Extramammary Paget Disease Pathology
Detailed histopathological analysis of extramammary Paget disease, covering clinical variants, microscopic features, and diagnostic challenges.
Author: Dr Ian McColl, Dermatopathologist, PathX Pathology Laboratory, Auckland, New Zealand.
DermNet NZ Editor: Dr Martin Steffens, Dermatologist, Hamilton, New Zealand. January 2025.
Extramammary Paget disease (EMPD) represents a rare intraepithelial adenocarcinoma primarily affecting apocrine gland-bearing skin regions such as the anogenital and axillary areas. This condition is histopathologically characterized by the presence of large, pale Paget cells scattered within the epidermis, mimicking mammary Paget disease but occurring outside the breast.
Introduction
Histologically, EMPD manifests as an in situ adenocarcinoma where atypical Paget cells proliferate within the epidermis and adnexal structures. These cells derive from intraepithelial cells of apocrine or other gland ducts or pluripotent stem cells within the epidermis. EMPD is categorized into primary (originating from skin adnexa) and secondary (extension from underlying visceral carcinoma) forms, each with distinct pathological implications.
Primary EMPD arises independently in the epidermis, while secondary EMPD results from direct extension or metastasis from internal malignancies, particularly urogenital or gastrointestinal adenocarcinomas. Accurate differentiation is crucial for prognosis and management, as secondary forms carry a higher risk of associated systemic disease.
Clinical
EMPD typically presents as a slowly enlarging, erythematous, eczematous plaque with irregular borders, scaling, and crusting, predominantly in the vulvar, perianal, or axillary regions. Lesions may be asymptomatic or pruritic, often misdiagnosed as dermatitis, leading to diagnostic delays of months to years. Pigmented variants appear hyperpigmented, while ectopic EMPD occurs in non-apocrine sites like the face or scalp.
- Anogenital predominance: Vulva (65%), perianal (20%).
- Axillary involvement: Less common, 10-15%.
- Rare ectopic sites: Scalp, umbilicus, thigh.
Histology
The hallmark of EMPD is single-cell or small-group infiltration of the epidermis by large, round Paget cells with abundant pale cytoplasm, hyperchromatic nuclei, and prominent nucleoli. These cells exhibit glandular differentiation, forming ducts or mucin droplets. The epidermis shows acanthosis, hyperkeratosis, and parakeratosis, with Paget cells distributed at all levels, including the basal layer and adnexa.
In primary EMPD, involvement is confined to the epidermis (in situ). Invasion into the dermis occurs in 10-20% of cases, indicated by Paget cells below the dermal-epidermal junction. Secondary EMPD shows pagetoid spread from underlying adnexal or dermal tumors, often with associated desmoplastic stroma.
| Feature | Primary EMPD | Secondary EMPD |
|---|---|---|
| Paget cell distribution | Random, epidermis-only | Upward from adnexa/dermis |
| Dermal invasion | Rare (<15%) | Frequent (30-50%) |
| Mucin production | Prominent | Variable |
| Associated tumor | None | Often present |
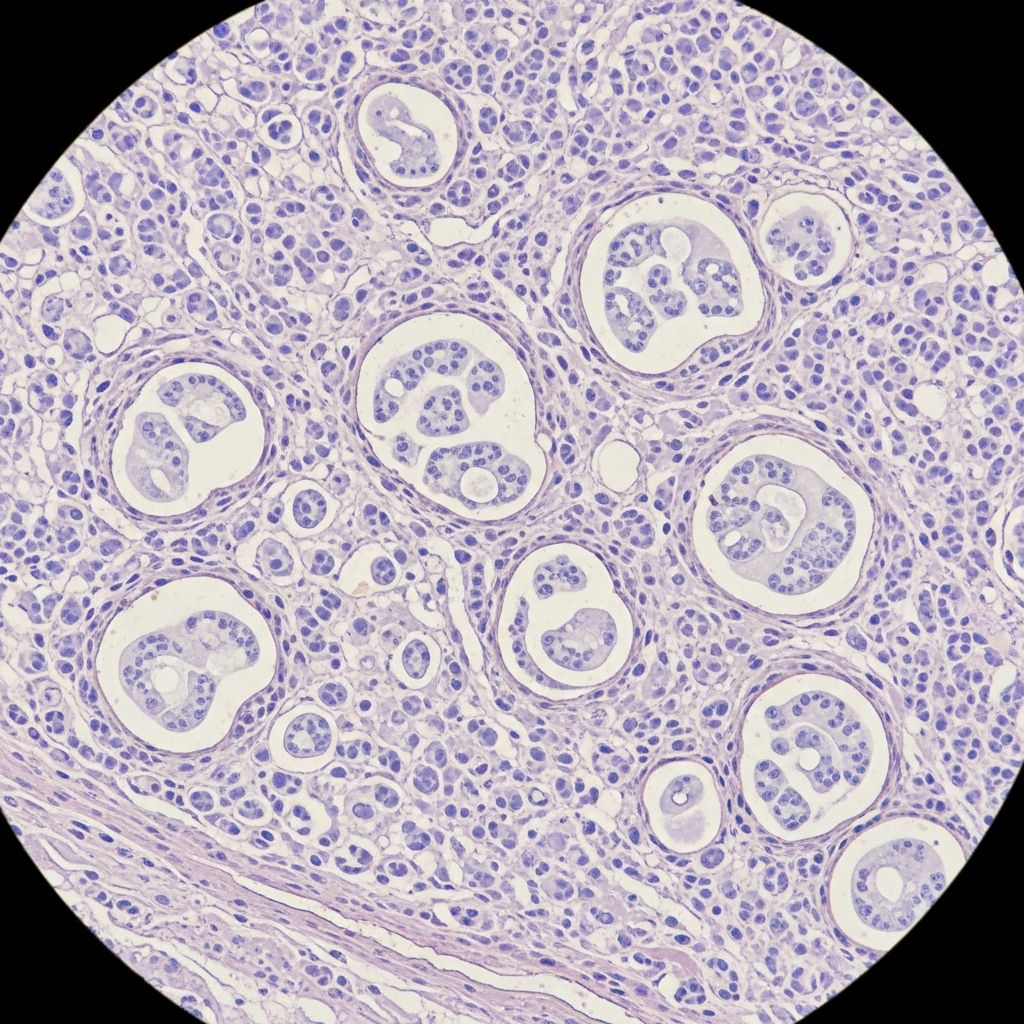
Microscopic images
Scanning power reveals an irregular plaque with epidermal thickening. Low power shows pale cells scattered throughout a thickened epidermis forming gland-like structures. Higher magnification highlights Paget cells with abundant pale cytoplasm, large nuclei, and mucin droplets. Ductal differentiation and signet-ring cells are evident in some fields.
