Gynecomastia Surgery: Male Breast Reduction Guide
Complete guide to gynecomastia surgery: procedures, recovery, and what to expect.
Understanding Gynecomastia Surgery
Gynecomastia surgery, also known as male breast reduction or reduction mammaplasty, is a surgical procedure designed to reduce the size of enlarged breast tissue in males. This procedure addresses a common condition called gynecomastia, which involves an abnormal enlargement of male breast tissue. Men choose to undergo this surgery for various reasons, including improving self-confidence, enhancing their physical appearance, and reducing discomfort that can result from larger breasts.
Gynecomastia can develop during adolescence due to hormonal changes, or it may affect older men as hormone levels shift with age. The condition can also result from obesity, certain medications, or hormonal imbalances. In severe cases, excess breast tissue causes the breasts to sag and the areola (the dark skin surrounding the nipple) to stretch, creating a more feminine appearance that many men find distressing.
What Is Gynecomastia?
Gynecomastia refers to the enlargement of breast tissue in males, which is a benign condition but can significantly impact a man’s self-esteem and quality of life. The condition can affect one or both breasts and ranges from mild to severe. When gynecomastia does not resolve naturally within six months or when it disrupts an individual’s self-confidence, surgical intervention becomes the recommended treatment approach.
Research indicates that gynecomastia affects a substantial portion of the male population, with studies suggesting that up to half of all healthy men may experience this condition at some point in their lives. Despite its prevalence, many men are unaware of available treatment options, and awareness about the condition continues to grow through specialized breast health programs.
Pre-Surgery Consultation and Evaluation
Before undergoing gynecomastia surgery, your healthcare provider will conduct a comprehensive consultation to assess your candidacy and discuss your goals. During this initial appointment, your provider will:
- Review your complete medical history to identify any underlying conditions or medications that may contribute to gynecomastia
- Perform a thorough physical examination, measuring your breast tissue and assessing skin quality
- Screen you for male breast cancer to ensure the enlarged tissue is not malignant
- Order laboratory tests, such as a complete blood count (CBC), to evaluate your overall health status
- Take photographs of your breasts for documentation and surgical planning purposes
This comprehensive evaluation ensures that your surgeon understands your specific situation and can recommend the most appropriate surgical technique for your needs. Your provider will also discuss your desired outcomes and help you establish realistic expectations for the procedure.
Surgical Techniques for Gynecomastia Surgery
Gynecomastia surgery employs different techniques depending on the amount of excess tissue and the patient’s desired appearance. Your surgeon will recommend the most appropriate approach based on your individual circumstances.
Liposuction Technique
In cases where excess breast tissue is primarily fatty in composition, surgeons may use liposuction as the primary treatment method. During this technique, the surgeon makes several small incisions and inserts a thin suction cannula (a hollow tube) attached to a vacuum device. The surgeon works the cannula back and forth under the skin to break up and remove excess fat cells. Before suctioning, saline solution may be injected into the breast tissue to help break up fatty deposits, making removal easier. This minimally invasive approach results in smaller scars and typically requires less recovery time compared to more extensive surgical techniques.
Excision Technique
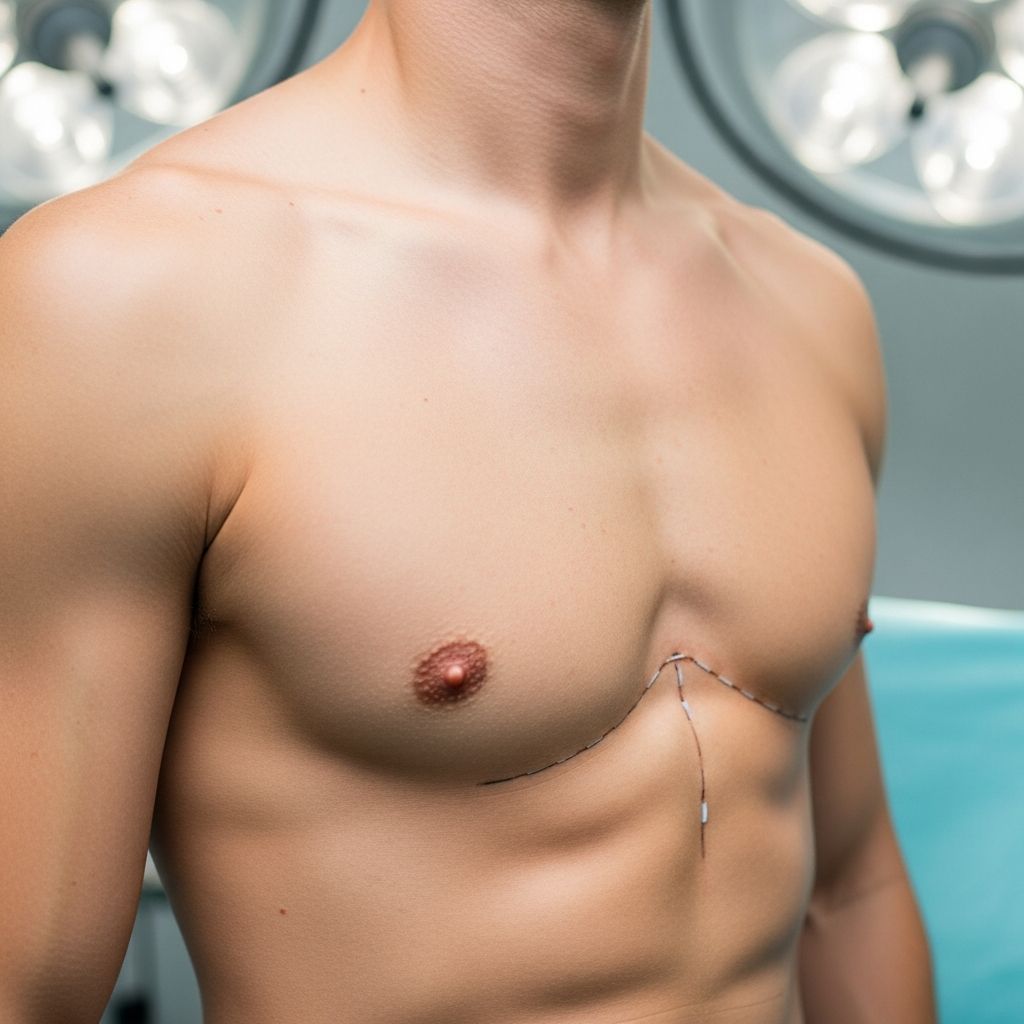
