Drug-Induced Pemphigus
Understanding drug-induced pemphigus: causes, symptoms, diagnosis, and effective treatment strategies for this rare autoimmune blistering disorder.
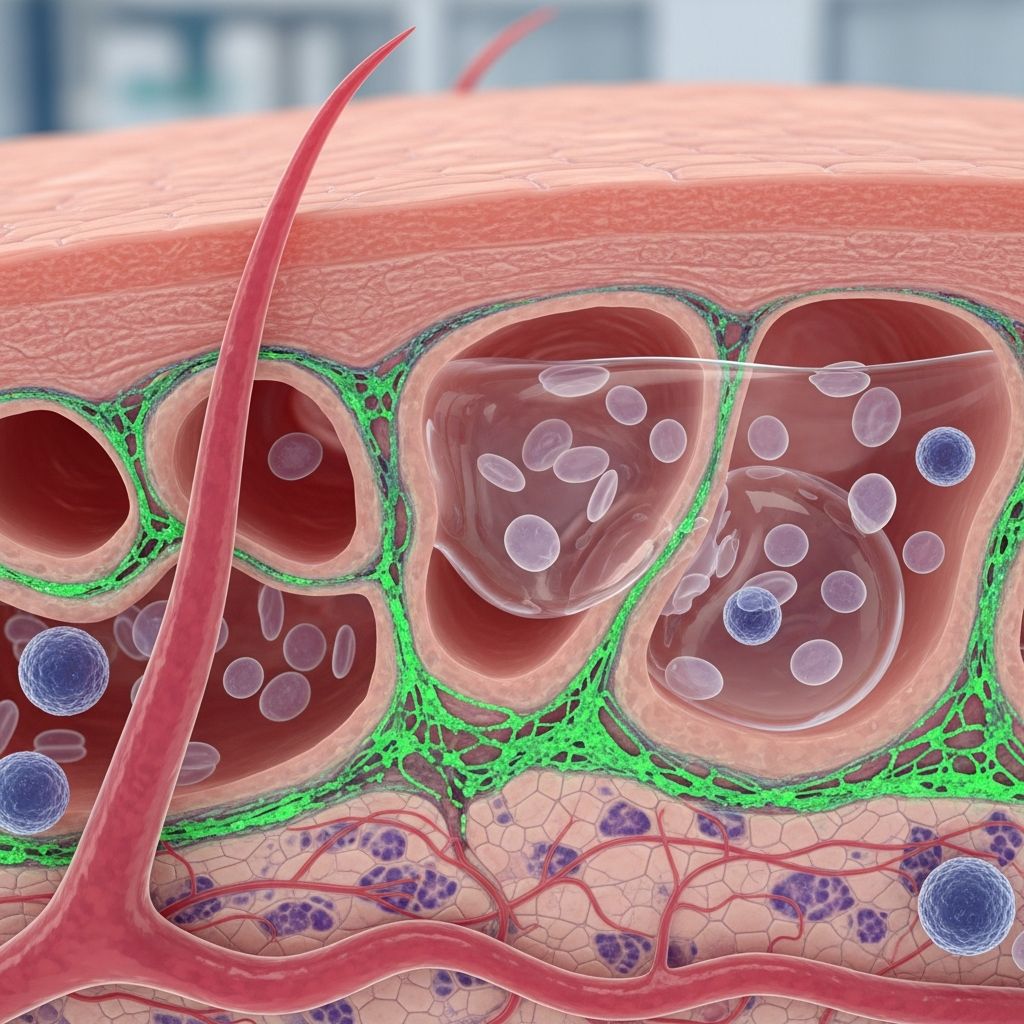
Drug-induced pemphigus represents a rare but significant subtype of pemphigus, an autoimmune blistering disorder where medications trigger an immune response against desmoglein proteins in the skin, leading to acantholysis and intraepidermal blisters identical to idiopathic forms.
What is drug-induced pemphigus?
