The Gut-Brain Connection: How Your Microbiome Affects Mental Health
Discover how your gut microbiome influences mood, cognition, and neurological health through the gut-brain axis.
The Gut-Brain Connection: Understanding the Microbiome’s Influence on Mental Health
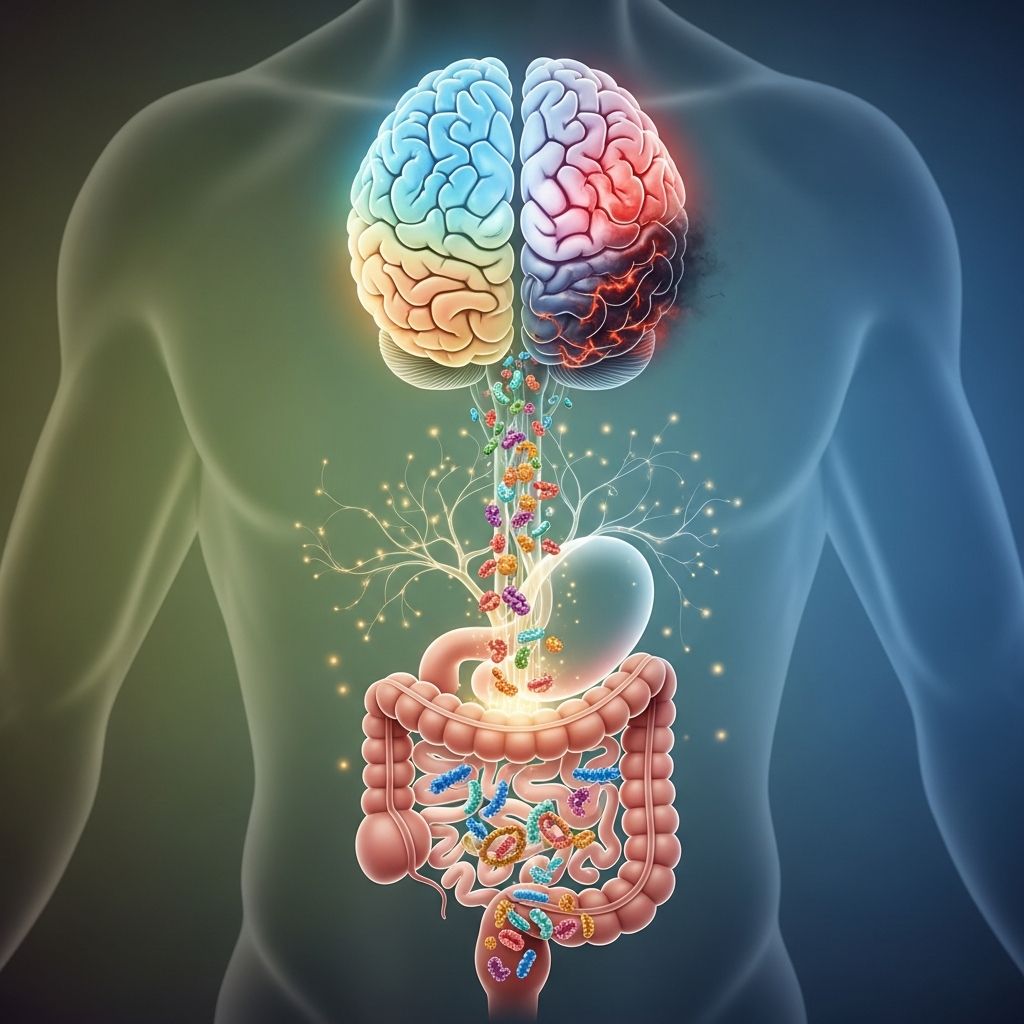
The human body operates as an interconnected system of remarkable complexity. One of the most fascinating discoveries in modern medicine is the profound relationship between your digestive system and your brain—a connection that extends far beyond simple nutrient absorption. This bidirectional communication network, known as the gut-brain axis, has revolutionized our understanding of mental health, cognitive function, and overall wellness. Recent research demonstrates that the trillions of microorganisms living in your gastrointestinal tract play a crucial role in regulating mood, behavior, and neurological function.
