Dermoscopy of Lichen Sclerosus
Explore dermoscopic patterns in lichen sclerosus for accurate diagnosis of anogenital and extragenital lesions.

Lichen sclerosus (LS) is a chronic inflammatory dermatosis primarily affecting the anogenital region but also occurring extragenitally, characterized by ivory-white sclerotic plaques with potential for atrophy and scarring.
Introduction
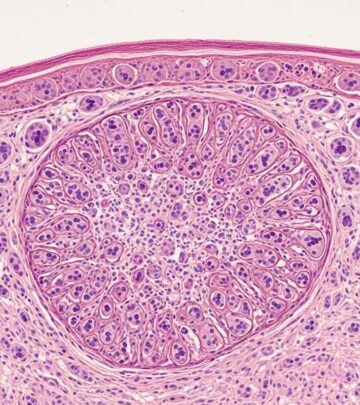
Lichen sclerosus represents a lymphocytic autoimmune-mediated dermatosis that leads to progressive skin fibrosis and epidermal atrophy. While predominantly anogenital, extragenital manifestations occur in up to 10-20% of cases, often on the trunk, limbs, or flexures. Early diagnosis is crucial to prevent irreversible scarring, dyspareunia, or squamous cell carcinoma risk in genital sites. Traditional diagnosis relies on clinical examination and biopsy, but dermoscopy offers a non-invasive bridge, revealing subtle vascular, textural, and pigmentary changes that correlate with histopathology.
Dermoscopy enhances visualization of epidermal, dermo-epidermal, and papillary dermal structures using polarized or non-polarized modes. In LS, it identifies patterns like whitish structureless areas (WSA), comedo-like openings (CLO), and specific vessels, aiding differentiation from mimics such as vitiligo or morphea.
Clinical Features
LS classically presents as porcelain-white, crinkled or thickened patches with a wrinkled ‘cigarette paper’ appearance. Genital LS shows well-defined ivory plaques on the vulva, penis, or perianal skin, often with erosions, fissures, or purpura from trauma. Extragenital LS manifests as hypopigmented macules or plaques on the upper trunk, arms, or thighs, less symptomatic but prone to koebnerization.
- Early lesions: Hypopigmented macules with subtle induration or follicular changes.
- Late lesions (>2 years): Atrophic, sclerotic plaques with telangiectasia and scarring.
- Genital specifics: Loss of labia minora, introital narrowing, phimosis in males.
- Extragenital: Guttate hypomelanosis-like spots or hyperkeratotic variants.
In a study of 20 Indian patients with extragenital LS, morphologies included scleroatrophic (61.5%), guttate (30.8%), and hyperkeratotic (7.7%) lesions, highlighting morphological diversity.
Dermoscopic Features
Dermoscopy of LS reveals distinctive patterns varying by stage, location, and mode (polarized vs. non-polarized). Non-polarized mode excels in detecting keratotic plugs and scales, while polarized highlights white structures and vessels.
Early Lesions
Predominant findings include:
- Whitish structureless areas (WSA): Homogeneous white-yellow patches (100% prevalence), reflecting epidermal atrophy and hyperkeratosis.
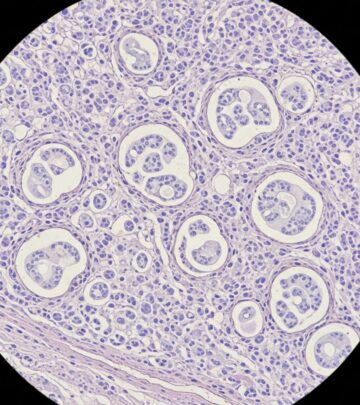
- Comedo-like openings (CLO): Dilated follicular ostia with keratin plugs (50-80%), more prominent early due to follicular plugging.
- Dotted or comma-shaped vessels: In net-like or linear patterns, indicating dilated papillary vessels (61.5%).
- Perifollicular scaling: Fine scales around follicles (50%).
Late Lesions (More Than 2 Years)
Features evolve with fibrosis:
- Chrysalis-like structures: White linear streaks or bands (80.8%), due to subepidermal collagen homogenization.
- White clods or linear tracks: Shiny white streaks (white cornflake-like areas, WCLA) visible in polarized mode, signifying dermal sclerosis.
- Telangiectasia: Linear irregular vessels of varying caliber.
- Rosettes: Novel finding in 38.5% (rosette = four white lines converging to a central white circle), possibly scale-related.
- Reduced CLO/WSA: Less follicular involvement in advanced atrophy.
In three cases of extragenital LS, WSA, CLO, and net-like dotted vessels were consistent, correlating with histopathology. Four women showed central CLO within whitish plaques.
