Eosinophilic Fasciitis Pathology
Detailed pathology insights into eosinophilic fasciitis, a rare fibrosing disorder with inflammation of deep fascia and eosinophil infiltration.
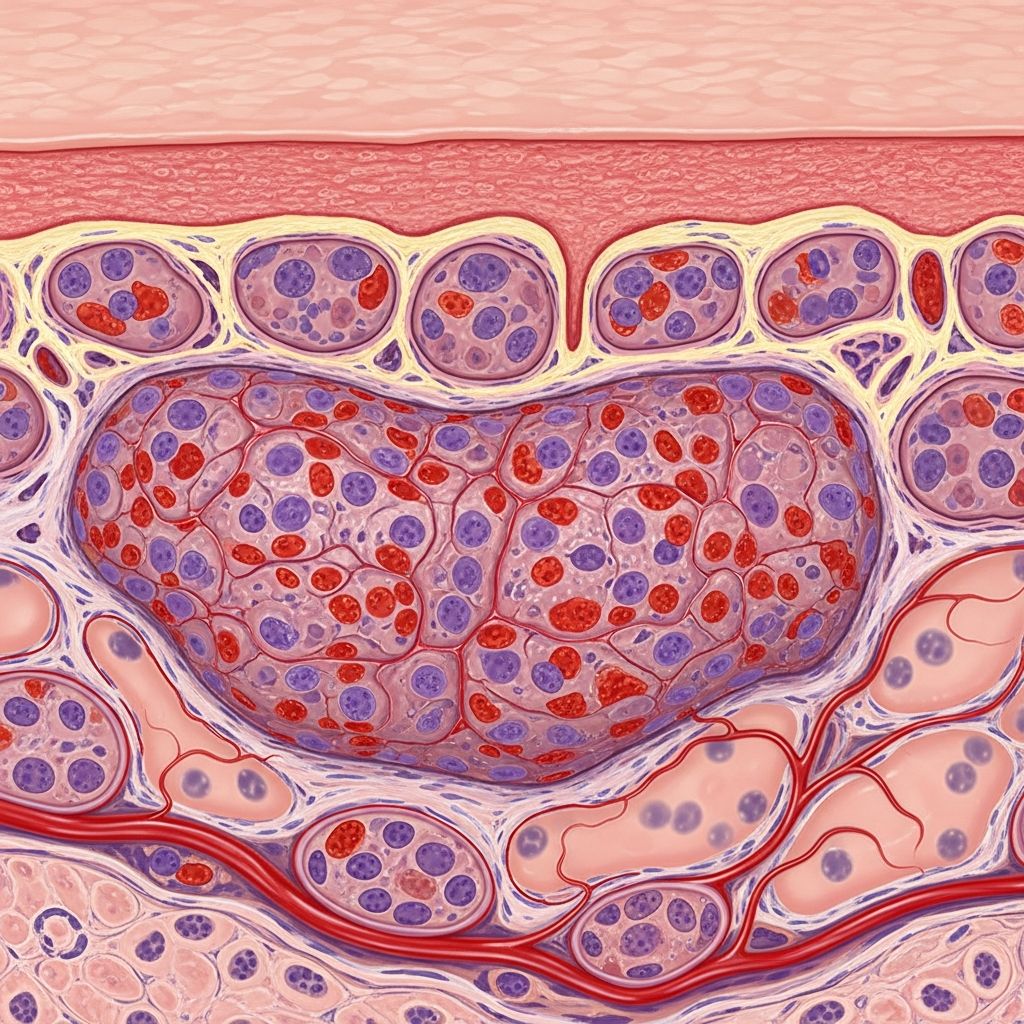
Eosinophilic fasciitis (EF), also known as Shulman’s syndrome, is a rare scleroderma-like disorder characterized by inflammation and thickening of the deep fascia, the tough connective tissue layer beneath the skin that envelops muscles. Pathologically, it features prominent eosinophilic infiltration in the fascia and adjacent tissues, leading to progressive fibrosis. This condition spares the overlying dermis and epidermis, distinguishing it from superficial sclerotic disorders.
Introduction
Eosinophilic fasciitis represents a unique fibrosing disorder with acute onset of edema followed by induration primarily affecting the extremities. First described by Shulman in 1974, its pathology centers on the deep fascia, where inflammatory cells, particularly eosinophils, accumulate abnormally. This leads to fascia thickening up to 10-20 times normal, with fibrosis extending into superficial muscle and septa of subcutaneous fat. Peripheral blood eosinophilia is common, affecting 60-90% of cases, though not universal. The disorder’s rarity—fewer than 300 reported cases—necessitates deep incisional biopsies for definitive diagnosis.
Demographics
EF typically manifests in middle-aged adults, with a mean onset age of 40-50 years. It shows a slight male predominance (1.5-2:1 male-to-female ratio). No strong racial or geographic predilections are noted, though cases cluster post-strenuous exercise or trauma. Pediatric cases are exceedingly rare, comprising less than 5% of reports. Association with HLA-DR4 suggests a genetic susceptibility component in some populations.
