Herpes Simplex
Comprehensive guide to herpes simplex virus infections: causes, clinical features, diagnosis, and management strategies for healthcare professionals.
What is herpes simplex?
Herpes simplex is a viral infection caused by the herpes simplex virus (HSV). It leads to painful blisters or ulcers on the skin or mucous membranes, most commonly around the mouth (orolabial herpes) or genitals (genital herpes). HSV establishes lifelong latency in sensory ganglia after primary infection, with periodic reactivation causing recurrent episodes.
Two main types exist: HSV-1, traditionally associated with orofacial infections (e.g., cold sores), and HSV-2, primarily causing genital herpes. However, overlap is common; HSV-1 increasingly causes genital infections via oral-genital contact. Globally, HSV prevalence is high: over 3.7 billion people under 50 have HSV-1, and 491 million aged 15-49 have HSV-2.
Related content
Virology
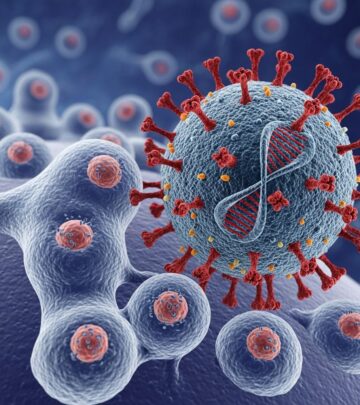
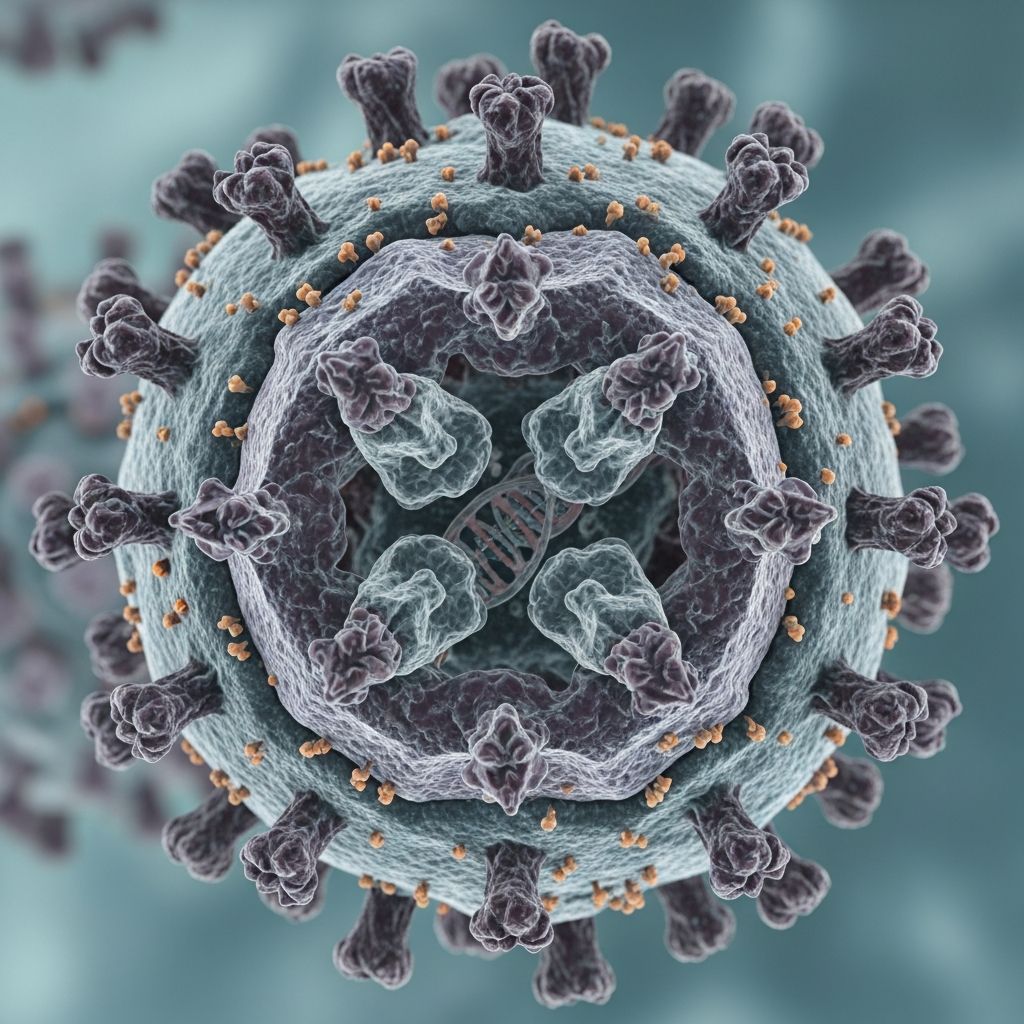
HSV belongs to the Alphaherpesvirinae subfamily of Herpesviridae, enveloped double-stranded DNA viruses measuring 150–200 nm. The genome encodes over 80 proteins, including glycoproteins essential for cell entry (e.g., gB, gC, gD, gH/gL). The viral envelope fuses with host cell membranes, enabling replication in epithelial cells and neurons.
