Mood Swings: 6 Expert Tips To Manage Emotional Instability
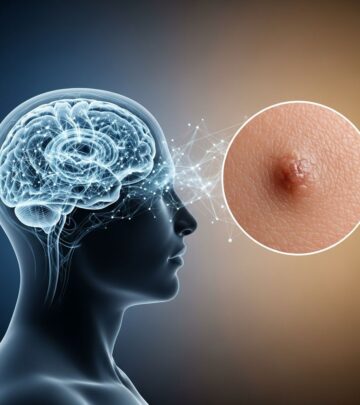
Understand the causes, symptoms, and treatments for mood swings to regain emotional balance and improve daily life.

Mood Swings
Mood swings are sudden, intense changes in emotional state that can disrupt daily life, ranging from euphoria to irritability or sadness. These shifts, often lasting minutes to days, affect 13.9% of the general population, with higher rates in women and young adults aged 16–24.
While occasional fluctuations are normal, frequent or extreme mood swings signal underlying issues like hormonal imbalances, stress, or psychiatric conditions. This article covers definitions, causes, symptoms, diagnosis, treatments, and prevention, drawing from clinical research to provide actionable insights.
What Are Mood Swings?
Mood swings, also termed
mood instability
oraffective lability
, involve rapid oscillations of intense affect with difficulty regulating these changes or their behavioral impacts. Unlike stable moods that adapt gradually to circumstances, mood swings feature abrupt valence shifts—positive to negative or vice versa—often without clear triggers.Key characteristics include:
- Frequency: Multiple shifts daily or weekly.
- Intensity: Extreme highs (euphoria, agitation) and lows (despair, anger).
- Rapidity: Quick onset and resolution, sometimes within hours.
- Reactivity: Triggered by minor events or occurring spontaneously.
Prevalence data from the Adult Psychiatric Morbidity Survey (APMS 2007, n=7403) shows 13.9% population rate, declining with age to 7% in those 65–74. It’s reported in 40–60% of individuals with depression, anxiety, PTSD, or OCD, linking to higher service use and suicidality independent of other factors.
Symptoms of Mood Swings
Recognizing symptoms is crucial for early intervention. Common signs include:
- Sudden tearfulness or outbursts disproportionate to events.
- Irritability flipping to laughter or apathy.
- Energy surges followed by crashes, impacting sleep and appetite.
- Difficulty concentrating or making decisions amid flux.
- Relationship strains from unpredictable reactions.
In severe cases, mood swings precede or accompany disorders like bipolar, where chronic instability exceeds discrete episodes. Physical cues like tension headaches or fatigue often accompany emotional turbulence.
Causes of Mood Swings
Mood swings stem from multifaceted origins, blending biological, psychological, and environmental factors. Understanding triggers enables targeted management.
Hormonal Changes
Fluctuating hormones drive many swings, especially in women. Premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) cause irritability and sadness pre-period due to estrogen/progesterone drops. Perimenopause elevates risks via similar imbalances. Thyroid disorders (hypo/hyperthyroidism) disrupt serotonin, mimicking swings; blood tests confirm this.
Mental Health Disorders
Psychiatric conditions feature prominently:
- Bipolar Disorder: hallmark manic-depressive cycles; prodromal instability predicts onset.
- Borderline Personality Disorder (BPD): intense, short-lived swings tied to abandonment fears.
- Depression/Anxiety: 40-60% comorbidity; rumination amplifies shifts.
- ADHD: impulsivity links to emotional dysregulation.
Mood instability mediates trauma to BPD or psychosis pathways.
Stress and Lifestyle Factors
Chronic stress elevates cortisol, destabilizing mood via HPA axis dysregulation. Sleep deprivation (<7 hours/night) impairs prefrontal regulation, worsening swings. Poor diet (high sugar/caffeine), lack of exercise, and substance use (alcohol, drugs) exacerbate volatility by altering neurotransmitters.
Medical Conditions and Medications
Conditions like diabetes, anemia, or neurological issues (e.g., multiple sclerosis) indirectly cause swings via fatigue or pain. Medications—steroids, antidepressants, birth control—can induce them as side effects; consult providers for adjustments.
When to See a Doctor for Mood Swings
Seek professional help if swings:
- Interfere with work, relationships, or self-care.
