Juvenile Xanthogranuloma Pathology
Detailed histopathological analysis of juvenile xanthogranuloma, a common non-Langerhans cell histiocytosis in young children.
Juvenile xanthogranuloma (JXG) is a benign, self-limited non-Langerhans cell histiocytosis primarily affecting infants and young children, characterized by a progressive histological evolution in the dermis.
Introduction
Juvenile xanthogranuloma typically manifests in young children as a smooth, pink or yellow nodule on the skin. It represents the most common form of non-Langerhans cell histiocytosis, with lesions often appearing before one year of age in 85% of cases, including one-third as congenital presentations. Histologically, JXG evolves through distinct phases, starting with early inflammatory infiltrates and progressing to foamy histiocytes and characteristic Touton giant cells. This condition arises from dermal dendrocytes and shows a male predominance in pediatric cases (up to 7:1 ratio). While primarily cutaneous, systemic involvement occurs in about 4% of cases, potentially affecting eyes, viscera, or the central nervous system.
The aetiology remains obscure but is thought to involve an unidentified infectious or physical stimulus triggering a granulomatous histiocytic response. Lesions are usually asymptomatic, firm, yellow-orange-brown papules or nodules, most commonly on the head, neck, and upper trunk, with spontaneous regression in 3–6 years for cutaneous forms.
Histology
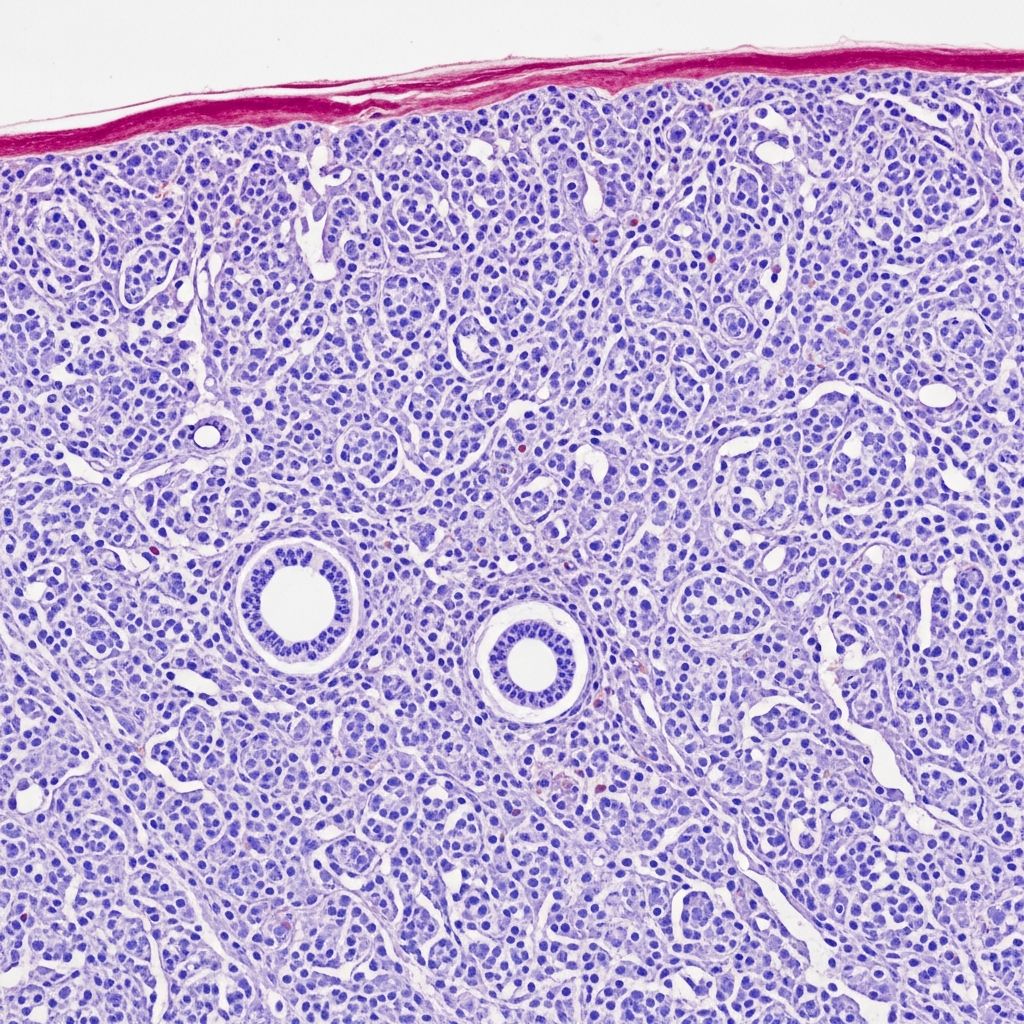
The histopathological features of JXG are distinctive and evolve over time, reflecting the lesion’s maturation. Early lesions show a dense lymphohistiocytic proliferation confined to the dermis, with rare multinucleated giant cells and blunting of rete ridges. As the lesion progresses, it develops a mixed population of foamy histiocytes (xanthomatized cells laden with lipid), Touton giant cells, lymphocytes, plasma cells, and eosinophils intermixed in the superficial dermis.
Key histological stages:
- Early phase: Dense dermal infiltrate of small histiocytes and lymphocytes, with minimal foamy change and occasional giant cells. The epidermis appears normal or slightly flattened.