What Is the Gut-Brain Connection?
The gut-brain connection, also referred to as the gut-brain axis, represents a complex bidirectional communication system that links your gut microbiome to your central nervous system. Rather than operating independently, your digestive system and brain engage in constant dialogue, exchanging chemical signals that influence physiological and cognitive functions. This communication pathway involves multiple systems working in concert—your nervous system, hormonal system, immune system, and the trillions of bacteria residing in your gastrointestinal tract.
Your gut microbiome is an extraordinarily diverse ecosystem comprising trillions of microorganisms, including bacteria, viruses, and fungi. These microscopic inhabitants play essential roles in digestion, nutrient absorption, and immune function. However, emerging research reveals that the microbiome’s influence extends well beyond digestive health. The gut microbiota actively participates in regulating central nervous system function, directly impacting emotional well-being, cognitive performance, and susceptibility to neurological and psychiatric disorders.
How the Gut and Brain Communicate
Understanding the mechanisms through which your gut and brain communicate provides insight into why digestive health is inseparable from mental health. Multiple pathways enable this remarkable dialogue:
The Vagus Nerve: The Main Communication Highway
The vagus nerve serves as the primary information superhighway between your brain and gut, forming a direct neural connection that transmits signals bidirectionally. This cranial nerve contains approximately 100,000 nerve fibers and functions as the main pathway through which your enteric nervous system—often called the “second brain”—communicates with your central nervous system. The vagus nerve continuously monitors your gut’s health, detecting inflammation and changes in bacterial composition, then relaying this information to your brain. When activated through practices such as deep breathing, the vagus nerve can calm both your mind and gut, reducing stress and improving digestive function.
Neurotransmitter Production
Your gut produces numerous neurotransmitters—chemical messengers that enable nerve cells to communicate. In fact, your gastrointestinal tract manufactures approximately 90 percent of your body’s serotonin, the neurotransmitter essential for mood regulation. Your gut microbiota actively participates in neurotransmitter synthesis, producing gamma-aminobutyric acid (GABA), which reduces anxiety, and other important signaling molecules. These neurotransmitters produced in your gut influence pain perception, muscle contraction, digestion function, and mood regulation, demonstrating how closely digestive health and mental state are intertwined.
Short-Chain Fatty Acids (SCFAs)
When you consume dietary fiber, your gut bacteria ferment it, producing short-chain fatty acids including butyrate, propionate, and acetate. These small molecules possess a remarkable ability to cross the blood-brain barrier and interact directly with brain receptors. SCFAs produce multiple beneficial effects on the central nervous system, including reducing inflammation, improving mood, and enhancing cognitive function. The production of adequate SCFAs depends on maintaining a diverse, healthy microbiome through fiber-rich nutrition.
Hormonal Signaling
Your gastrointestinal tract produces hormones that directly influence brain function and mood. The gut microbiota regulates the production of these hormonal messengers, which travel through your bloodstream to affect brain chemistry and behavior. This hormonal dialogue influences appetite regulation, stress response, and emotional processing.
Immune System Modulation
Your gastrointestinal system represents your body’s largest immune organ, and your microbiota plays a critical role in regulating immune responses. A healthy microbiome maintains the intestinal barrier, preventing harmful substances from entering the bloodstream. When the microbiome becomes imbalanced, intestinal permeability increases—a condition commonly called “leaky gut”—allowing inflammatory molecules to enter circulation and trigger systemic inflammation that reaches the brain, affecting cognition and mood.
