Cutaneous Lymphadenoma: Disease Pathology
Comprehensive pathology guide to cutaneous lymphadenoma, a rare benign adnexal tumor with distinctive lymphoepithelial features.
Cutaneous lymphadenoma, also known as benign lymphoepithelial tumor of the skin, is a rare benign adnexal neoplasm characterized by basaloid epithelial lobules infiltrated by lymphocytes and histiocytes. This tumor primarily affects the head and neck, presenting as a small, asymptomatic nodule, and requires complete excision for cure.
Introduction
Cutaneous lymphadenoma (CL) represents a distinctive cutaneous adnexal tumor first described in 1987 by Santa Cruz and Barr as a ‘benign lymphoepithelial tumor of the skin.’ It was later renamed ‘cutaneous lymphadenoma’ in 1991, reflecting its lymphoid-rich histology despite lacking true lymph node-like architecture. Fewer than 60 cases have been documented in the literature, underscoring its rarity. Clinically, it manifests as a solitary, skin-colored to reddish papule or nodule, typically 0.5-1.5 cm in diameter, on the head and neck of adults aged 20-75 years, with no sex predilection.
Despite its benign nature, CL often elicits a clinical suspicion of basal cell carcinoma (BCC) or cutaneous lymphoma due to its location and infiltrative lymphoid appearance. Histogenesis remains debated, with proposals linking it to follicular (trichoblastic), sebaceous, or eccrine differentiation. Recent views favor it as an adamantinoid trichoblastoma variant with prominent lymphoepithelial features. Complete surgical excision is curative, though incomplete removal, such as via shave biopsy, may lead to recurrence.
Clinical Features
Patients typically present with a slowly enlarging, non-ulcerated nodule on sun-exposed areas, most commonly the face (forehead, cheek, nose), followed by scalp or neck. Lesions are asymptomatic, firm, and dome-shaped, measuring 3-15 mm. The overlying skin may appear stretched or telangiectatic but rarely ulcerates. Age at diagnosis ranges from 21 to 75 years (mean ~50), affecting males and females equally.
- Key clinical characteristics:
- Solitary lesion (rarely multiple)
- Skin-colored or erythematous papule/nodule
- Head and neck predominance (90% of cases)
- Slow growth over months to years
- No systemic symptoms or lymphadenopathy
Differential clinical diagnoses include BCC, trichoepithelioma, syringoma, or metastatic carcinoma. Recurrence after incomplete excision has been reported, as in a case of forehead CL recurring 2 years post-shave biopsy.
