Hyperbaric Oxygen Therapy
Explore hyperbaric oxygen therapy: mechanism, approved uses, dermatological applications, and safety considerations for enhanced healing.
Hyperbaric oxygen therapy (HBOT) involves breathing pure oxygen in a pressurized environment to enhance oxygen delivery to tissues, promoting healing for various conditions including wounds, infections, and decompression sickness.
What is hyperbaric oxygen therapy?
Hyperbaric oxygen therapy is a medical treatment where patients inhale 100% pure oxygen inside a hyperbaric chamber pressurized to 2–3 atmospheres absolute (ATA), significantly increasing oxygen dissolution in plasma for better tissue oxygenation.
This therapy leverages Henry’s law, allowing oxygen to dissolve directly into blood plasma, bypassing hemoglobin limitations, which is crucial for hypoxic tissues. Unlike normal air (21% oxygen), HBOT uses medical-grade 100% oxygen, elevating tissue oxygen levels up to 1,000% higher than baseline.
HBOT chambers come in monoplace (single-patient, acrylic tube) or multiplace (room-sized for multiple patients) designs, with treatments lasting 60–120 minutes, often 20–40 sessions depending on the condition.
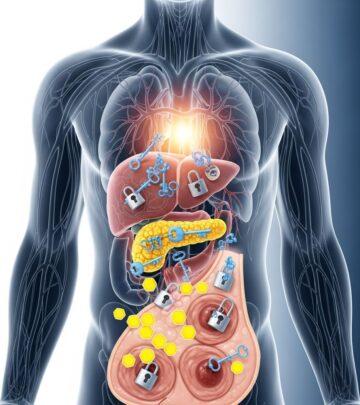
Mechanism of hyperbaric oxygen therapy
HBOT drives several physiological effects: hyperoxygenation reduces hypoxia-driven anaerobic metabolism, stimulates angiogenesis via vascular endothelial growth factor (VEGF), enhances collagen synthesis for wound repair, and exhibits antimicrobial action by generating reactive oxygen species that weaken bacteria and biofilms.
- Increased oxygen delivery: Plasma transports oxygen to ischemic tissues, supporting fibroblast proliferation and neovascularization.
- Anti-inflammatory effects: Reduces edema and cytokine release, aiding recovery in inflamed areas.
- Immune modulation: Boosts white blood cell function and stem cell mobilization for regeneration.
- Angiogenesis and tissue repair: Promotes new vessel growth and collagen production, essential for chronic wounds.
These mechanisms make HBOT particularly effective for conditions with compromised vascularity.
What is hyperbaric oxygen therapy used for?
HBOT is FDA-approved for 14 indications, primarily addressing compromised tissue perfusion. Key uses include:
- Air or gas embolism
- Carbon monoxide poisoning
- Clostridial myositis and myonecrosis (gas gangrene)
- Crush injury, compartment syndrome, and acute traumatic ischemia
- Decompression sickness
- Arterial insufficiencies (e.g., central retinal artery occlusion)
- Severe anemia
- Intracranial abscess
- Necrotizing soft tissue infections
- Refractory osteomyelitis
- Delayed radiation injury
- Compromised grafts and flaps
- Acute thermal burn injury
- Idiopathic sudden sensorineural hearing loss
Beyond approvals, HBOT shows promise in regenerative therapy, cognitive enhancement, and chronic conditions like fibromyalgia.
Hyperbaric oxygen therapy for skin disorders
In dermatology, HBOT excels for wounds and radiation-damaged skin by countering hypoxia, a barrier to healing.
Diabetic foot ulcers
HBOT stimulates granulation in Wagner grade 3+ ulcers unresponsive to standard care, with healing rates up to 85% in trials.
Venous leg ulcers
Auxiliary therapy for large, recalcitrant ulcers, promoting epithelialization via improved perfusion.
Pyoderma gangrenosum
Adjunctive for steroid-resistant cases, reducing inflammation and accelerating closure.
Radiation dermatitis and proctitis
Alleviates chronic ulcers and telangiectasia from radiotherapy by inducing angiogenesis.
