natural products labeled as butterbur are equally effective. The most studied form is butterbur extract standardized to contain petasins, the active compounds responsible for its therapeutic effects. When considering butterbur supplementation, it is crucial to choose products from reputable manufacturers that have undergone quality testing. Additionally, individuals with allergies to ragweed, chrysanthemums, or daisies should exercise caution, as these plants are related to butterbur and may cause cross-reactions.
Important Considerations:
- Look for standardized extracts containing petasins
- May interact with certain medications
- Should be obtained from reputable manufacturers
- Not recommended for pregnant or nursing women
- Consult healthcare providers before use
3. Honey: The Popular Yet Unproven Remedy
Local honey is frequently recommended as a natural remedy for seasonal allergies, based on the theory that consuming small amounts of local pollen through honey may help build immunity to these allergens. This folk remedy has gained significant popularity, particularly on social media and among wellness communities.
However, it is important to understand that there is no convincing scientific evidence demonstrating that honey relieves seasonal allergies. The available data on the efficacy of honey for seasonal allergy symptoms consist of only a few randomized controlled trials, which limits the strength of conclusions that can be drawn.
One 2011 randomized controlled pilot study of 44 patients with physician-diagnosed birch pollen allergy found that patients who used pre-seasonal birch pollen honey had significantly better control of their symptoms compared to those on conventional allergy medication, and marginally better control compared to those using regular honey. However, these results should be regarded as preliminary and have not been consistently replicated in subsequent research. The small sample size and limited number of studies make it difficult to draw firm conclusions about honey’s effectiveness.
While honey may not be an effective treatment for seasonal allergies, it does offer other health benefits and is generally safe for most adults. The key takeaway is that honey should not be relied upon as a primary treatment for seasonal allergies, though it can be enjoyed as part of a balanced diet while managing allergies through other proven methods.
What the Evidence Shows:
- Limited scientific evidence supports honey for allergy relief
- Most studies are small and preliminary
- Local honey theory lacks robust scientific support
- May have other health benefits for general wellness
- Should not replace proven allergy treatments
4. Acupuncture: Ancient Practice With Modern Scientific Support
Acupuncture, a cornerstone of traditional Chinese medicine, involves the insertion of thin needles into specific points on the body. This practice has been used for thousands of years and is increasingly being studied for its effects on various health conditions, including allergic rhinitis.
A 2015 systematic review and meta-analysis of 13 studies involving a total of 2,365 participants found evidence that acupuncture may be helpful for allergic rhinitis. Compared with a control group, the acupuncture treatment group showed significant reductions in nasal symptom scores, medication scores, and serum IgE levels, along with an increase in quality of life scores. These findings suggest that acupuncture may work through multiple mechanisms to reduce allergic responses.
The clinical importance of acupuncture for allergy management was recognized by the American Academy of Otolaryngology in their 2015 clinical practice guidelines, which included the recommendation that clinicians may offer acupuncture or refer patients to qualified practitioners for those with allergic rhinitis who are interested in nonpharmacologic therapy options.
When considering acupuncture for seasonal allergies, it is essential to work with a licensed and qualified practitioner who has specific experience treating allergic rhinitis. The practitioner should explain their treatment approach and the expected number of sessions needed. Some people experience improvement in symptoms within a few sessions, while others may require more extended treatment courses.
Key Findings:
- Supported by 2015 meta-analysis of 2,365 participants
- Reduces nasal symptom scores and medication use
- Improves quality of life scores
- Recognized by mainstream medical organizations
- Requires qualified, licensed practitioners
- May be particularly suitable for those avoiding medications
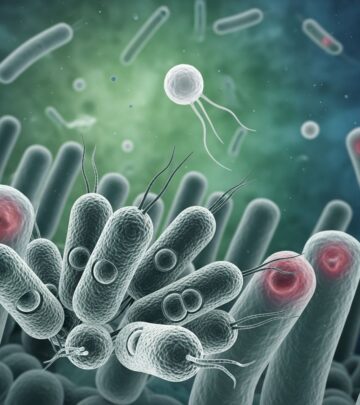
5. Probiotics: Emerging Science With Mixed Results
Probiotics are live microorganisms that may have health benefits, particularly for immune system function. Researchers have been investigating probiotics for diseases of the immune system, including allergies, based on evidence that gut microbiota composition may influence allergic responses.
There is some limited evidence suggesting that probiotics may improve some symptoms and quality of life in people with allergic rhinitis. However, the overall data on probiotics and allergic rhinitis remains inconsistent, making it difficult to make firm conclusions about effectiveness. A 2013 randomized controlled trial of 60 patients with allergic rhinitis examined the effects of probiotic consumption (Lactobacillus casei Shirota) on clinical and immunological parameters of seasonal allergic rhinitis. Results showed that daily oral supplementation with L. casei Shirota modified some parameters of allergic inflammation at the nasal mucosa, though there were no significant changes in clinical symptoms of seasonal allergic rhinitis.
One major challenge in evaluating probiotics is that formulations vary significantly from study to study. Different strains of bacteria, different dosages, and different delivery methods all produce different results. Some types of probiotics might be helpful for allergic rhinitis, while others may not be effective. This variability makes it difficult for consumers to know which products might work for their specific situation.
Current Understanding:
- Limited evidence for allergic rhinitis benefit
- Results are inconsistent between studies
- Effectiveness varies by strain and formulation
- More research is needed
- Individual responses may vary
- Consult healthcare providers before use
6. Talk to Your Healthcare Provider
Perhaps the most important recommendation is to discuss any complementary health approach with your healthcare provider before starting treatment. Your healthcare provider can help you evaluate the evidence, consider potential interactions with other medications or conditions, and determine the best ways to manage your specific allergy symptoms.