- Include suicidal thoughts, self-harm, or mania (racing thoughts, risky behavior).
- Persist >2 weeks or intensify suddenly.
- Accompany physical symptoms like unexplained weight changes.
Early intervention prevents escalation; mood instability predicts poorer bipolar outcomes if untreated.
How Are Mood Swings Diagnosed?
No single test exists; diagnosis involves:
- Clinical Interview: History of swings, triggers, family mental health.
- Questionnaires: Scales like Affective Lability Scale or single-item APMS questions assess instability.
- Physical Exams/Labs: Rule out thyroid, vitamin deficiencies, hormones.
- Mood Tracking: Apps or diaries capture real-time patterns; high-frequency monitoring reveals chronicity beyond episodes.
Differential diagnosis distinguishes from cyclothymia, PMDD, or substance effects.
Mood Swing Treatments and Management
Treatment targets root causes with multimodal approaches.
Therapy
Cognitive Behavioral Therapy (CBT) reframes negative patterns; Dialectical Behavior Therapy (DBT) builds emotion regulation, ideal for BPD-linked swings. Mindfulness-Based Cognitive Therapy (MBCT) reduces relapse in mood disorders.
Medications
Antidepressants (SSRIs) stabilize serotonin for depression/anxiety-driven swings. Mood stabilizers (lithium, valproate) manage bipolar. Hormone therapy addresses PMDD/thyroid issues. Always pair with therapy; monitor side effects.
Lifestyle Changes
| Strategy | Benefits | Implementation |
|---|---|---|
| Regular Exercise | Boosts endorphins, reduces cortisol | 30 min/day aerobic activity |
| Sleep Hygiene | Stabilizes circadian rhythms | 7-9 hours/night, consistent schedule |
| Balanced Diet | Supports neurotransmitter balance | Omega-3s, whole grains, limit sugar |
| Stress Management | Lowers reactivity | Meditation, yoga 10-20 min/day |
Alternative Approaches
Supplements like omega-3s or magnesium show promise (consult MD). Acupuncture or yoga aid some via relaxation response.
How to Prevent Mood Swings
Proactive steps minimize episodes:
- Track moods daily to identify patterns/triggers.
- Maintain routines for sleep, meals, exercise.
- Build support networks; limit alcohol/caffeine.
- Practice grounding techniques: deep breathing, progressive muscle relaxation.
- Address stressors via journaling or therapy.
Longitudinal studies emphasize early mood instability tracking from childhood to avert disorder progression.
Complications of Untreated Mood Swings
Chronic instability raises risks: suicidality, substance abuse, relationship breakdowns, occupational impairment. In bipolar, it forecasts relapse; transdiagnostically, it amplifies psychopathology.
Frequently Asked Questions (FAQs)
What triggers mood swings?
Common triggers: hormonal shifts, stress, sleep loss, medications, mental health conditions like bipolar or BPD.
Are mood swings a sign of bipolar?
They can be prodromal; bipolar features episodic extremes, but instability often precedes diagnosis.
Can diet affect mood swings?
Yes; blood sugar spikes from sugars worsen volatility, while stable nutrition supports serotonin.
How long do mood swings last?
Minutes to days; duration varies by cause—hormonal (days), stress (hours).
Do mood swings improve with age?
Often yes; prevalence drops post-24, per APMS data.
(Word count: 1672)
References
- Mood instability: significance, definition and measurement — PMC – NIH. 2015-09-14. https://pmc.ncbi.nlm.nih.gov/articles/PMC4589661/
- Mood Disorders Overview — National Institute of Mental Health (NIMH). 2023-07-05. https://www.nimh.nih.gov/health/topics/mood-disorders
- Bipolar Disorder — World Health Organization (WHO). 2024-02-20. https://www.who.int/news-room/fact-sheets/detail/bipolar-disorder
- Premenstrual Dysphoric Disorder — American Psychiatric Association. 2022-03-18. https://www.psychiatry.org/patients-families/pmdd/what-is-premenstrual-dysphoric-disorder
- Emotional Dysregulation in ADHD — Centers for Disease Control and Prevention (CDC). 2024-11-15. https://www.cdc.gov/adhd/signs-symptoms/index.html
Read full bio of medha deb