Other applications
Includes calciphylaxis, livedoid vasculopathy, and compromised skin grafts, where HBOT reduces necrosis risk.
| Condition | HBOT Benefit | Evidence Level |
|---|---|---|
| Diabetic foot ulcers | 85% healing rate | FDA-approved |
| Radiation injury | Angiogenesis promotion | FDA-approved |
| Venous ulcers | Epithelialization | Adjunctive |
| Pyoderma gangrenosum | Inflammation reduction | Case series |
Hyperbaric medicine protocols
Standard protocol: 2.0–2.5 ATA for 90 minutes daily, 20–40 sessions. Diabetic wounds may require 2.4 ATA × 90 min × 30 sessions; decompression sickness uses 2.8 ATA × 30 min × multiple dives.
Monitoring includes otoscopy for barotrauma prevention and vital signs during compression/decompression phases.
Contraindications and complications of hyperbaric oxygen therapy
Absolute contraindications
- Untreated pneumothorax
- Intracranial air (e.g., post-neurosurgery)
Relative contraindications
- Recent MI (wait 4–6 weeks)
- Uncontrolled seizures
- Pregnancy (except life-threatening cases)
- Active viral infections
- COPD with CO2 retention
- Claustrophobia
Side effects
Common: Ear barotrauma (10–20%), sinus squeeze, transient myopia (from lens oxygen saturation).
Rare: Oxygen toxicity (seizures <0.1% at 2.4 ATA), pulmonary edema, claustrophobia.
- Barotrauma: Middle ear pressure injury; mitigated by auto-inflation devices.
- Oxygen toxicity: Pulmonary (chest pain) or CNS (seizures); risk rises >3 ATA.
Future directions for hyperbaric oxygen therapy
Emerging research explores HBOT in anti-aging via telomere elongation, stem cell mobilization, and neuroprotection for TBI/stroke. Regenerative potential includes liver repair post-hepatectomy and cognitive decline mitigation.
Challenges: High costs, access, and need for RCTs in off-label uses like long COVID or Alzheimer’s.
Frequently asked questions
What conditions does HBOT treat?
HBOT treats FDA-approved conditions like decompression sickness, carbon monoxide poisoning, non-healing wounds, and radiation injuries.
Is HBOT safe?
Yes, when administered properly; most side effects are mild like ear pressure, with serious risks rare (<1%).
How many sessions are needed?
Typically 20–40 sessions of 90 minutes each, tailored to the condition.
Does insurance cover HBOT?
Covered for FDA-approved indications; check with providers for specifics.
Can HBOT help with chronic fatigue or brain fog?
Promising off-label evidence exists for cognitive benefits via improved oxygenation and reduced inflammation.
References
- 5 Benefits of Hyperbaric Oxygen Therapy — Independence Health. 2023-03-01. https://www.independence.health/newsroom/2023/march/5-benefits-of-hyperbaric-oxygen-therapy/
- The Healing Power of Hyperbaric Oxygen Therapy — University Hospitals. 2022-09-01. https://www.uhhospitals.org/blog/articles/2022/09/the-healing-power-of-hyperbaric-oxygen-therapy
- Hyperbaric oxygen therapy – Mayo Clinic — Mayo Clinic. 2023-01-01. https://www.mayoclinic.org/tests-procedures/hyperbaric-oxygen-therapy/about/pac-20394380
- Hyperbaric oxygen therapy: future prospects in regenerative therapy — PMC (NCBI). 2024-04-22. https://pmc.ncbi.nlm.nih.gov/articles/PMC11097100/
- Hyperbaric Oxygen Therapy: What It Is & Benefits, Side Effects — Cleveland Clinic. 2023-01-01. https://my.clevelandclinic.org/health/treatments/17811-hyperbaric-oxygen-therapy
- Hyperbaric Oxygen Therapy (HBOT) — UC San Diego Health. 2023-01-01. https://health.ucsd.edu/care/wound/hbot/
Read full bio of Sneha Tete