Mirizzi Syndrome: Types, Symptoms, Treatment
Understanding Mirizzi syndrome: causes, symptoms, diagnosis, and surgical treatment options.
Mirizzi Syndrome: Understanding a Rare Gallstone Complication
Mirizzi syndrome is a rare but serious complication of chronic gallstone disease that affects the biliary system’s ability to transport bile. It occurs when a large gallstone or cluster of stones becomes lodged in the gallbladder or cystic duct, causing significant swelling that can block the normal flow of bile from the liver to the small intestine. This condition represents an uncommon sequela of cholelithiasis, affecting approximately 2.5% of patients undergoing gallbladder removal surgery. Despite its rarity, Mirizzi syndrome requires prompt diagnosis and treatment to prevent serious complications including jaundice, inflammation, infection, and potentially life-threatening conditions such as sepsis and liver failure.
What is Mirizzi Syndrome?
Mirizzi syndrome develops when a gallstone or multiple gallstones obstruct a bile duct from the outside rather than from within the duct itself. Your gallbladder receives and stores bile produced by your liver and releases it into your small intestine through a network of branching passageways called ducts. In normal circumstances, bile flows freely through these ducts to aid in digestion. However, in Mirizzi syndrome, a duct becomes blocked from external pressure when a gallstone within your gallbladder or one of the other ducts becomes so enlarged that it presses on an adjacent duct, severely compromising bile flow.
The condition was originally caused by an impacted cystic duct stone leading to gallbladder distention and subsequent compression of the extrahepatic biliary tree. However, the original classification has been expanded to include hepatic duct stenosis caused by a stone at the junction of the cystic and hepatic ducts or as a result of cholecystitis, even in the absence of an obstructing cystic duct stone. Occasionally, the gallstone erodes into the common hepatic duct, producing a cholecystocholedochal fistula, which represents a more severe form of the condition.
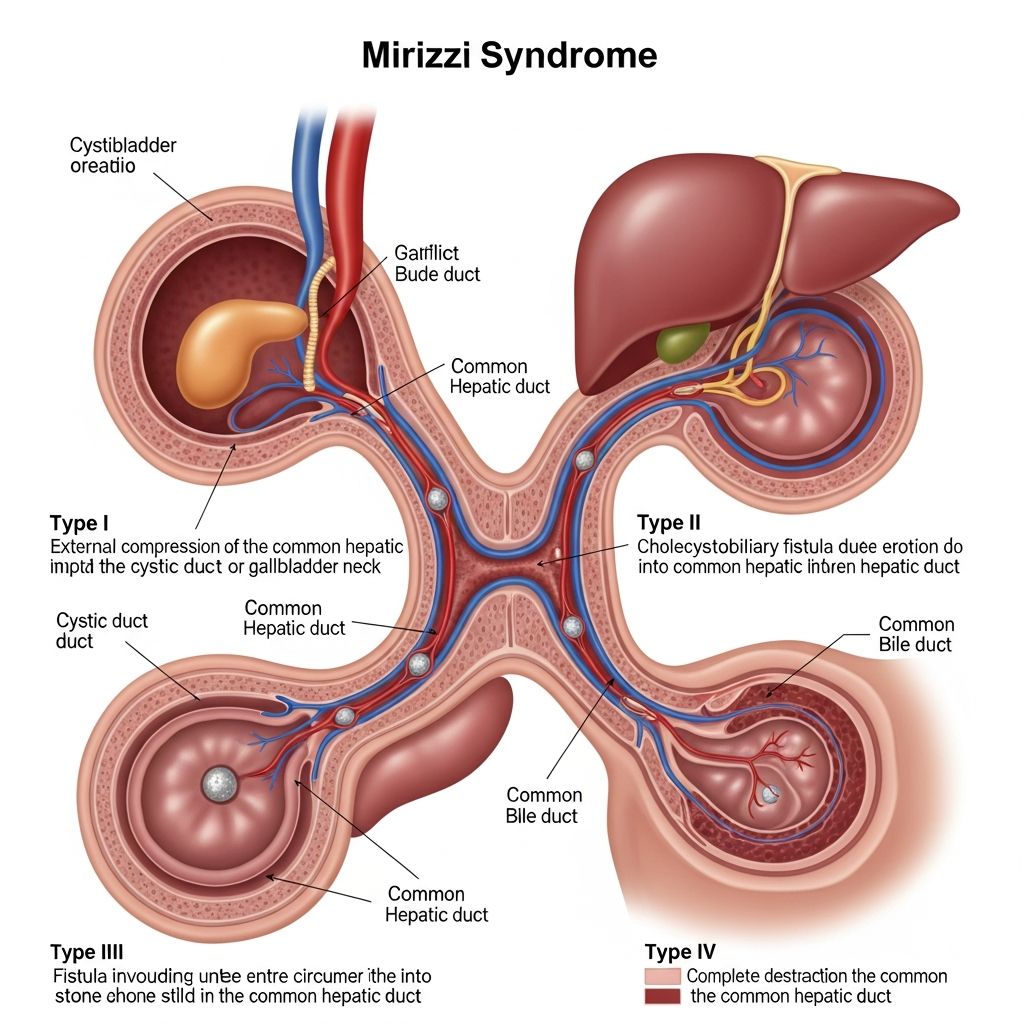
Classification of Mirizzi Syndrome
Healthcare providers classify Mirizzi syndrome into five distinct types based on the severity and characteristics of the condition. Understanding these classifications helps surgeons plan appropriate treatment strategies.
| Mirizzi Syndrome Type | Characteristics and Complications |
|---|---|
| Type I | One or more gallstones stuck in the gallbladder or cystic duct press on a nearby duct, blocking bile flow without any fistula formation |
