Digital Myxoid Pseudocyst Pathology
Comprehensive pathology of digital myxoid pseudocysts: histology, variants, and diagnostic features for clinicians and pathologists.
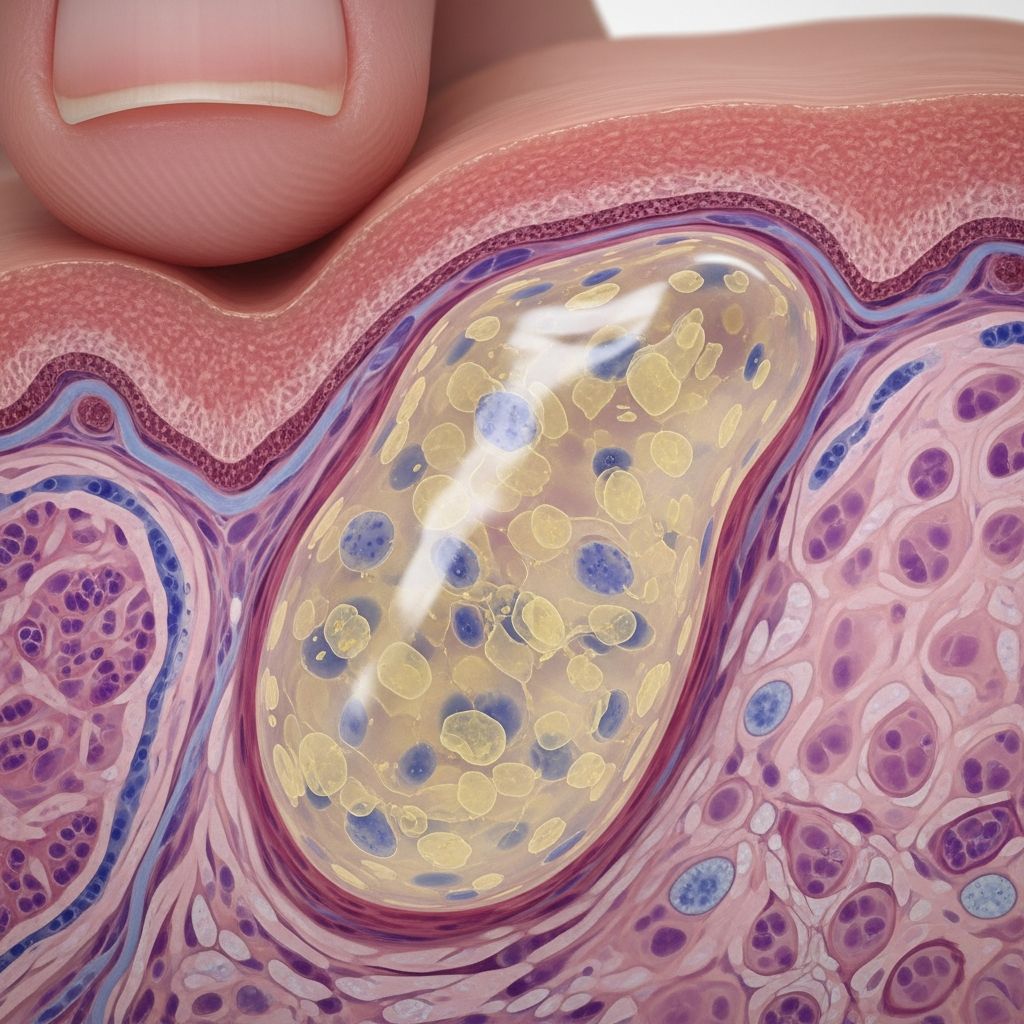
Digital myxoid pseudocyst, commonly referred to as a digital mucous cyst, represents a focal accumulation of mucin beneath the skin, predominantly affecting the distal aspects of the fingers. This benign lesion typically presents as a solitary, skin-coloured to translucent nodule, often exerting pressure on the overlying nail apparatus, leading to characteristic grooves or structural deformities. Frequently associated with underlying osteoarthritis, particularly of the distal interphalangeal joint (DIPJ), it is considered a ganglion-like structure in such contexts, with potential for multiplicity in patients with chronic arthritic conditions. Treatment modalities focus on content evacuation, destructive techniques, or surgical excision to prevent recurrence and nail damage.
Clinical features
Digital myxoid pseudocysts manifest as shiny, dome-shaped papules located within 1 cm of the proximal nail fold on fingers or toes, exhibiting a semi-translucent appearance due to their jelly-like mucinous content. These pseudocysts lack a true epithelial lining, distinguishing them from genuine cysts, and arise from either focal mucin deposition in the dermis or synovial fluid leakage from the DIPJ via a communicating tract. The most common site is the dorsal aspect of the DIPJ, with predominance on the dominant hand’s index or ring fingers.
Clinically, the lesion measures 5 mm to 1 cm, featuring a smooth, shiny surface that may transilluminate, revealing viscous, straw-coloured or blood-tinged fluid upon expression. Nail involvement is hallmark, with longitudinal grooves (up to several mm wide) resulting from matrix compression; these may fluctuate in depth, producing a ‘waves sign’ under dermoscopy for cysts overlying the germinal matrix. Subtypes include type A (between DIPJ crease and proximal nail fold), type B (within proximal nail fold compressing matrix), and type C (beneath nail plate), influencing visible features and dystrophy severity. Pain is uncommon unless infection or significant joint degeneration occurs, but associated DIPJ osteoarthritis may cause stiffness.