Genital vs. Extragenital
| Feature | Genital LS | Extragenital LS |
|---|---|---|
| WSA | Porcelain-white glow | Cloudy white-yellow areas |
| Vessels | Prominent telangiectasia | Dotted/comma in nets |
| CLO | Less common | Predominant early |
| Chrysalis | Frequent in sclerosis | 80.8% in studies |
Polarized dermoscopy is key for genital sites, revealing fibrosis absent in non-polarized views.
Differential Diagnoses
LS mimics require dermoscopy for distinction:
- Vitiligo: Uniform ‘white glow’ structureless areas without vessels or CLO; loss of pigment network.
- Idiopathic guttate hypomelanosis (IGH): ‘Cloudy sky’ white areas in amoeboid/petaloid patterns, no WSA or plugs.
- Morphea: Fibrotic white bands without CLO; ‘sweat duct openings’ in active edges.
- Lichen planus: Comma/hairpin vessels, Wickham striae; lacks WSA dominance.
- Lichen simplex chronicus: Irregular vessels, diffuse scaling; no structureless white.
Dermoscopy avoids biopsy in 70-80% of cases by highlighting LS-specific CLO and chrysalis structures.
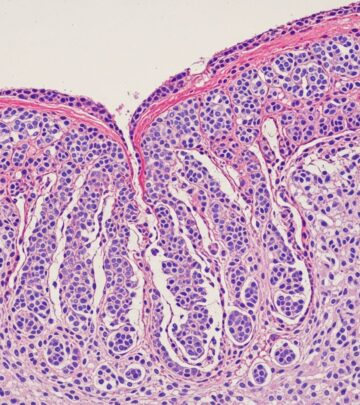
Histological Explanation
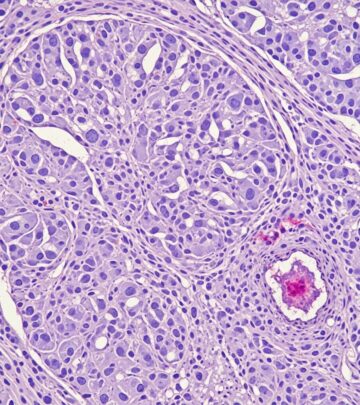
Dermoscopic-histological correlations are robust:
- WSA: Hyperkeratosis, compact orthokeratosis, epidermal atrophy.
- CLO: Follicular plugging, dilated ostia with keratin.
- Chrysalis/WCLA: Homogenized, hyalinized collagen in dermis; edema.
- Vessels: Dilated capillaries in atrophic papillary dermis with lymphocytic infiltrate.
- Rosettes: Possibly crystallized scales or keratin whorls (novel).
Histopathology confirms: epidermal atrophy, basal vacuolization, dermal edema, homogenized collagen, perivascular/perifollicular lymphohistiocytic infiltrate. Early nonspecific changes underscore dermoscopy’s role.
Frequently Asked Questions (FAQs)
Can dermoscopy replace biopsy in lichen sclerosus?
Dermoscopy aids early diagnosis and differentials, potentially avoiding biopsy in classic cases, but histopathology confirms atypical or early lesions.
What is the most common dermoscopic finding in LS?
Structureless white-yellow areas (100%), followed by chrysalis-like structures (80.8%).
Is extragenital LS dermoscopically different from genital?
Extragenital shows more CLO and dotted vessels; genital emphasizes telangiectasia and porcelain glow.
What does comedo-like openings represent histologically?
Follicular keratin plugging in dilated ostia, prominent in early lesions.
Are rosettes specific to LS?
A new finding in 38.5% of extragenital LS, not previously reported; utility needs validation.
Conclusion
Dermoscopy revolutionizes LS management with non-invasive, stage-specific patterns correlating to histopathology. Combining modes enhances accuracy, reducing biopsy needs and enabling prompt treatment with topical corticosteroids.
References
- Dermoscopic patterns in lichen sclerosus: A report of three cases — Indian Dermatol Online J. 2015-05-15. https://pmc.ncbi.nlm.nih.gov/articles/PMC4439768/
- Dermoscopic evaluation of extragenital lichen sclerosus et atrophicus — Dermatol Pract Concept. 2022-10-01. https://dpcj.org/index.php/dpc/article/view/1854
- Dermoscopic Evaluation of Extragenital Lichen Sclerosus et … — PubMed. 2022-09-01. https://pubmed.ncbi.nlm.nih.gov/36159134/
- Dermoscopy of lichen sclerosus — DermNet NZ. 2023-01-01. https://dermnetnz.org/topics/dermoscopy-of-lichen-sclerosus
- Dermoscopy of Extragenital Lichen Sclerosus — JAMA Dermatol. 2008-11-01. https://jamanetwork.com/journals/jamadermatology/fullarticle/712308
- Lichen sclerosus: Causes, Diagnosis, and Images — DermNet NZ. 2023-01-01. https://dermnetnz.org/topics/lichen-sclerosus
Read full bio of medha deb