The Role of Microbiome Composition in Brain Health
The specific bacteria inhabiting your gut directly influence your neurological and mental health. Your microbiome composition affects brain development and plasticity by secreting various neurotrophins and proteins, such as brain-derived neurotrophic factor (BDNF), which supports neuronal growth and survival. Dysbiosis—an imbalance in the microbial community characterized by reduced diversity and altered bacterial composition—has been linked to numerous psychiatric and neurological conditions.
Research demonstrates that individuals experiencing depression, anxiety, autism spectrum disorder, and other psychiatric conditions frequently exhibit distinct alterations in their gut microbiota. For example, people with depression often show reduced levels of beneficial bacteria that produce short-chain fatty acids with antidepressant effects. Similarly, individuals with anxiety disorders may have imbalanced microbiota that produce insufficient GABA and other calming neurotransmitters.
Gut-Brain Connection and Mental Health Disorders
Depression
The gut-brain axis plays a significant role in depression pathophysiology. Dysbiotic microbiota produce reduced levels of mood-supporting metabolites, while simultaneously increasing inflammation that crosses the blood-brain barrier. This dual mechanism—decreased production of beneficial compounds and increased inflammatory signaling—contributes to depressive symptoms. Treatment strategies targeting the microbiome show promise in alleviating depressive symptoms.
Anxiety Disorders
Anxiety and the gut are intimately connected through multiple communication pathways. A dysbiotic microbiome produces insufficient GABA and other anxiolytic neurotransmitters while simultaneously promoting inflammatory responses that trigger anxiety symptoms. Stress itself can disrupt microbiota composition, creating a vicious cycle where anxiety damages the microbiome, which in turn worsens anxiety.
Cognitive Function and Neurodegenerative Diseases
Your gut communicates inflammation status to your brain, directly affecting cognitive function. A healthy microbiome maintains low systemic inflammation, preserving cognitive clarity and focus. Conversely, dysbiosis promotes neuroinflammation associated with cognitive decline and increased risk of neurodegenerative conditions such as Alzheimer’s disease. Studies of animals with disrupted gut microbiomes demonstrate cognitive impairments including anxiety, depression, and impaired learning and memory.
Autism Spectrum Disorder
Research indicates that individuals on the autism spectrum frequently exhibit distinct microbiota alterations. The mechanisms through which dysbiosis contributes to autism symptoms likely involve neuroinflammation, altered neurotransmitter production, and impaired intestinal barrier function.
How Diet and Lifestyle Impact the Gut-Brain Axis
Your daily choices profoundly influence both your microbiota composition and brain health through the gut-brain axis. Supporting microbiota diversity through dietary choices, stress management, and physical activity creates beneficial effects across multiple body systems:
Dietary Influences
Fiber-rich foods nourish beneficial bacteria, promoting SCFA production and maintaining microbial diversity. Fermented foods containing probiotics introduce beneficial microorganisms. Conversely, highly processed foods, excessive sugar, and artificial additives promote dysbiosis. Your dietary choices directly determine which bacterial populations thrive, thereby influencing neurotransmitter production and inflammation levels.
Stress Management
Chronic stress disrupts microbiota composition while also increasing intestinal permeability. Practices that reduce stress—including meditation, deep breathing, and physical activity—preserve microbiota health and reduce systemic inflammation. The stress-reducing effects of activating the vagus nerve through breathing exercises benefit both mental state and gut function simultaneously.
Physical Activity
Regular exercise promotes microbiota diversity and metabolite production while simultaneously improving mood and cognitive function through multiple mechanisms. This creates a positive feedback loop where exercise benefits the microbiome, which then supports better mental health.
Sleep Quality
Sleep disruption damages microbiota composition and increases intestinal permeability, allowing inflammatory molecules to enter circulation. Prioritizing consistent sleep supports both microbiota health and neurological function.