Histochemistry
Mucin histochemistry confirms glandular origin: Paget cells stain positively with periodic acid-Schiff (PAS), Alcian blue (pH 2.5), and mucicarmine, demonstrating intracytoplasmic mucin. These stains aid in distinguishing EMPD from mimics like melanoma or Bowen disease, which lack mucin.
- PAS: Highlights glycogen and mucopolysaccharides in cytoplasm.
- Alcian blue: Acid mucins at low pH.
- Mucicarmine: Specific for epithelial mucin.
Immunohistochemistry
IHC is pivotal for diagnosis and classification. Paget cells in EMPD express cytokeratins (CK7+, CK20 variable), epithelial membrane antigen (EMA+), and mucin markers. GCDFP-15 and HER2 are often positive in primary EMPD, while CDX-2 and CK20 favor secondary gastrointestinal origin.
| Marker | Primary EMPD | Secondary (GI/Uro) | Melanoma | Bowen |
|---|---|---|---|---|
| CK7 | + | +/- | – | – |
| CK20 | – | + | – | – |
| GCDFP-15 | + | – | – | – |
| CDX-2 | – | + | – | – |
| S100 | – | – | + | – |
Primary vs. Secondary Discrimination: CK7+/CK20- with GCDFP-15+ suggests primary; CK7-/CK20+ with CDX-2+ indicates secondary from colorectum. HER2 overexpression (seen in 20-50%) predicts response to targeted therapy.
Electron microscopy
Ultrastructurally, Paget cells display abundant cytoplasm with mucin vacuoles, tonofilaments, desmosomes, and well-formed Golgi apparatus. Junctional complexes and ductal lumen formation confirm apocrine differentiation, distinguishing from non-glandular pagetoid diseases.
Differential diagnosis
Histological mimics include:
- Melanoma (pagetoid spread): S100+, melan-A+, lacks mucin/CK7.
- Bowen disease (SCC in situ): Full-thickness atypia, CK5/6+, p63+.
- Clear cell acanthoma:
- Glandular but CK7-, no pagetoid spread.
- Seborrhoeic keratosis (claro variant): Basal confinement, horn cysts.
- Toker cells: Benign, adnexal, CK7+ but small, no atypia.
IHC panels resolve most differentials: EMPD is CK7+/S100-/p63-.
Underlying malignancy
Secondary EMPD mandates screening for internal carcinoma: colonoscopy, cystoscopy, mammography, etc. Up to 40% harbor associated cancers, emphasizing multidisciplinary evaluation post-diagnosis.
Prognosis
Primary in situ EMPD has excellent prognosis post-excision (recurrence 30-50% due to margins). Invasive/dermal disease risks lymph node metastasis (10-20%). Secondary forms depend on primary tumor stage.
Frequently Asked Questions
What are the key pathological features of EMPD?
Large pale Paget cells with mucin, CK7+, scattered throughout epidermis.
How to distinguish primary from secondary EMPD?
IHC: Primary CK7+/CK20-/GCDFP+; Secondary CK20+/CDX2+.
Is mucin staining always positive?
80-90% cases; rare non-mucinous variants require IHC.
What is the recurrence rate?
High (up to 50%) due to subclinical spread; Mohs preferred.
Role of HER2 in EMPD?
Overexpressed in 30%; trastuzumab-responsive subset.
References
- Extramammary Paget disease — DermNet NZ. 2023. https://dermnetnz.org/topics/extramammary-paget-disease
- Extramammary Paget’s Disease: Symptoms, Causes & Treatment — Cleveland Clinic. 2024-05-15. https://my.clevelandclinic.org/health/diseases/24266-extramammary-pagets-disease
- Anatomic Subtype Differences in Extramammary Paget Disease — JAMA Dermatology. 2023-06-07. https://jamanetwork.com/journals/jamadermatology/fullarticle/2815630
- Extramammary Paget disease (EMPD): What you need to know — MD Anderson Cancer Center. 2022-12-01. https://www.mdanderson.org/cancerwise/extramammary-paget-disease-what-you-need-to-know.h00-159778812.html
- Insights Into Mammary and Extramammary Paget’s Disease: Diagnosis, Management, and Recent Advances — Cureus (Peer-reviewed). 2024-10-15. https://www.cureus.com/articles/348899-insights-into-mammary-and-extramammary-pagets-disease-diagnosis-management-and-recent-advances
Read full bio of Sneha Tete