Histopathology
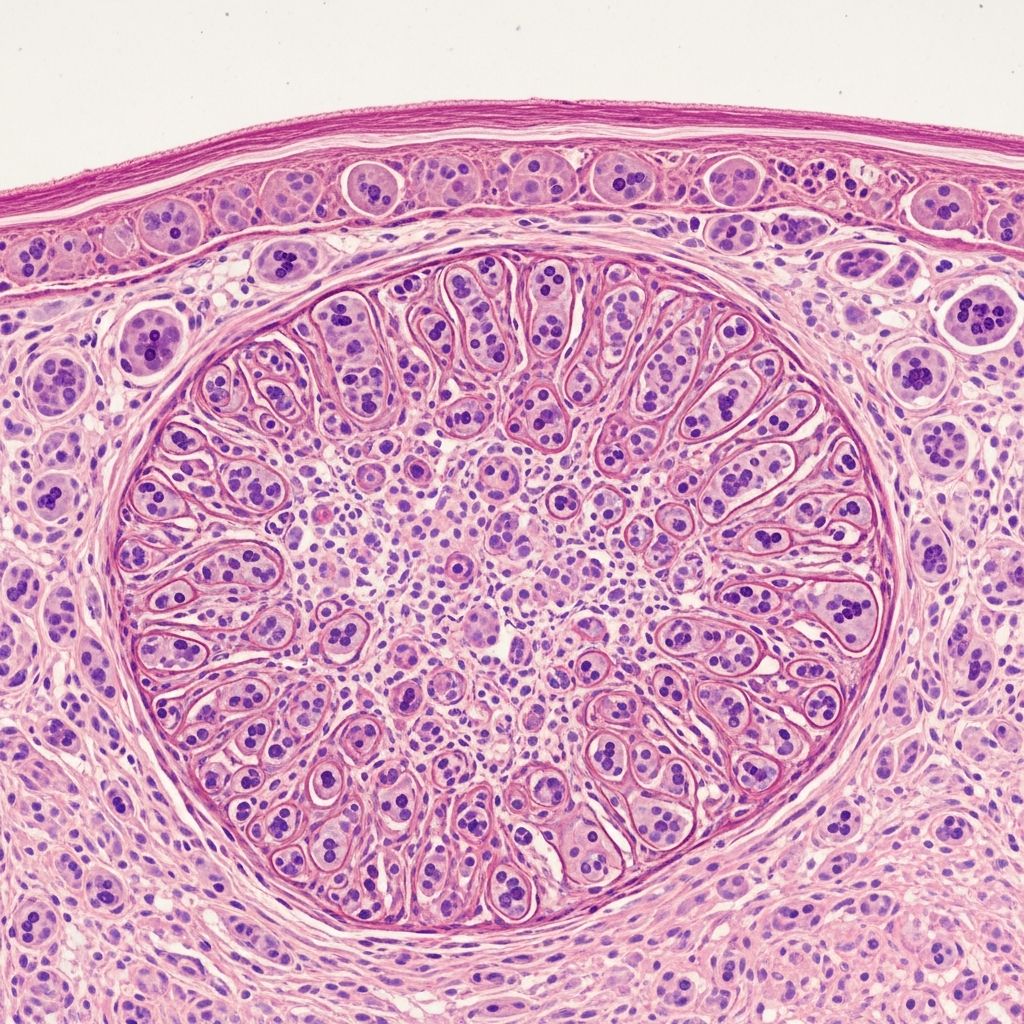
Microscopically, CL appears as a well-circumscribed, non-encapsulated dermal nodule composed of irregular lobules, islands, and trabeculae of basaloid cells within a dense, sclerotic stroma. Each epithelial nest features a peripheral rim of palisading basaloid cells surrounding central pale or clear cells, often forming pseudocystic or bag-like spaces.
The hallmark is abundant intraepithelial and stromal lymphocytic infiltration (predominantly T-cells) admixed with histiocytes, creating a lymphoepithelial pattern. Lymphocytes permeate epithelial lobules, while histiocytes fill central areas. Stroma is collagenous, with fibroblasts and occasional mucin. Peripheral follicular differentiation, such as papillary mesenchymal bodies or germ-like structures, supports trichoblastic origin.
- Microscopic subtypes:
- Classic type: Symmetric lobules with dense lymphoid infiltrate
- Adamantinoid variant: Larger epithelial islands with clear cells
- Branching type: Interconnected trabeculae mimicking syringoma
| Feature | Description |
|---|---|
| Tumor architecture | Well-defined dermal nodules, no encapsulation |
| Epithelial cells | Peripheral basaloid palisading; central eosinophilic/clear cells |
| Infiltrate | Intraepithelial lymphocytes (T-cells) + histiocytes |
| Stroma | Desmoplastic, collagenous, ± mucin |
| Other | ± Follicular papillae; rare ducts/osteoma |
No cytologic atypia, mitoses, or necrosis is seen, confirming benignity. Connections to epidermis or follicles occur in ~20% of cases.
Histogenesis and Variants
The origin of CL is controversial. Initial descriptions suggested eccrine or lymphoepithelial differentiation, akin to salivary gland tumors. Others proposed BCC-like features or desmoplastic trichoepithelioma. Contemporary consensus views CL as a trichoblastoma variant with adamantinoid (clear cell) features and unique lymphoid stroma. Cytokeratin 17 (CK17) strongly labels CL, aiding distinction from BCC.
Variants include:
- Classic lymphadenoma: Lymphoid-rich, bag-like nests.
- Adamantinoid trichoblastoma: Prominent clear cells, follicular differentiation.
- Branching/syringoid: Duct-like structures, sweat gland mimic.
In one study, peripheral follicular induction and CD34 patterns resembled immature follicular tumors rather than pure adamantinoid trichoblastoma. The dense T-lymphoid infiltrate is distinctive, absent in other adamantinoid adnexal tumors.