Drug-induced pemphigus (DIP) occurs when certain medications precipitate pemphigus, typically by inducing autoantibodies against desmogleins, the proteins responsible for keratinocyte adhesion in the epidermis. This results in the separation of skin cells (acantholysis), forming flaccid blisters and erosions. Unlike idiopathic pemphigus, DIP is directly linked to drug exposure, with onset ranging from days to 6 months or more after starting the offending agent. Over 200 cases have been documented, often in patients resembling those with spontaneous pemphigus in demographics and clinical presentation.
Pemphigus encompasses several variants, including pemphigus vulgaris (PV), pemphigus foliaceus (PF), pemphigus erythematosus, IgA pemphigus, and paraneoplastic pemphigus. DIP most commonly mimics PV or PF, depending on the drug class. It affects approximately 1 in 100,000 people annually, with higher prevalence among Jewish and Mediterranean populations, equally in men and women aged 40-60.
Who gets drug-induced pemphigus?
Individuals developing DIP share characteristics with idiopathic pemphigus patients: middle-aged adults (40-60 years), no strong gender bias, and genetic predispositions in Ashkenazi Jewish or Mediterranean ancestries. Risk escalates with prolonged exposure to culprit drugs; for instance, D-penicillamine use over 6 months yields a 7% incidence in some studies. Patients with pre-existing pemphigus in remission may experience reactivation upon re-exposure. Those on multiple medications face diagnostic challenges due to delayed onset.
- Demographics: 40-60 years old, equal male/female ratio.
- Ethnic predisposition: Jewish, Mediterranean descent.
- Risk factors: Long-term thiol drug therapy, polypharmacy.
What causes drug-induced pemphigus?
DIP arises from drugs disrupting intercellular adhesion via immune or biochemical mechanisms. Thiol drugs (-SH group containing) dominate, comprising 75% of cases, by inhibiting enzymes like protein kinase C, promoting acantholysis. Phenol drugs induce inflammatory cytokines (TNF-alpha, IL-1), weakening desmoglein bonds. Non-thiol/non-phenol drugs act via B-cell stimulation, producing anti-desmoglein IgG antibodies.
Thiol drugs induce superficial PF-like disease; non-thiols cause deeper PV-like involvement. Topical agents can trigger localized ‘contact pemphigus’. In some cases without detectable desmoglein antibodies, direct biochemical acantholysis is implicated.
Drugs that cause pemphigus
| Drug Class | Examples | Associated Pemphigus Type |
|---|---|---|
| Thiols | D-penicillamine, captopril, tiopronine, penicillin | Foliaceus (superficial) |
| Phenols | Aspirin, heroin, rifampin, levodopa | Vulgaris (deep) |
| Non-thiol/phenol | Piroxicam, propranolol, pyritinol, ACE inhibitors, antibiotics (piperacillin-tazobactam, linezolid) | Vulgaris or foliaceus |
| Topical | Imiquimod, ketoprofen, neomycin, bacitracin, benzoin, chromium sulfate | Contact pemphigus (localized) |
Penicillamine and captopril are notorious, with penicillamine linked to 7% incidence after 6 months.
Clinical features of drug-induced pemphigus
Features mirror idiopathic pemphigus but correlate with drug type. Thiol-induced: scaly, crusted erosions on seborrheic areas (scalp, face, upper trunk) like PF. Non-thiol: flaccid blisters/erosions on mucosa (mouth 50-70%), skin flexures like PV. Pruritus or burning precedes lesions; Nikolsky sign (epidermis shears with friction) is positive. Vaginal/oral involvement prompts full mucocutaneous exam.
- Thiol drugs: Erythematous plaques, flaccid pustules, erosions healing with hyperpigmentation; rare mucosal disease.
- Non-thiol drugs: Intense mucosal erosions, fragile blisters rupturing to denuded skin; scalp, face, trunk affected.
- Progression: Starts localized, spreads if drug continued.