- Developed phase: Prominent foamy histiocytes and characteristic Touton giant cells dominate. Touton cells feature a central wreath of nuclei surrounded by homogeneous pink cytoplasm, with peripheral foamy lipid-laden zones—best visualized on low-power magnification.
- Late phase: Histiocytes become spindled, adopting a fibrohistiocytic appearance with increased fibrosis and fewer Touton cells. Lesions may show sclerosis and partial involution.
Grossly, biopsies reveal well-demarcated, yellow-red papulonodular lesions ranging from 1 mm to 2 cm, with intense superficial dermal infiltration and preserved rete ridge architecture.
Histopathology images
Histological examination reveals the progressive changes in JXG:
- Figure 1 (Early lesion): Dense lymphohistiocytic infiltrate in the dermis with sparse giant cells (H&E).
- Figure 2 (Developed lesion): Mixture of foamy histiocytes, Touton giant cells, and inflammatory cells expanding the dermis.
- Figure 3 (Characteristic Touton cells): High-power view highlighting Touton giant cells with wreath-like nuclei and foamy periphery.
These images underscore the diagnostic hallmark of Touton giant cells, absent in mimics like xanthomas or Langerhans cell histiocytosis.
Immunohistochemistry
Immunohistochemical staining confirms the non-Langerhans nature of JXG histiocytes. Key markers include:
| Marker | Expression in JXG | Significance |
|---|---|---|
| CD68 | Strong positive | Marks lipid-laden macrophages/histiocytes. |
| CD163 | Strong positive | Specific for monocyte-macrophage lineage. |
| Factor XIIIa | Positive | Supports dermal dendrocyte origin. |
| S100 | Focal/weak or negative | Distinguishes from Langerhans cells. |
| CD1a | Negative | Rules out Langerhans cell histiocytosis. |
| Langerin (CD207) | Negative | Confirms non-Langerhans phenotype. |
Histiocytes in JXG express markers of monocyte-macrophage differentiation but lack Birbeck granules and Langerhans-specific antigens. Occasional positivity for fascin or CD4 may be seen. Ki-67 proliferation index is low, reflecting the benign nature. In systemic cases, similar profiles aid in confirming extracutaneous involvement.
Differential diagnosis
Histological mimics require careful distinction:
- Xanthoma: More lipidized foamy cells without Touton giants; clinical hyperlipidemia context.
- Langerhans cell histiocytosis: CD1a/Langerin positive, Birbeck granules on EM.
- Spitz naevus: Epithelioid melanocytes, S100 strong, HMB45 positive.
- Mastocytosis: Mast cell tryptase positive, lacks histiocytic markers.
- Rosai-Dorfman disease: Emperipolesis, S100 strong.
- Erdheim-Chester disease: Adult onset, foamy histiocytes with BRAF mutations.
Clinical correlation and IHC panel resolve most differentials. In ambiguous cases, electron microscopy shows lipid vacuoles without Birbeck granules.
Clinical features (Pathology context)
Pathology informs clinical recognition: solitary or multiple yellow-orange papules/nodules (2–15 mm), often on head/neck/trunk. Subcutaneous variants appear deeper. Multiple lesions (>5) raise systemic risk (4%), including ocular (iris hyphema, glaucoma), CNS (seizures), or visceral sites. Adult JXG is rarer, with persistent lesions.
Complications and associations
Rarely, JXG associates with neurofibromatosis type 1 (NF1) or juvenile myelomonocytic leukemia (JMML), warranting screening in atypical/multiple cases. Ocular involvement (unilateral, <2 years) risks blindness; systemic mortality 5–10%.
Diagnosis and management
Diagnosis relies on histology/IHC for typical solitary lesions; biopsy indicated for multiples or systemic suspicion. Self-resolving; excision for cosmetics or complications. Monitor systemic cases.
Frequently asked questions
What are Touton giant cells?
Touton giant cells are pathognomonic for JXG, featuring a ring of nuclei around central homogeneous cytoplasm with peripheral foamy lipid.
Is biopsy always needed for JXG?
No, for solitary typical lesions; yes for multiples, atypical sites, or systemic symptoms.
Does JXG regress spontaneously?
Yes, cutaneous lesions in 3–6 years; systemic often resolves but requires monitoring.
Can JXG affect adults?
Yes, 10% adult-onset, no sex bias, more persistent.
What is the IHC profile?
CD68/CD163+, CD1a/S100-, confirming non-Langerhans histiocytes.
References
- Juvenile xanthogranuloma pathology — DermNet NZ. 2023. https://dermnetnz.org/topics/juvenile-xanthogranuloma-pathology
- Juvenile Xanthogranuloma — StatPearls, NCBI Bookshelf, NIH. 2023-10-01. https://www.ncbi.nlm.nih.gov/books/NBK526103/
- Juvenile xanthogranuloma — DermNet NZ. 2023. https://dermnetnz.org/topics/juvenile-xanthogranuloma
- The Budding Scavenger-Juvenile Xanthogranuloma — Juniper Publishers. 2023. https://juniperpublishers.com/oajs/OAJS.MS.ID.555846.php
- Juvenile xanthogranuloma – Knowledge and References — Taylor & Francis. 2023. https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Dermatology/Juvenile_xanthogranuloma/
Read full bio of medha deb