| Type II | A fistula (hole) exists in the bile duct, with the opening measuring less than one-third of the bile duct’s circumference |
| Type III | A fistula is present with the opening measuring between one-third and two-thirds of the bile duct’s circumference |
| Type IV | A fistula exists with an opening measuring more than two-thirds of the bile duct’s circumference, often involving the hepatic duct |
| Type V | Involvement of the intrahepatic bile ducts in addition to the common bile duct or hepatic duct |
How Mirizzi Syndrome Develops
Mirizzi syndrome occurs through a specific pathophysiological process that distinguishes it from simple gallstone disease. A stuck gallstone or cluster of gallstones causes such significant swelling that it exerts pressure on your common bile duct—the tube that carries bile from your liver and gallbladder to your small intestine—or your common hepatic duct, which carries bile from your liver to your small intestine.
The gallbladder’s pouch, neck, and cystic duct are all relatively narrow structures where a gallstone could easily become trapped. Importantly, these anatomical structures lie very close beside each other, and the distance between them varies considerably from person to person. Some individuals have anatomical variations that make them more susceptible to developing Mirizzi syndrome when gallstones form. The chronic pressure exerted by an impacted stone eventually leads to inflammation, fibrosis, and potential erosion through the bile duct wall, particularly in more advanced cases.
Symptoms of Mirizzi Syndrome
Mirizzi syndrome symptoms fall into three main categories, each indicating different aspects of bile flow disruption and its systemic effects:
Biliary Symptoms
These symptoms relate directly to the obstruction of bile flow and include right upper quadrant abdominal pain, which may be severe and persistent. Patients often experience discomfort that worsens after eating fatty meals, similar to other biliary conditions. Nausea and vomiting are common accompaniments, along with loss of appetite that can lead to unintended weight loss.
Cholestatic Symptoms
Cholestasis, the slowing or stalling of bile flow through the biliary system, produces characteristic signs including jaundice, where the skin and whites of the eyes develop a yellowish tint due to elevated bilirubin levels. Patients frequently experience pruritus, or severe itching, which can be extremely bothersome. Pale or clay-colored stools occur because bile is not reaching the intestines to aid in digestion and color stool appropriately. Dark urine develops due to excess bilirubin being filtered by the kidneys.