Pathogenesis
The aetiology bifurcates into two primary mechanisms. The myxomatous variant stems from localised cutaneous mucinosis, where fibroblasts excessively produce hyaluronic acid and other mucopolysaccharides, independent of joint communication. This results in dermal mucin pools without synovial origin. Conversely, the ganglion variant links to DIPJ osteoarthritis, involving synovial lining herniation or fluid extravasation through capsular defects, forming a pseudocyst with potential stalk connection to the joint.
Traumatic degeneration of connective tissue overlying the DIPJ also contributes, with prevalence up to 12% among nail unit tumours. In osteoarthritic patients, Heberden nodes may coexist, amplifying risk. Histogenetically, both types feature fibroblast metaplasia and mucin accumulation, but ganglion forms show compressed collagen and occasional haemorrhage. Fluctuating cyst volume, due to joint fluid dynamics, explains variable nail grooving.
Clinical variants
- Myxomatous type: Pure focal mucinosis with abundant dermal mucopolysaccharides, no joint communication; often smaller and nail-independent.
- Ganglion type: Associated with osteoarthritis; communicates with DIPJ synovium, larger, more prone to recurrence post-evacuation.
- Multiple lesions: Seen in chronic arthritis, reflecting polyarticular degeneration.
Dermoscopy
Dermoscopy aids non-invasive diagnosis, revealing structureless bluish areas from mucin, alongside vascular patterns: arborizing, dotted, linear, or polymorphous vessels, and red-purple lacunae. The ‘waves sign’—irregular, shore-like grooving in fluctuating matrix-overlying cysts—distinguishes from static dystrophies. Ulcerated or subtle lesions benefit most, highlighting even non-evident pseudocysts.
Diagnosis
Diagnosis is primarily clinical, supported by transillumination (silhouetting mucin), needle aspiration (yielding gelatinous fluid), or methylene blue injection to trace joint tracts. Ultrasonography confirms communication or subungual location. Histopathology is confirmatory for ambiguous cases, showing avascular mucin lakes rimmed by fibroblasts without epithelial lining.
Pathology
Histology: Low-power view displays a well-circumscribed submucosal or subcutaneous nodule filled with abundant pale basophilic mucin dissecting collagen bundles, compressing surrounding tissue into a pseudocapsule. No true epithelial lining exists; instead, a fibrous connective tissue wall with fibroblasts and histiocytes encases the pool. Mucin appears slightly bluish on H&E, with stellate fibroblasts and occasional entrapped collagen strands.
In ganglion variants, subtle haemorrhage or haemosiderin may appear, alongside osteoarthritis-related bone changes if excised with joint tissue. Myxomatous forms emphasise pure mucinosis with fibroblast hyperactivity.
| Feature | Myxomatous Variant | Ganglion Variant |
|---|---|---|
| Mucin Source | Dermal fibroblasts (hyaluronic acid) | DIPJ synovial fluid leak |
| Joint Link | Absent | Present (stalk/tract) |
| Associated OA | Rare | Common |
| Recurrence Risk | Low | High without excision |
Histochemistry
Mucin stains positively with colloidal iron (blue), Alcian blue (pH 2.5, turquoise), and toluidine blue (metachromatic pink-purple), confirming glycosaminoglycan composition. These highlight mucin pools sharply against stroma, aiding quantification.
Differential diagnosis
- Ganglion cyst: Larger, deeper, joint-associated; true synovial lining possible.
- Rheumatoid nodule: Firmer, palisaded histiocytes, necrosis; rheumatoid arthritis context.
- Heberden node: Bony, painful; radiographic OA without mucin.
- Epidermoid cyst: Keratin-filled, epithelial lining; punctum often present.
- Verruca vulgaris: Hyperkeratotic, thrombosed vessels dermoscopically.
- Onychomatricoma/other nail tumours: Lack fluctuation, different dermoscopy.
Treatment pathology considerations
Post-treatment specimens may show fibrosis or inflammation if sclerotherapy or laser used; surgical pieces confirm mucin evacuation and tract ligation to minimise recurrence. Recurrence rates drop with DIPJ exploration.
Frequently asked questions
What is a digital myxoid pseudocyst?
A benign mucin-filled pseudocyst on distal fingers/toes, often causing nail grooves.
Is it cancerous?
No, entirely benign; not contagious or malignant.
Does it always connect to the joint?
No; myxomatous type does not, ganglion type does.
How is pathology confirmed?
H&E shows mucin pools; special stains (Alcian blue etc.) highlight glycosaminoglycans.
What if it recurs?
Surgical excision with joint tract interruption recommended.
References
- Digital myxoid pseudocyst pathology — DermNet NZ. 2023. https://dermnetnz.org/topics/digital-myxoid-pseudocyst-pathology
- Digital mucous (myxoid) cyst — DermNet NZ. 2023. https://dermnetnz.org/topics/digital-myxoid-pseudocyst
- The “Waves Sign” in Digital Myxoid Pseudocyst — PMC/NCBI (PMID: 38835718). 2024-05-31. https://pmc.ncbi.nlm.nih.gov/articles/PMC11147518/
- Verruca Vulgaris and Digital Mucoid Cyst — Dermatology Advisor. 2024. https://www.dermatologyadvisor.com/ddi/verruca-vulgaris-digital-mucoid-cyst/
- Digital Mucous Cyst — StatPearls/NCBI Bookshelf (NBK559092). 2023-08-08. https://www.ncbi.nlm.nih.gov/books/NBK559092/
Read full bio of medha deb