When patients have excess skin, fat, and glandular tissue, your provider may recommend excision, which involves larger incisions to remove breast tissue directly. This technique allows the surgeon to remove both fatty and glandular components of enlarged breast tissue. During excision, the surgeon may also reposition the nipple and areola to a more natural location, particularly in cases where the areola has stretched due to tissue enlargement. The incision patterns, lengths, and locations vary based on the size of the breasts and your desired aesthetic outcome.
Combined Approach
Many patients benefit from a combination of excision and liposuction, often referred to as a hybrid approach. This technique allows the surgeon to remove both glandular tissue through direct excision and fatty deposits through liposuction, providing comprehensive tissue removal and optimal contouring results. Your surgeon will evaluate your specific situation and recommend the combination of techniques that will produce the best results for your body type and goals.
The Surgical Procedure
Understanding what happens during gynecomastia surgery can help you prepare mentally and physically for the procedure. The operation is typically performed as an outpatient procedure, meaning you will return home the same day.
Anesthesia Administration
Before beginning the surgical procedure, you will receive general anesthesia administered through an intravenous line in your arm. General anesthesia ensures that you remain asleep throughout the procedure and experience no pain during surgery. Your anesthesiologist will monitor your vital signs continuously throughout the operation to ensure your safety.
Tissue Removal and Contouring
Once you are asleep, your surgeon will proceed with the planned technique or combination of techniques. Whether using liposuction, excision, or both, the goal is to remove excess tissue while creating a natural-appearing, masculine chest contour. The surgeon carefully removes tissue while maintaining appropriate nipple-areola positioning and ensuring smooth transitions between treated and untreated areas.
Nipple Repositioning
In cases where the nipple-areola complex has shifted due to tissue enlargement or where the surgeon needs to remove significant tissue, the nipple may be temporarily detached and repositioned to a more aesthetically pleasing location. This ensures that the final result appears natural and proportionate to the chest.
Drain Placement
Your surgeon may place thin tubes (drains) under your skin during the procedure. These drains prevent fluid and blood accumulation during the early healing phase. The fluid collects in a receptacle or bulb attached to the drain tube, which your surgeon will remove once adequate healing has occurred and fluid production has diminished.
Recovery and Aftercare
Proper post-operative care is essential for achieving optimal results and minimizing complications. Your recovery process will include several important components.
Immediate Post-Operative Period
After surgery, you will have bandages and a supportive garment (compression vest or chest binder) around your chest. This supportive garment serves multiple purposes: it supports your chest wall during healing, reduces swelling, and helps your skin conform to its new contours. You will need to arrange for someone to drive you home after surgery, as the effects of general anesthesia make it unsafe for you to operate a vehicle.
Pain Management
Your provider will prescribe medications to relieve pain and manage discomfort during the recovery period. These medications also help reduce swelling and lower the risk of infection. Take pain medications as directed and do not hesitate to contact your surgeon if pain becomes severe or unmanageable.
Drain Care
If drains were placed during surgery, you will need to monitor them regularly and empty the fluid as instructed by your surgical team. Keep the drain sites clean and dry, and watch for signs of infection such as increasing redness, warmth, or foul-smelling drainage.