Inflammatory and Infectious Symptoms
When inflammation or infection develops, patients may experience fever, chills and general malaise. These symptoms indicate acute cholecystitis or ascending cholangitis and require urgent medical attention. Left untreated, these infections can progress to sepsis, a life-threatening systemic inflammatory response.
Diagnosis of Mirizzi Syndrome
Because Mirizzi syndrome is rare and shares symptoms with other common conditions, surgeons often don’t diagnose it until they perform gallstone surgery. However, healthcare providers use several diagnostic approaches to identify the condition.
Physical Examination
Diagnosis begins with a physical exam where providers press on your belly to feel for signs of swelling. The physician will also carefully ask about your symptoms and medical history, paying particular attention to the duration and character of abdominal pain and whether you have experienced jaundice.
Laboratory Testing
If you have signs of infection or jaundice, your provider will run blood tests including liver function tests to assess bilirubin levels, alkaline phosphatase, aspartate transaminase (AST), and alanine transaminase (ALT). A complete blood count may reveal elevated white blood cells indicating infection. These laboratory abnormalities help confirm obstruction and inflammation but cannot definitively diagnose Mirizzi syndrome alone.
Imaging Studies
Several imaging modalities help visualize the biliary system and gallstones:
Ultrasound: Often the first imaging study performed, ultrasound can identify gallstones and assess gallbladder distention, though it may not clearly show the relationship between stones and ducts.
Magnetic Resonance Cholangiopancreatography (MRCP): This non-invasive imaging technique provides excellent visualization of the biliary tree and can demonstrate extrinsic compression of bile ducts by gallstones, making it invaluable for confirming Mirizzi syndrome diagnosis.
Computed Tomography (CT) Scan: CT imaging can show the relationship between gallstones, the gallbladder, and nearby ducts, helping determine the type and severity of Mirizzi syndrome.
Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure combines endoscopy with X-ray imaging and is both diagnostic and therapeutic, allowing visualization of the biliary obstruction and placement of stents if needed.
Complications Associated with Mirizzi Syndrome
Without prompt treatment, Mirizzi syndrome can lead to several serious complications. Bile duct injury may result from the chronic inflammation and stone erosion, potentially requiring complex surgical repair. Cholangitis, an infection of the bile ducts, can develop due to bile stasis and bacterial overgrowth. Acute pancreatitis may occur if the obstruction affects pancreatic duct drainage. The condition is associated with an increased risk of gallbladder cancer, though it is not necessarily a direct contributing cause. Most concerning is the potential for progression to sepsis, a life-threatening systemic infection, and hepatic dysfunction or liver failure from prolonged cholestasis.
Treatment of Mirizzi Syndrome
Surgery is the definitive treatment for Mirizzi syndrome, though there is no single standard procedure that applies to all cases. Instead, surgical management is tailored to the specific characteristics of each patient’s condition.
Surgical Approach
In most cases, Mirizzi syndrome management involves gallbladder removal (cholecystectomy) and repair of the blocked duct. In some cases, your surgeon may also need to remove blocked bile ducts or use stents to open them up. Your surgeon may employ a minimally invasive laparoscopic approach or perform open surgery (laparotomy) depending on the complexity of the case and intraoperative findings.
Surgical Challenges
Surgery for Mirizzi syndrome can be challenging because inflammation makes it difficult to see anatomical structures clearly. The chronic inflammatory process obscures normal tissue planes, increasing the risk of accidental injury to bile ducts during surgery. Such iatrogenic injuries can lead to additional complications including bile leaks, strictures, and the need for additional procedures. Surgeons must exercise careful dissection and may need to convert from laparoscopic to open surgery if complications arise.