After primary infection, HSV travels retrogradely along sensory nerves to dorsal root ganglia (trigeminal for HSV-1, sacral for HSV-2), establishing latency. Reactivation occurs due to triggers like UV light, stress, or immunosuppression, with anterograde transport back to skin/mucosa causing lesions. Viral shedding happens even asymptomatically, facilitating transmission.
Transmission
HSV spreads via direct contact with infected skin, mucosa, or secretions, including during asymptomatic shedding. Key routes include:
- Oral-oral contact (HSV-1 cold sores via kissing).
- Genital-genital, oral-genital, or anal contact (HSV-2 predominant).
- Autoinoculation (e.g., eye or finger infections).
- Vertical transmission (neonatal herpes from maternal genital lesions during birth).
| Type of Contact | HSV Spread Example |
|---|---|
| Genital-to-genital | HSV-2 genital herpes transmission |
| Oral-to-genital | HSV-1 causing genital herpes |
| Skin-to-sore | Herpetic whitlow via lesion contact |
Incubation is 2–12 days (typically 4 days). Primary infections are often severe; recurrences milder and less frequent.
Clinical features
Primary infection
Symptoms appear 2–14 days post-exposure: prodrome of tingling/burning, followed by clustered vesicles on erythematous base that ulcerate, crust, and heal in 7–10 days without scarring. Systemic features include fever, lymphadenopathy, malaise. Two-thirds are asymptomatic.
- Orolabial (gingivostomatitis): Vesicles on lips, tongue, gingiva; painful swallowing, drooling in children.
- Genital herpes: Vulval/vaginal in women, penile/scrotal in men; dysuria, sacral pain. Cervicitis or proctitis possible.
Recurrent infection
Shorter (3–7 days), localized, preceded by prodrome. Triggers: sunlight, stress, menses, illness. Recurrent labial herpes affects 20–40% of adults; genital recurrence rates higher for HSV-2 (80–90%) than HSV-1.
Immunocompromised patients
Severe, chronic, atypical presentations: large ulcers, dissemination to viscera (e.g., esophagitis, pneumonia, encephalitis).
Neonatal herpes
Rare but devastating (60% mortality untreated); skin-eye-mucosa (SEM), CNS, or disseminated disease. Most from HSV-2 maternal primary infection near delivery.
Other sites
- Herpetic whitlow: Finger pulp vesicles in healthcare workers/children (HSV-1/2).
- Herpes gladiatorum: Wrestlers’ trunk/neck lesions (HSV-1).
- Herpetic keratitis: Dendritic corneal ulcers (HSV-1), vision-threatening.
- HSV proctitis: MSM with severe anorectal pain, discharge.
Diagnosis
Clinical diagnosis is reliable for typical recurrent lesions but confirm primaries/atypical cases via lab tests.
| Method | Sensitivity/Specificity | Notes |
|---|---|---|
| Viral culture | 50–70% (lower for recurrences) | Gold standard historically; swab fresh vesicle base. |
| PCR (lesion/CSF) | 95–100%/97% | Preferred; detects HSV DNA rapidly. |
| Tzanck smear | 60–70% | Multinucleate giant cells; low specificity. |
| Serology (type-specific IgG) | N/A | Confirms prior exposure; IgM unreliable. |
For encephalitis: CSF PCR (gold standard, 98% sensitive); MRI, EEG supportive. Neonatal: Surface cultures + CSF PCR.
