Mohs Surgery: What to Expect
Comprehensive guide to Mohs surgery: preparation, step-by-step procedure, recovery tips, and why it's the gold standard for skin cancer treatment.

Mohs surgery, also known as Mohs micrographic surgery, is a highly effective, tissue-sparing procedure for treating skin cancer, particularly basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). It offers cure rates up to 99% for new cancers and 94% for recurrent ones by removing cancer layer by layer with immediate microscopic examination. This outpatient technique minimizes damage to healthy tissue, making it ideal for cosmetically sensitive areas like the face, ears, nose, eyelids, and genitals.
What Is Mohs Surgery?
Developed by Dr. Frederic Mohs in the 1930s, Mohs surgery combines surgical excision with real-time pathology analysis in an on-site lab. Unlike traditional excision where tissue is sent off-site for later review, Mohs allows the surgeon to examine 100% of the tumor margins during the procedure, ensuring complete cancer removal while preserving healthy skin. It’s the gold standard for high-risk skin cancers that are recurrent, aggressive, large, or in areas where tissue conservation is crucial.
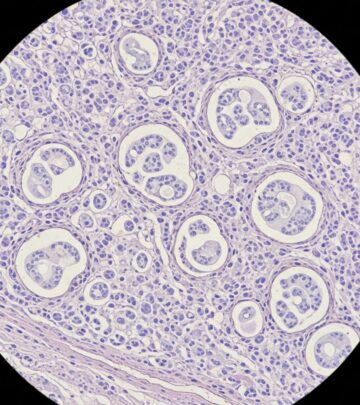
The procedure treats common non-melanoma skin cancers like BCC and SCC, and sometimes melanoma or other rare types when precision is needed. By mapping the exact location of cancer cells, surgeons target only affected areas, reducing recurrence risk and improving cosmetic outcomes.
Why Choose Mohs Surgery?
Mohs stands out for its precision and efficacy. Key benefits include:
- Highest cure rates: Up to 99% for primary BCC and 94-98% for recurrent cases, surpassing standard excision.
- Tissue preservation: Removes only cancerous tissue, minimizing scars especially on the face and functional areas.
- Real-time results: Immediate lab analysis confirms clear margins before closing the wound.
- Outpatient convenience: Done under local anesthesia in one visit, typically 2-6 hours.
- Lower recurrence: Examines 100% of margins, ideal for ill-defined or aggressive tumors.
It’s recommended for cancers with high recurrence risk, unclear borders, or in preservation-priority sites like eyes, nose, mouth, hands, feet, or genitals.
Preparing for Mohs Surgery
Preparation ensures a smooth experience. Start by:
- Consult your surgeon: Discuss medical history, medications (e.g., blood thinners), allergies, and skin care routine.
- Medication review: Stop aspirin, ibuprofen, or supplements like vitamin E 7-10 days prior if advised; continue prescribed blood thinners unless instructed otherwise.
- Day before: Wash surgical site with mild soap, avoid lotions, makeup, or shaving. Arrange transportation and a companion.
- Eat and hydrate: Have a light breakfast; local anesthesia allows normal intake.
- What to bring: ID, insurance, comfortable loose clothing, snacks, book, or entertainment for wait times.
Avoid alcohol, smoking, and sun exposure pre-op to promote healing. Confirm arrival time, as surgery may last several hours.
The Day of Mohs Surgery: Step-by-Step
Mohs is staged, with each cycle of removal, mapping, and analysis repeating until clear. Expect 2-6 hours total.
Step 1: Arrival and Anesthesia
Check-in, change into a gown, and receive local anesthesia via injection to numb the area. You’ll stay awake but comfortable; sedation is rare.
Step 2: First Layer Removal
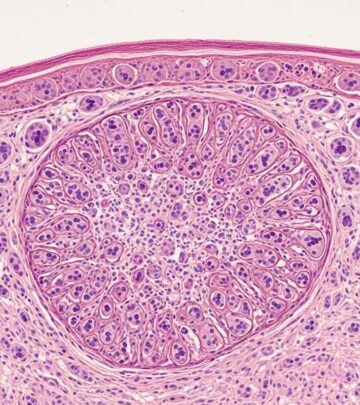
The surgeon excises the visible tumor plus a thin margin using a scalpel at a 45-degree bevel for processing. The wound is bandaged; you relax in a waiting area.