Prognosis and Outcomes
Mirizzi syndrome is treatable, but the risk of serious complications increases the longer treatment is delayed. The mortality rate associated with Mirizzi syndrome ranges between 5% and 30%, with death potentially resulting from systemic infection (sepsis), liver failure, or associated gallbladder cancer. Early diagnosis and prompt surgical intervention significantly improve outcomes and reduce the risk of these life-threatening complications.
When to Seek Emergency Medical Care
Certain symptoms warrant immediate medical attention. Symptoms of sepsis, including fast heart rate, sweaty skin, and shortness of breath, represent a medical emergency. Severe abdominal pain accompanied by high fever and vomiting requires urgent evaluation. Persistent jaundice with darkening urine and progressive itching should prompt immediate medical assessment. If you develop these symptoms after gallbladder surgery, don’t wait—seek medical care right away, as post-cholecystectomy Mirizzi syndrome is a recognized complication requiring urgent intervention.
Frequently Asked Questions
Q: How common is Mirizzi syndrome?
A: Mirizzi syndrome is quite rare. Surgeons identify it in up to 2.5% of people having their gallbladder removed. Because of its rarity and similarity to other conditions, it is often diagnosed during surgery rather than beforehand.
Q: Can Mirizzi syndrome develop after gallbladder removal?
A: Yes, post-cholecystectomy Mirizzi syndrome can occur in patients who previously had their gallbladder removed. It is characterized by recurrent abdominal pain, jaundice, and fever and requires specialized diagnosis and treatment.
Q: Is Mirizzi syndrome related to gallbladder cancer?
A: Mirizzi syndrome is associated with an increased risk of gallbladder cancer, though it is not necessarily a contributing cause. Patients with Mirizzi syndrome should be monitored carefully for signs of malignancy.
Q: What is the difference between Type I and Type II Mirizzi syndrome?
A: Type I involves simple external compression of the bile duct by gallstones without any fistula formation. Type II involves a fistula (hole) in the bile duct measuring less than one-third of the duct’s circumference, representing a more severe form requiring different surgical management.
Q: Can Mirizzi syndrome be treated without surgery?
A: Surgery is the definitive treatment for Mirizzi syndrome. While endoscopic procedures such as stent placement may provide temporary relief, they do not address the underlying problem and are typically used as bridge therapy before definitive surgical intervention.
Q: What are the long-term outcomes after Mirizzi syndrome surgery?
A: Most patients experience good long-term outcomes after appropriate surgical treatment of Mirizzi syndrome. However, outcomes depend on the type and severity of the condition, the surgeon’s experience, and whether complications develop. Early diagnosis and treatment improve the likelihood of favorable outcomes.
References
- Mirizzi Syndrome: Types, Symptoms, Treatment & Prognosis — Cleveland Clinic. 2024-01-15. https://my.clevelandclinic.org/health/diseases/22092-mirizzi-syndrome
- Gallbladder and Biliary Tract Disease — Cleveland Clinic Department of Digestive Diseases. 2024-01-10. https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/gallbladder-biliary-tract-disease
- Post-cholecystectomy Mirizzi Syndrome — PubMed Central, National Center for Biotechnology Information. 2022-06-01. https://pubmed.ncbi.nlm.nih.gov/35611037/
- Bile Duct Obstruction: Symptoms, Causes & Treatment — Cleveland Clinic. 2024-01-12. https://my.clevelandclinic.org/health/diseases/bile-duct-obstruction
- Cholestasis: Definition, Symptoms, Treatment, Causes — Cleveland Clinic. 2024-01-08. https://my.clevelandclinic.org/health/diseases/24554-cholestasis
- Does incidentally detected common bile duct dilation need intervention? — Cleveland Clinic Journal of Medicine, Vol. 89, No. 6. 2022-06-01. https://www.ccjm.org/content/89/6/315
Read full bio of Sneha Tete