Therapeutic Strategies Targeting the Gut-Brain Axis
Dietary Approaches
Increasing dietary fiber from vegetables, fruits, legumes, and whole grains promotes beneficial bacteria and SCFA production. Mediterranean-style diets rich in polyphenols from olive oil, nuts, and berries demonstrate particular benefit for mental health. Probiotic foods including yogurt, kefir, sauerkraut, and kimchi introduce beneficial organisms.
Targeted Supplementation
Specific probiotic strains show promise in clinical research for depression, anxiety, and cognitive function. Prebiotic supplements that feed beneficial bacteria may support mental health. However, supplementation should complement rather than replace dietary approaches and lifestyle modifications.
Stress Reduction Techniques
Meditation, yoga, and deep breathing activate the vagus nerve, reducing both stress and systemic inflammation while supporting microbiota diversity. These practices simultaneously benefit mental state and gut health through the gut-brain axis.
The Bidirectional Nature of the Connection
The gut-brain relationship operates bidirectionally—your gut influences your brain, and your brain influences your gut. When your mental health deteriorates, negative feedback from your brain to your gut can impair digestion and nutrient absorption. Conversely, when your mood and mental state improve, this positive feedback enhances your gut’s ability to function optimally. This bidirectional nature means that supporting mental health through conventional approaches simultaneously supports gut health, creating synergistic benefits.
Frequently Asked Questions
Q: Can probiotics treat depression and anxiety?
A: While research shows promising results for specific probiotic strains in supporting mental health, probiotics work best as part of a comprehensive approach including dietary changes, stress management, and conventional treatment when needed. Probiotics alone are not a replacement for established mental health treatments.
Q: How long does it take to restore a healthy microbiome?
A: Microbiota composition can begin changing within days of dietary modifications, though establishing stable, diverse populations typically requires several weeks to months of consistent healthy practices.
Q: What foods harm the gut-brain axis?
A: Highly processed foods, excess sugar, artificial additives, and excessive alcohol promote dysbiosis and increase intestinal permeability, damaging the gut-brain axis. These foods simultaneously promote systemic inflammation affecting brain function.
Q: Can stress alone damage my microbiome?
A: Yes, chronic stress disrupts microbiota composition and increases intestinal permeability, even without dietary changes. This demonstrates why stress management is essential for maintaining a healthy gut-brain axis.
Q: Is the gut-brain connection the same for everyone?
A: While the mechanisms of the gut-brain axis are universal, individual responses vary based on genetics, existing microbiota composition, health status, and other factors. Personalized approaches often prove most effective.
Key Takeaways
The gut-brain connection represents one of the most significant discoveries in modern medicine, revealing that mental health and digestive health are inseparable. Your gut microbiota produces neurotransmitters, metabolites, and hormones that directly influence mood, cognition, and behavior. Supporting your microbiome through dietary choices, stress management, physical activity, and adequate sleep simultaneously supports your mental health and cognitive function. As research continues to illuminate the mechanisms underlying the gut-brain axis, healthcare professionals increasingly recognize that addressing digestive health is essential for comprehensive mental health treatment. By understanding and supporting your gut-brain connection through lifestyle modifications, you can enhance both your mental well-being and overall health.
References
- The Gut Brain Connection — Scientific Research Publishing (SCIRP). 2024. https://www.scirp.org/journal/paperinformation?paperid=132008
- The Gut-Brain Axis: The Missing Link in Depression — National Center for Biotechnology Information, U.S. National Library of Medicine. 2015. https://pmc.ncbi.nlm.nih.gov/articles/PMC4662178/
- What is the Gut-Brain Connection? — HelpGuide International. 2024. https://www.helpguide.org/wellness/nutrition/gut-brain-connection
- The Gut and the Brain — Harvard Medical School. 2024. https://hms.harvard.edu/news-events/publications-archive/brain/gut-brain
- How Gut Bacteria Influence the Brain and Behavior — National Institute of Mental Health (NIMH), National Institutes of Health. 2024. https://www.nimh.nih.gov/
Read full bio of Sneha Tete