Congenital Heart Defect: Causes, Symptoms, Treatment Guide
Understanding congenital heart defects: causes, symptoms, diagnosis, treatment, and living with CHD for better outcomes.
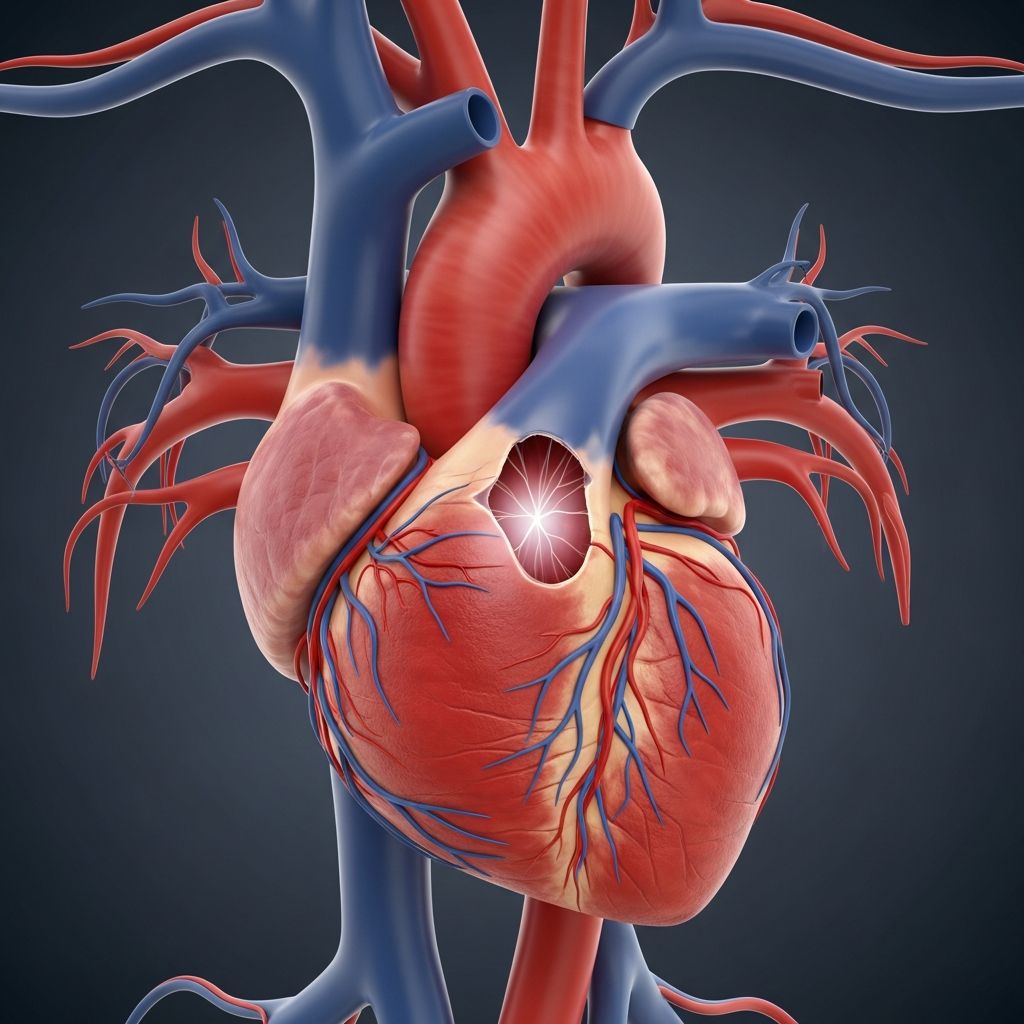
Congenital Heart Defect
Congenital heart defects (CHD), also known as congenital heart disease, represent the most common birth defects worldwide, affecting approximately 1% of newborns or about 40,000 infants annually in the United States alone. These structural abnormalities in the heart or major blood vessels occur during fetal development, often in the first six weeks of pregnancy when the heart is forming.
CHDs range from mild defects that may resolve without intervention to severe conditions requiring immediate surgery. Advances in pediatric cardiology have dramatically improved survival rates, exceeding 98% with proper treatment, allowing many children to lead full lives. However, lifelong monitoring is often necessary to manage complications like heart failure or arrhythmias.
What Is a Congenital Heart Defect?
A
congenital heart defect
arises when the heart or nearby blood vessels fail to develop properly before birth, typically due to errors in embryonic heart formation shortly after conception. The heart begins as a simple tube around week three of pregnancy, dividing into chambers and developing valves and vessels by week six. Disruptions during this critical window lead to malformations affecting blood flow, oxygenation, or heart function.Common issues include holes between heart chambers, malformed valves, or misplaced great arteries. Simple defects like small atrial septal defects (ASD) may cause minimal symptoms, while complex ones like hypoplastic left heart syndrome demand urgent care. Not all CHDs manifest at birth; some are detected prenatally via ultrasound or later in childhood/adulthood.
Symptoms of Congenital Heart Defects
Symptoms vary by defect severity and type. Mild CHDs may be asymptomatic, discovered incidentally. Severe cases present in newborns with:
- Rapid or difficulty breathing, especially during feeding.
- Poor weight gain or failure to thrive.
- Cyanosis (bluish skin, lips, nails) from low oxygen.
- Fatigue, irritability, or sweating while eating.
- Swelling in legs, belly, or around eyes.