Differential diagnosis
- Primary: Aphthous ulcers, hand-foot-mouth, erythema multiforme, impetigo, candidiasis, syphilis, chancroid.
- Recurrent labial: Impetigo, angular cheilitis, erythema multiforme.
- Genital ulcers: Syphilis, chancroid, lymphogranuloma venereum, Behçet syndrome.
Disease severity
Primary genital herpes is most severe; recurrences decrease over time. HSV-2 recurs 4x more than HSV-1. Complications: Urinary retention, aseptic meningitis, transverse myelitis (rare).
Management
General measures
- Saltwater compresses, petroleum jelly for crusts.
- Analgesics (paracetamol), topical anesthetics (lidocaine).
- Avoid triggers: sunscreen, stress reduction.
Antivirals
Reduce duration/severity; suppressive therapy for frequent recurrences (>6/year) or partners.
| Indication | Aciclovir | Valaciclovir | Famciclovir |
|---|---|---|---|
| Primary genital (5 days) | 400 mg TDS | 1 g BD | 250 mg TDS |
| Recurrent genital (5 days) | 400 mg TDS | 500 mg BD | 125 mg BD |
| Suppressive | 400 mg BD | 500 mg OD | 250 mg BD |
| Labial (if started <1h prodrome) | — | 2 g stat, repeat 12h | 1500 mg stat |
IV aciclovir (5–10 mg/kg TDS) for severe disease (neonatal, encephalitis, immunocompromised). Resistance rare (<1%) but increasing in HIV.
Immunocompromised
Longer courses (7–10 days), higher doses; prophylaxis if CD4 <200.
Neonatal
IV aciclovir 20 mg/kg TDS x 14–21 days; suppressive oral x 6 months.
Counselling
Discuss asymptomatic shedding (10–20% days), condom use (reduces transmission 30–50%), suppressive therapy (cuts shedding 70–95%), disclosure to partners. No cure; vaccines in trials.
Prevention
- Avoid contact during outbreaks; condoms/STI screening.
- Suppressive antivirals for discordant couples.
- C-section if maternal lesions at delivery.
Prognosis
Recurrences decline over years; no scarring unless secondary infection. Rare neuralgia. High seroprevalence means many unaware carriers.
Patient resources
Frequently asked questions (FAQs)
Q: Can herpes be cured?
A: No, HSV is lifelong, but antivirals control symptoms and reduce transmission.
Q: Is herpes only sexually transmitted?
A: Primarily yes, but autoinoculation or close contact (e.g., wrestling) possible.
Q: How do I know if I have HSV-1 or HSV-2?
A: Type-specific serology or lesion PCR distinguishes them.
Q: Can I breastfeed with herpes?
A: Yes, if lesions covered and not on breast; pump/discard if active.
Q: Does suppressive therapy prevent outbreaks forever?
A: No, but reduces frequency by 70–80%; reassess annually.
References
- Herpes Simplex Virus — BC Centre for Disease Control. 2023. https://www.bccdc.ca/health-info/diseases-conditions/herpes-simplex-virus
- Herpes Simplex Virus (HSV): Types Symptoms, & Treatment — Cleveland Clinic. 2023-05-02. https://my.clevelandclinic.org/health/diseases/22855-herpes-simplex
- Herpes Simplex Virus — Johns Hopkins ABX Guide. 2024. https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540242/all/Herpes_Simplex_Virus
- Herpes simplex infections — Primary Care Dermatology Society. 2025-07-18. https://www.pcds.org.uk/clinical-guidance/herpes-simplex
- Herpes Simplex Virus (HSV) Infections — Merck Manuals. 2024. https://www.merckmanuals.com/home/infections/herpesvirus-infections/herpes-simplex-virus-hsv-infections
- Herpes Simplex Virus: A Practical Guide to Diagnosis, Management — PubMed (J Clin Virol). 2024-02-01. https://pubmed.ncbi.nlm.nih.gov/38331482/
- Herpes – STI Treatment Guidelines — Centers for Disease Control and Prevention (CDC). 2021-07-22. https://www.cdc.gov/std/treatment-guidelines/herpes.htm
Read full bio of Sneha Tete