Immunohistochemistry
IHC confirms dual epithelial-lymphoid components. Epithelial cells express pancytokeratins (AE1/AE3), CK17 (highly sensitive for CL vs. BCC), CK5/6, and p63. Basaloid periphery shows CD34 in some cases, overlapping with BCC.
Lymphoid infiltrate is polyclonal T-cells (CD3+, CD4>CD8, UCHL-1+), with rare CD30+ activated cells and histiocytes (CD68+). Leukocyte common antigen (CLA) labels lymphocytes. No light chain restriction excludes lymphoma.
| Marker | Pattern in CL |
|---|---|
| AE1/AE3, CK17 | Strong epithelial labeling |
| CD3, CD4 | Lymphocytes (intraepithelial/stromal) |
| CD68 | Histiocytes in lobule centers |
| CD34 | Peripheral basaloid cells (subset) |
| Ki67 | Low (<5%), basal location |
CK17 immunohistochemistry is particularly useful, showing high sensitivity in discriminating CL from BCC.
Differential Diagnosis
CL mimics several entities:
- Basal cell carcinoma: Lacks intraepithelial lymphocytes; retraction artifact, higher atypia; CK17 weaker.
- Trichoepithelioma: More organized follicular structures, fewer lymphocytes, ADAM2+ stroma.
- Lymphoepithelial carcinoma: Atypical keratinocytes, p53+, ductal differentiation.
- Cutaneous lymphoma: Monoclonal infiltrate, epidermotropism absent.
- Syringoma: True ducts, less lymphoid infiltrate.
Video pathology highlights basiloid islands packed with histiocytes and lymphocytes, with keratin staining rimming epithelial components.
Treatment and Prognosis
Complete surgical excision with clear margins is the treatment of choice, curative in nearly all cases. Mohs micrographic surgery may be considered for facial lesions to preserve tissue. Shave excision risks recurrence, as documented in forehead cases. No adjuvant therapy is needed due to benign behavior. Long-term follow-up is unnecessary absent recurrence.
Frequently Asked Questions (FAQs)
Q: Is cutaneous lymphadenoma malignant?
A: No, it is a benign adnexal tumor with no metastatic potential. Complete excision prevents recurrence.
Q: What is the most common location for cutaneous lymphadenoma?
A: Head and neck region, especially the face (forehead, cheeks, nose).
Q: How does CL differ histologically from basal cell carcinoma?
A: CL features dense intraepithelial T-lymphocytes and histiocytes, peripheral follicular differentiation, and lacks BCC’s retraction clefts or high atypia. CK17 is more diffuse in CL.
Q: Can cutaneous lymphadenoma recur?
A: Rare, but possible after incomplete shave excision. Ensure margin-free removal.
Q: What is the histogenesis of CL?
A: Likely a trichoblastoma variant (adamantinoid type) with unique lymphoid infiltrate.
Conclusion
Cutaneous lymphadenoma exemplifies a rare yet architecturally striking benign tumor, blending epithelial and lymphoid elements. Awareness of its features prevents misdiagnosis as malignancy. Pathologists should seek follicular clues and perform IHC for confirmation.
References
- Benign lymphoepithelial tumor of the skin (“cutaneous lymphadenoma”) — eScholarship. 2006. https://escholarship.org/uc/item/3xf75552
- Cutaneous Lymphoma — Yale Medicine. 2023. https://www.yalemedicine.org/clinical-keywords/cutaneous-lymphoma
- Cutaneous Lymphadenoma: A Case of Recurrence after Shave Excision — Wiley Online Library. 2021-09-15. https://onlinelibrary.wiley.com/doi/10.1155/2021/5543404
- Cutaneous lymphadenoma — PubMed. 2003-11-01. https://pubmed.ncbi.nlm.nih.gov/14639395/
- Cutaneous Lymphadenoma: Report of 2 Cases — Karger Publishers. 1989. https://karger.com/drm/article/185/1/62/110054/Cutaneous-Lymphadenoma-Report-of-2-Cases
- Cutaneous Lymphadenoma (aka adamantinoid trichoblastoma) — YouTube (Pathology video). 2020. https://www.youtube.com/watch?v=tMP6rbNjqD0
- Cutaneous Lymphadenoma: A Case Report and Systematic Review — PubMed Central. 2012. https://pmc.ncbi.nlm.nih.gov/articles/PMC3331883/
Read full bio of Sneha Tete