Diagnosis of drug-induced pemphigus
Diagnosis hinges on history of recent/prolonged drug exposure plus typical clinical/histological findings. Challenges arise in polypharmacy or delayed onset (up to 6 months). Key steps:
- Clinical history: Timeline of drug start and symptom onset; exclude idiopathic via antibody testing.
- Skin biopsy: Suprabasal acantholysis (PV) or subcorneal (PF); tombstoning of basal cells.
- Immunofluorescence: Direct (DIF): intercellular IgG/C3 on keratinocytes; Indirect (IIF): circulating anti-Dsg1 (PF) or anti-Dsg3 (PV) antibodies.
- ELISA: Quantifies anti-desmoglein antibodies; absent in some thiol cases suggests biochemical mechanism.
Differential includes bullous impetigo, Hailey-Hailey disease; DIF distinguishes.
Management of drug-induced pemphigus
Primary: immediate culprit drug withdrawal, often leading to remission in thiol cases without antibodies. Supportive: wound care, infection prevention. Systemic immunosuppression for persistent/severe disease, as untreated pemphigus is life-threatening (mortality 75% pre-corticosteroids).
Treatment
- First-line: High-dose corticosteroids (prednisone 1-2 mg/kg/day) to halt blistering.
- Steroid-sparing: Azathioprine, mycophenolate mofetil, methotrexate, cyclophosphamide.
- Biologics: Rituximab (anti-CD20) targets B-cells; effective but rare exacerbations reported.
- Adjuncts: IVIG, dapsone, antibiotics for secondary infection.
Treatment staged: induction (high-dose steroids), consolidation (taper + immunosuppressant), maintenance (low-dose). Monitor via blood tests for side effects (osteoporosis, diabetes, infections).
Outlook and complications
Prognosis varies: thiol-DIP without antibodies resolves in ~50% post-withdrawal; antibody-positive cases mimic chronic idiopathic pemphigus, requiring long-term therapy. Non-thiol worse prognosis. Early intervention improves outcomes; many remit but may need years of meds.
Complications:
- Secondary bacterial infections, sepsis.
- Skin ulcers, gangrene.
- Severe pain, poor cosmesis (scarring, dyspigmentation).
- Therapy-related: steroid side effects (moon face, osteoporosis).
Frequently Asked Questions
What drugs most commonly cause pemphigus?
Thiol drugs like D-penicillamine, captopril; phenols like aspirin; others include piroxicam, ACE inhibitors.
How is drug-induced pemphigus diagnosed?
Via clinical history, biopsy showing acantholysis, DIF/IIF for intercellular IgG, anti-desmoglein ELISA.
Does stopping the drug always cure it?
No; thiol cases without antibodies often remit (50%), but antibody-positive persist like idiopathic forms.
What is the treatment for severe cases?
High-dose prednisone + immunosuppressants (azathioprine); rituximab for refractory disease.
Is drug-induced pemphigus preventable?
Monitor high-risk drugs (e.g., penicillamine); early recognition via history aids prompt withdrawal.
References
- Drug Induced Pemphigus — MD Searchlight. 2023. https://mdsearchlight.com/medications/drug-induced-pemphigus/
- Drug-induced pemphigus — DermNet NZ. 2024-01-15. https://dermnetnz.org/topics/drug-induced-pemphigus
- Pemphigus – Diagnosis and treatment — Mayo Clinic. 2025-06-12. https://www.mayoclinic.org/diseases-conditions/pemphigus/diagnosis-treatment/drc-20350409
- Pemphigus: Types, Symptoms, Causes & Treatment — Cleveland Clinic. 2024-11-05. https://my.clevelandclinic.org/health/diseases/21130-pemphigus
- Drug Induced Pemphigus — NCBI StatPearls. 2023-07-17. https://www.ncbi.nlm.nih.gov/books/NBK499864/
Read full bio of Sneha Tete