Causes
The precise etiology remains idiopathic in most cases, but immune dysregulation drives pathogenesis. Triggers include:
- Vigorous exercise or physical trauma preceding onset in 50-60% of patients.
- Autoimmune associations: 20-30% concurrent with malignancies (e.g., lymphoma, solid tumors); links to autoimmune thyroiditis, rheumatoid arthritis.
- Drug-induced: Rare reports with statins, carbidopa, or L-tryptophan (historical eosinophilia-myalgia syndrome).
- Infectious or paraproteinemic triggers hypothesized but unproven.
Pathogenic mechanisms involve T-cell activation, with elevated interferon-gamma and IL-5 production stimulating eosinophil recruitment. Eosinophil degranulation releases major basic protein and eosinophil cationic protein, inducing fibroblast activation and collagen overproduction.
Clinical Features
Symptoms evolve acutely: initial painful edema and erythema of forearms, legs, and thighs, sparing hands, feet, and face. Progression yields ‘woody’ induration with peau d’orange texture and venous grooving along superficial veins. Joint contractures develop in 50% untreated cases due to periarticular fibrosis. Systemic features include fatigue, myalgias, and occasional sicca symptoms.
Complications
Untreated EF leads to:
- Permanent joint contractures limiting mobility (elbows, knees most affected).
- Reflex sympathetic dystrophy or carpal tunnel syndrome from nerve compression.
- Secondary morphea plaques in 20-40%.
- Rare progression to systemic sclerosis or aplastic anemia.
Long-term fibrosis causes muscle atrophy and reduced quality of life.
Diagnosis
Diagnosis hinges on full-thickness incisional biopsy from indurated skin to muscle, ideally from forearm. Key pathological hallmarks:
| Feature | Description |
|---|---|
| Fascia Thickening | 2-20x normal, hyalinized collagen bundles. |
| Inflammatory Infiltrate | Diffuse eosinophils (10-100/field), lymphocytes, plasma cells; perivascular emphasis. |
| Adjacent Tissues | Septal panniculitis, superficial muscle/perimysial inflammation; dermis spared. |
| Late Stage | Fibrosis predominates, eosinophils wane. |
Laboratory: Eosinophilia (absolute count >0.5 x 10^9/L), elevated ESR/CRP, hypergammaglobulinemia. MRI reveals fascia hyperintensity on T2; ultrasound detects thickening.
Differential Diagnoses
| Condition | Key Distinctions from EF |
|---|---|
| Scleroderma (Systemic) | Raynaud’s, nailfold capillary changes, acral involvement, anti-nuclear antibodies; dermis thickened. |
| Morphea | Bound-down plaques, epidermal atrophy; superficial dermis fibrosis. |
| Hypereosinophilic Syndrome | Multiorgan eosinophilic infiltration; cardiac/hematologic involvement. |
| Poly- and Dermatomyositis | Proximal muscle weakness, elevated CK, interface dermatitis. |
EF uniquely spares digits and shows fascia-centric pathology.
Treatment
First-line: High-dose prednisone (1 mg/kg/day) tapered over months; 70-90% respond within weeks. Refractory cases require methotrexate, mycophenolate, or rituximab. Adjuncts include hydroxychloroquine for morphea overlap or PUVA phototherapy. Monitor response via serial MRI or biopsy.
Outcome
Prognosis is favorable with early treatment: 80% achieve remission, though 20-30% relapse requiring maintenance therapy. Residual fibrosis or contractures persist in delayed diagnoses. Malignancy surveillance advised at onset.
Frequently Asked Questions (FAQs)
What is the hallmark pathology of eosinophilic fasciitis?
Thickened deep fascia with dense eosinophilic infiltrate, sparing the dermis.
How is EF diagnosed definitively?
Full-thickness skin-to-muscle biopsy confirming fascial inflammation and fibrosis.
Does EF progress to systemic sclerosis?
Rarely; most cases remain localized without visceral involvement.
What labs support EF diagnosis?
Peripheral eosinophilia, elevated inflammatory markers; ANCA/ANA often negative.
Is exercise a trigger for EF?
Yes, reported in up to 60% preceding onset, suggesting trauma-induced immune activation.
References
- Eosinophilic Fasciitis — American Partnership for Eosinophilic Disorders (APFED). 2023. https://apfed.org/about-ead/eosinophilic-fasciitis/
- Eosinophilic Fasciitis — National Organization for Rare Disorders (NORD). 2024-01-15. https://rarediseases.org/rare-diseases/eosinophilic-fasciitis/
- Eosinophilic Fasciitis — DermNet NZ. 2025. https://dermnetnz.org/topics/eosinophilic-fasciitis
- Eosinophilic Fasciitis (Shulman Syndrome) — Cleveland Clinic. 2024-06-20. https://my.clevelandclinic.org/health/diseases/23516-eosinophilic-fasciitis
- Eosinophilic fasciitis: Current concepts — PubMed (Semin Arthritis Rheum). 2018-10. https://pubmed.ncbi.nlm.nih.gov/30047432/
Read full bio of medha deb