Step 3: Lab Processing and Mapping
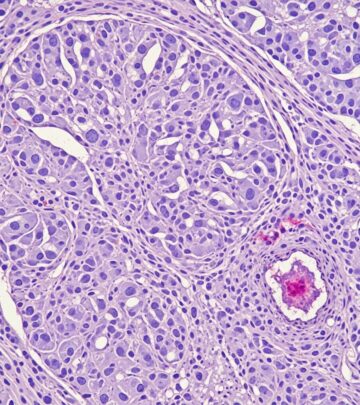
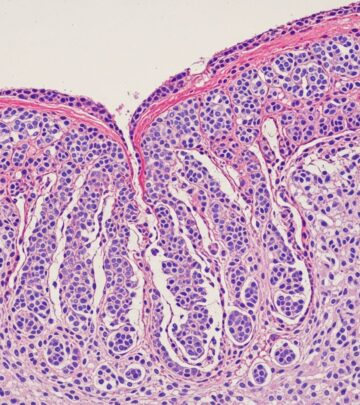
Tissue is sectioned, frozen, stained, and mapped. The surgeon microscopically checks 100% of edges and deep margins for cancer cells, noting exact locations if positive.
Step 4: Repeat if Needed
Additional layers are removed only from positive areas. Cycles repeat (average 2-3) until margins are clear. You’ll be informed each time.
| Stage | Description | Duration |
|---|---|---|
| 1st Layer | Visible tumor + margin excised | 15-30 min |
| Lab Exam | Microscopic review & mapping | 30-60 min |
| Subsequent Layers | Targeted removal if cancer found | Repeat as needed |
| Wound Repair | Closure once clear | 30-90 min |
Wound Repair After Clear Margins
Once cancer-free, the surgeon repairs the wound using:
- Primary closure: Stitches for small defects.
- Flaps or grafts: For larger areas to optimize healing and appearance.
- Healing by secondary intention: Natural granulation for some sites.
- Referral: To specialists for complex reconstructions.
Repair choice depends on size, location, and your health.
Post-Operative Care and Recovery
Recovery varies by wound size; most resume normal activities in days.
- Immediate aftercare: Keep bandage dry 24-48 hours; elevate head while sleeping.
- Wound care: Clean daily with saline/hydrogen peroxide, apply antibiotic ointment and new dressing.
- Pain management: Tylenol; ice first 48 hours. Avoid aspirin.
- Activity restrictions: No strenuous exercise, heavy lifting, or bending for 1-2 weeks; protect from sun.
- Healing timeline: Stitches out 5-14 days; full healing 4-6 weeks. Scars fade over months.
Watch for infection (redness, pus, fever) or bleeding; contact your doctor. Long-term: Daily SPF 30+, hats, skin checks.
Risks and Complications
Mohs is safe with low risks:
- Common: Bleeding, bruising, swelling, temporary numbness.
- Rare: Infection (1-2%), poor healing, nerve damage, recurrence (<5%).
- Allergic reactions: To anesthesia or dressings.
Discuss with your surgeon; outcomes are excellent for most.
Frequently Asked Questions (FAQs)
Is Mohs surgery painful?
The numbed area feels pressure but no pain during removal. Post-op discomfort is mild, managed with OTC pain relievers.
How long does Mohs surgery take?
2-6 hours, depending on stages needed. Plan for a full morning or afternoon.
Will I have a scar?
Yes, but smaller and better placed than alternatives due to tissue sparing. Skilled repair minimizes visibility.
Can I drive home after?
Yes, local anesthesia doesn’t impair driving, but bring a companion for support.
Is Mohs covered by insurance?
Often yes for medically indicated cases; confirm with your provider.
Long-Term Skin Cancer Prevention
Post-Mohs, prevent recurrence with:
- Sunscreen SPF 30+ daily, reapply every 2 hours.
- Protective clothing, hats, sunglasses.
- Avoid peak sun (10 AM-4 PM); seek shade.
- Monthly self-exams; annual dermatologist visits.
- Avoid tanning beds.
Early detection saves lives; Mohs empowers confidence in treatment.
References
- Mohs Surgery Explained: A Seattle Patient’s Guide — Dermatology Seattle. 2023. https://dermatologyseattle.com/mohs-surgery-skin-cancer-guide/
- Mohs Surgery: Procedure, Risks, Recovery — Cleveland Clinic. 2024-01-15. https://my.clevelandclinic.org/health/treatments/13312-mohs-surgery
- Mohs Surgery — Skin Cancer Foundation. 2024. https://www.skincancer.org/treatment-resources/mohs-surgery/
- Mohs Surgery for Skin Cancer: Benefits, Process & What to Expect — Clarus Dermatology. 2023-06-12. https://clarusdermatology.com/mohs-surgery-explained/
- Mohs Surgery — Mayo Clinic. 2024-05-20. https://www.mayoclinic.org/tests-procedures/mohs-surgery/about/pac-20385222
- Mohs Surgery for Melanoma — Melanoma Research Foundation. 2023. https://www.curemelanoma.org/patient-eng/melanoma-treatment/options/mohs-surgery
- Mohs Micrographic Surgery — NCBI StatPearls. 2024-07-01. https://www.ncbi.nlm.nih.gov/books/NBK441833/
Read full bio of medha deb