In older children, signs include shortness of breath during activity, frequent respiratory infections, or clubbing of fingers/toes. Adults with undiagnosed mild CHDs might experience arrhythmias, fatigue, or heart failure later in life. Prompt recognition is crucial, as untreated severe defects can lead to congestive heart failure or stroke.
Causes of Congenital Heart Defects
The exact cause of most CHDs remains unknown, but they result from a complex interplay of genetic, environmental, and lifestyle factors during early pregnancy. Key contributors include:
- Genetic factors: Chromosomal abnormalities (e.g., Down syndrome) or gene mutations increase risk threefold if a parent or sibling has CHD.
- Maternal conditions: Diabetes, obesity, phenylketonuria (PKU), or infections like rubella.
- Medications/teratogens: Certain drugs (e.g., isotretinoin), smoking, alcohol, or illicit substances.
- Environmental exposures: Radiation or high altitudes.
Researchers emphasize that while genetics play a role, most cases are multifactorial without a single identifiable cause.
Risk Factors for Congenital Heart Defects
Identified risk factors heighten CHD likelihood:
| Risk Factor | Description |
|---|---|
| Family history | 3x higher risk if first-degree relative affected. |
| Maternal diabetes | Poorly controlled blood sugar disrupts fetal heart development. |
| Advanced maternal age (>40) | Increased chromosomal issues. |
| Smoking/alcohol | Toxins impair embryogenesis. |
| Prior CHD-affected pregnancy | Recurrence risk up to 10%. |
Preventive steps like preconception counseling, folic acid supplementation (400-800 mcg daily), and avoiding teratogens can mitigate risks.
Types of Congenital Heart Defects
Over 40 types exist, categorized by affected structure. Common ones include:
- Septal defects: Atrial septal defect (ASD) – Hole in upper chambers; Ventricular septal defect (VSD) – Hole in lower chambers, often closing spontaneously.
- Valve issues: Bicuspid aortic valve – Aortic valve with two cusps; Aortic stenosis – Narrowed valve; Pulmonary atresia – Absent pulmonary valve.
- Obstructions: Coarctation of the aorta (CoA) – Narrowed aorta.
- Complex: Tetralogy of Fallot – Four defects causing cyanosis; Transposition of great arteries (TGA) – Switched main arteries; Hypoplastic left heart syndrome – Underdeveloped left side; Tricuspid atresia – Absent tricuspid valve.
- Other: Atrioventricular canal defect, Double-outlet right ventricle, Ebstein anomaly.
Each impacts blood flow differently, dictating symptoms and treatment.
Diagnosis of Congenital Heart Defects
Diagnosis often starts prenatally via fetal echocardiography (week 18-24 ultrasound). Postnatally:
- Echocardiogram (echo): Gold standard, using sound waves for detailed heart images.
- Chest X-ray/ECG: Assess heart size, rhythm, lung status.
- Pulse oximetry: Screens newborns for low oxygen.
- Cardiac MRI/CT catheterization: For complex cases.
Early detection enables timely intervention.
Treatment for Congenital Heart Defects
Treatment depends on severity:
- Monitoring: Small VSDs/ASD may close naturally.
- Medications: Diuretics, ACE inhibitors for heart failure; anticoagulants for clots.
- Catheter procedures: Device closure for septal defects.
- Surgery: Repair (e.g., patch holes, valve replacement) or palliation (staged for single ventricle). About 25% of CHDs need surgery.
Multistage repairs for complex defects like HLHS occur in infancy/childhood.
Complications of Congenital Heart Defects
Even post-treatment, risks persist:
- Heart failure/arrhythmias: From overworked heart.
- Endocarditis: Infection risk; antibiotic prophylaxis for procedures.
- Stroke/clots: From abnormal flow.
- Developmental delays: Due to hypoxia or chronic illness.
- Mental health: Anxiety from restrictions.
Regular cardiology follow-up is essential.
Living With Congenital Heart Defects
Most children thrive post-treatment, but require:
- Lifelong cardiology care.
- Activity guidelines (avoid contact sports if advised).
- Infection prevention (dental hygiene, endocarditis prophylaxis).
- Healthy lifestyle: Balanced diet, exercise, no smoking.
- Education support for potential learning issues.
Survival >98%, but 10-15% need reinterventions.
Frequently Asked Questions (FAQs)
Can congenital heart defects be prevented?
No guaranteed prevention, but folic acid, diabetes control, avoiding smoking/alcohol, and genetic counseling reduce risks.
Do all CHDs require surgery?
No; mild ones like small VSDs often resolve without intervention. About 1 in 4 needs surgery.
What is the prognosis for CHD?
Excellent with treatment—98%+ survival. Many lead normal lives, though monitoring continues.
Are CHDs hereditary?
Partly; family history triples risk, but most are sporadic.
When are CHDs diagnosed?
Prenatally (echo), at birth (oximetry), or later via symptoms/exams.
References
- About Congenital Heart Defects — American Heart Association. 2023. https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects
- Congenital heart defects in children – Symptoms and causes — Mayo Clinic. 2024-01-12. https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/symptoms-causes/syc-20350074
- Congenital Heart Defects in Newborns — American Academy of Pediatrics (HealthyChildren.org). 2023. https://www.healthychildren.org/English/health-issues/conditions/heart/Pages/Common-Heart-Defects.aspx
- Managing congenital heart disease — Children’s Health. 2024. https://www.childrens.com/health-wellness/managing-congenital-heart-disease
- Exploring Health Educational Interventions for Children With Congenital Heart Disease — National Library of Medicine (PMC). 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11806270/
Read full bio of Sneha Tete