Activity Restrictions
During the initial recovery period, you should limit strenuous activities, heavy lifting, and intense exercise. Your surgeon will provide specific guidelines about when you can gradually return to normal activities. Most patients can resume light activities within a few weeks but should wait several weeks to months before returning to heavy exercise and contact sports.
Incision Care
Keep your incisions clean and dry as they heal. Follow your surgeon’s specific instructions regarding wound care, and watch for signs of infection such as increased redness, swelling, warmth, or drainage. Avoid submerging incisions in water until they have healed sufficiently.
Results and Benefits
Gynecomastia surgery delivers significant aesthetic and psychological benefits for most patients. The procedure effectively removes excess breast tissue, creating a flatter, more masculine chest contour. Many men report substantial improvements in self-confidence and body image following surgery. Additionally, the procedure can reduce physical discomfort that may have resulted from excess breast tissue, particularly during activities requiring jumping and running.
The results of gynecomastia surgery are typically long-lasting, though maintaining a healthy weight and lifestyle helps preserve the surgical outcome. Most patients experience satisfaction with their results and report that the procedure significantly improved their quality of life.
Risks and Complications
Like any surgical procedure, gynecomastia surgery carries certain risks. Potential complications include:
- Reaction to general anesthesia
- Bleeding and excessive blood loss
- Blood clots and deep vein thrombosis
- Infection at the incision sites
- Changes in nipple sensation or breast sensation
- Visible scarring
- Cardiac and pulmonary complications
- Poor wound healing
- Unsatisfactory aesthetic results
However, serious complications are relatively uncommon when the procedure is performed by a qualified, experienced surgeon. Discussing these risks openly with your provider helps you make an informed decision about whether surgery is appropriate for you.
Combination Procedures and Advanced Techniques
Recent innovations in gynecomastia surgery have improved patient outcomes and reduced undesirable aesthetic complications. Some surgeons now employ advanced reconstructive techniques that utilize existing tissue to enhance chest contouring and prevent the development of a concave or “dished-out” appearance that can sometimes result from traditional surgical approaches. These advanced techniques may involve repositioning and augmenting the pectoralis muscle to create more natural-appearing, aesthetically pleasing chest contours.
Frequently Asked Questions
Q: How long does gynecomastia surgery take?
A: The duration varies depending on the surgical technique and extent of tissue removal, but most procedures typically take one to two hours. Your surgeon will provide a more specific time estimate during your consultation.
Q: When can I return to work?
A: Most patients can return to desk-based work within one to two weeks. However, if your job involves physical labor or heavy lifting, you may need additional time off. Your surgeon will provide specific guidance based on your job requirements.
Q: Will there be visible scars?
A: Scarring depends on the surgical technique used. Liposuction results in minimal scarring from small incisions, while excision techniques produce larger scars that gradually fade over time. Your surgeon can discuss scar placement and management strategies during your consultation.
Q: Can gynecomastia recur after surgery?
A: Recurrence is unlikely when glandular tissue is properly removed. However, significant weight gain or hormonal changes could potentially lead to recurrence. Maintaining a stable weight and healthy lifestyle helps preserve your surgical results.
Q: How soon will I see final results?
A: While initial results are visible immediately after surgery, final results typically emerge over three to six months as swelling resolves and the chest takes its final shape.
Q: Is gynecomastia surgery covered by insurance?
A: Insurance coverage depends on whether the procedure is deemed medically necessary or purely cosmetic. If gynecomastia causes significant physical discomfort or psychological distress, insurance may provide coverage. Contact your insurance provider for specific information about your plan.
References
- Gynecomastia Surgery (Male Breast Reduction): What to Expect — Cleveland Clinic. 2022-08-18. https://my.clevelandclinic.org/health/treatments/24022-gynecomastia-surgery
- Enlarged Male Breast Tissue (Gynecomastia): What It Is, Causes, Diagnosis & Treatment — Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/16227-enlarged-male-breast-tissue-gynecomastia
- Cleveland Clinic Abu Dhabi Pioneers Reconstructive Technique to Improve Surgical Outcomes for Patients with Gynecomastia — Cleveland Clinic Abu Dhabi. https://www.clevelandclinicabudhabi.ae/en/media-center/news/ccad-pioneers-reconstructive-technique-to-improve-surgical-outcomes-for-patients-with-gynecomastia
- Gynecomastia: Its Features, and When and How to Treat It — Cleveland Clinic Journal of Medicine. https://www.ccjm.org/content/71/6/511
- Gynecomastia Surgery: Safety and Risks — Galani’s Plastic Surgery. https://galanisplasticsurgery.com/blog/gynecomastia-surgery-safety-and-risks/
Read full bio of Sneha Tete