Your healthcare provider may also suggest practical strategies alongside complementary approaches to manage seasonal allergies more effectively. When the pollen count is high, staying indoors when possible, wearing protective masks outdoors, and rinsing off clothing and washing hair when you come inside can help reduce allergen exposure. Air filtration systems with HEPA filters can also help reduce indoor pollen levels.
The combination of complementary approaches with conventional treatments, environmental modifications, and professional medical guidance typically provides the most comprehensive approach to managing seasonal allergies.
Understanding Seasonal Allergies Better
Seasonal allergies occur when your immune system overreacts to pollen particles that are otherwise harmless. Your immune system treats the pollen as a threat and releases histamine and other chemicals, which cause the characteristic allergy symptoms. The severity of seasonal allergies can vary from year to year depending on pollen counts, weather patterns, and individual immune system sensitivity.
Traditional treatments include antihistamines, decongestants, corticosteroid nasal sprays, and in some cases, immunotherapy. Complementary approaches should ideally complement these conventional treatments rather than replace them entirely, though some people find they can reduce their medication use when combining approaches.
Comparing Complementary Approaches for Seasonal Allergies
| Approach | Evidence Level | Safety Profile | Cost |
|---|---|---|---|
| Nasal Saline Irrigation | Good Evidence | Very Safe | Low |
| Butterbur Extract | Moderate Evidence | Generally Safe | Moderate |
| Honey | Limited Evidence | Safe | Low |
| Acupuncture | Good Evidence | Safe (when qualified) | Moderate-High |
| Probiotics | Limited Evidence | Generally Safe | Moderate |
Frequently Asked Questions
Q: Can I use complementary approaches instead of my allergy medications?
A: While some complementary approaches show promise, they should not immediately replace your allergy medications without consulting your healthcare provider. Many people find the best results by combining complementary approaches with conventional treatments. Your doctor can help you determine if and when it might be appropriate to adjust your medication regimen.
Q: How long does it typically take to see results from complementary approaches?
A: Results vary depending on the approach. Nasal saline irrigation may provide relief within the first few uses. Herbal supplements like butterbur and acupuncture may take weeks before noticeable improvement. Probiotics may require several weeks to months of consistent use. It’s important to give treatments adequate time while monitoring for effectiveness.
Q: Are there any complementary approaches I should avoid?
A: While most complementary approaches for seasonal allergies are safe when used properly, some may interact with medications or be contraindicated for certain health conditions. This is why consulting with your healthcare provider is essential before starting any new treatment, especially if you take other medications or have underlying health conditions.
Q: Can children use these complementary approaches?
A: Some complementary approaches, like nasal saline irrigation, are safe for children. However, age-appropriate dosages and formulations are important for herbal supplements, and acupuncture should only be performed by practitioners experienced in treating pediatric patients. Always consult your child’s healthcare provider before starting complementary treatments.
Q: Where can I find qualified practitioners for acupuncture or other complementary approaches?
A: Look for licensed and certified practitioners in your area. Many states regulate acupuncturists, requiring specific credentials and licensing. Ask your healthcare provider for referrals, check professional organizations for qualified practitioners, and verify credentials before beginning treatment.
Making Your Decision
When considering complementary health approaches for seasonal allergy relief, take time to review the scientific evidence for each option. Nasal saline irrigation and acupuncture have the strongest evidence supporting their use. Butterbur shows moderate promise, while honey’s effectiveness remains unproven. Probiotics show some potential but require more research.
Consider your individual circumstances, preferences, and health status. Some approaches may work better for you than others based on your specific allergy triggers and response patterns. Remember that complementary approaches work best when combined with conventional treatments, environmental modifications, and guidance from qualified healthcare providers.
By taking an informed, evidence-based approach and working closely with your healthcare team, you can develop a comprehensive strategy for managing seasonal allergies that maximizes symptom relief while minimizing side effects.
References
- Seasonal Allergies and Complementary Health Approaches: What the Science Says — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024-11-15. https://www.nccih.nih.gov/health/providers/digest/seasonal-allergies-and-complementary-health-approaches-science
- Hermelingmeier KE, Weber RK, Hellmich M, et al. Nasal irrigation as an adjunctive treatment in allergic rhinitis: a systematic review and meta-analysis — American Journal of Rhinology & Allergy. 2012-09-01. https://pubmed.ncbi.nlm.nih.gov/23168148/
- Seasonal Allergies at a Glance — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024-11-15. https://www.nccih.nih.gov/health/seasonal-allergies-at-a-glance
- 6 Things To Know About Complementary Health Approaches for Seasonal Allergy Relief — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024-11-15. https://www.nccih.nih.gov/health/tips/things-to-know-about-complementary-health-approaches-for-seasonal-allergy-relief
- Ivory K, Wilson AM, Sankaran P, et al. Oral delivery of a probiotic induced changes at the nasal mucosa of seasonal allergic rhinitis subjects after local allergen challenge: a randomised clinical trial — International Forum of Allergy & Rhinology. 2015-06-01. https://pubmed.ncbi.nlm.nih.gov/25877024/
- Seasonal Allergies and Complementary Health Practices — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024-11-15. https://content.govdelivery.com/accounts/USNIHNCCIH/bulletins/13b4713
Read full bio of medha deb