Non-Dermatophyte Mould Onychomycosis
Understanding the causes, diagnosis, and management of opportunistic mould nail infections worldwide.

Author: Dr. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Reviewed and copy-edited by Richa Tripathi, Consultant Dermatologist, Grande International Hospital, Kathmandu, Nepal. November 2021. Updated with recent evidence as of 2026.
Introduction
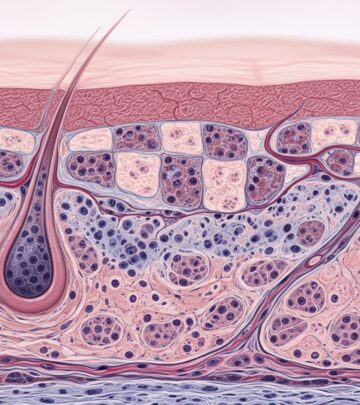
Non-dermatophyte mould onychomycosis (NDMO), also known as non-dermatophyte mould (NDM) nail infection, represents an opportunistic fungal invasion of the nail plate and surrounding tissues by various environmental mould species. Unlike dermatophyte fungi, which are primary nail pathogens, NDMs are ubiquitous contaminants that rarely invade healthy nails without predisposing factors. These infections constitute approximately 10% of all onychomycosis cases globally, with rising prevalence noted in recent years, particularly in tropical regions and cases with co-existing dermatophyte infections.
Moulds thrive in soil, decaying vegetation, and damp environments, gaining entry through microtrauma or damaged nail barriers. Most NDMs are non-keratolytic, meaning they do not digest keratin effectively, except for species like Neoscytalidium dimidiatum, which exhibits stronger invasiveness. NDMO predominantly affects toenails (25 times more common than fingernails) and often involves a single nail, distinguishing it from multifocal dermatophyte infections.
Demographics
NDMO shows no strong age or gender predilection but is more prevalent in warmer climates where mould proliferation is favored. Reports indicate increasing incidence in immunocompromised populations, diabetics, and those with peripheral vascular disease. Global surveys highlight higher rates in Asia (e.g., India, Nepal) and Latin America, where species like Aspergillus and Fusarium dominate. Elderly patients and those with occupational exposure to soil or water (farmers, gardeners) are at elevated risk.
Causes
NDMs cause onychomycosis when environmental spores penetrate compromised nails. Key risk factors mirror those of general onychomycosis but emphasize trauma and humidity:
- Trauma or dystrophy from prior nail disease (e.g., psoriasis, onycholysis)
- Hyperhidrosis and occlusive footwear promoting moisture
- Immunosuppression (HIV, diabetes, chemotherapy)
- Peripheral artery disease or poor circulation
- Age-related nail changes
- Tinea pedis or co-infections
- Occupational exposure to mouldy environments
Geographical variation influences causative species. Common pathogens include:
- Aspergillus spp. (e.g., A. niger, A. flavus) – 20-30% of cases
- Fusarium spp. – Frequent in toenails
- Scopulariopsis brevicaulis – Brittle, powdery nails
- Neoscytalidium spp. – Keratolytic, black discoloration
- Acremonium and Paecilomyces – Rare but aggressive
Clinical features
NDMO manifests in patterns akin to dermatophyte onychomycosis but with distinctive features:
- Distal lateral subungual onychomycosis (DLSO): Most common; yellow-white discoloration, onycholysis, hyperkeratosis.
- Superficial white onychomycosis (SWO): Powdery white patches on nail surface.
- Proximal subungual onychomycosis (PSO): Rare, indicates severe immunocompromise.
- Total dystrophic onychomycosis (TDO): Advanced crumbling of entire nail
Paronychia is frequent, with erythema, swelling, and granulation tissue. Nail color varies: black (A. niger), green (Pseudomonas co-infection), white powdery (Scopulariopsis). Painless dystrophy progresses to thickening and brittleness.
Complications
Untreated NDMO leads to permanent nail destruction, secondary bacterial infections, and pain limiting mobility. In diabetics, it increases ulceration and osteomyelitis risk. Aesthetic impact causes psychosocial distress. Relapses are common (up to 50%), especially with incomplete eradication.
Diagnosis
Diagnosis is challenging due to contamination risks; moulds in culture may not indicate true infection. Confirmed by ≥3 criteria:
- Positive direct microscopy (KOH/whitfield prep showing fungal hyphae)
- Non-dermatophyte mould in ≥2 repeated cultures
- No dermatophytes or Candida in culture
- Clinical features consistent with NDMO (e.g., single nail, paronychia)
- Mould observed in histological sections (PAS stain)
Advanced tools include PCR for species identification (sensitivity >90%) and immunofluorescence. Combining PAS staining with culture boosts detection to 96%. Differential diagnoses: psoriasis, trauma, bacterial infections, lichen planus.
Differential diagnosis
| Condition | Key Features | Differentiator |
|---|---|---|
| Traumatic onycholysis | No discoloration, no hyphae | Negative microscopy |
| Psoriatic nails | Onycholysis + pitting | Systemic signs, biopsy |
| Bacterial paronychia | Green pus, acute pain | Gram stain positive |
| Dermatophyte onychomycosis | Multinail, yellow spikes | Positive dermatophyte culture |
Treatment
NDMO is harder to treat than dermatophyte infections, often requiring combined oral + topical therapy for 12-18 months. Systemic antifungals are effective for Aspergillus, Scopulariopsis, Fusarium.
Oral antifungals
- Terbinafine: 250 mg/day; first-line, but variable response (mycotic cure 50-70%)
- Itraconazole: Pulse (200 mg BID x1 wk/mo) or continuous; effective for Candida co-infections
- Fluconazole: 150-300 mg/week; for Candida/NDM
Monitor LFTs; duration longer than dermatophytes.
Topical therapies
- Ciclopirox 8% lacquer: Daily; adjunct, improves cure with orals (88% mycotic cure combined)
- Amorolfine 5% weekly
- Bifonazole/urea for debridement
Physical treatments
Nail debridement enhances penetration (77% mycotic cure with ciclopirox). Lasers (Nd:YAG) offer temporary clearance (FDA-approved for cosmetic improvement), not curative.
| Agent | Regimen | Mycotic Cure (%) |
|---|---|---|
| Terbinafine + Ciclopirox | Oral daily + lacquer | 88 |
| Vicks Vaporub | Daily topical | 28 |
| Tea tree oil | BID | Variable, limited evidence |
Outcome
Cure rates: 40-70% mycotic, lower complete cures due to relapses (higher in NDMO). Predictors of failure: immunosuppression, Fusarium, poor adherence. Prevention: foot hygiene, trauma avoidance, prompt treatment of tinea pedis.
Frequently asked questions
Q: Can NDMO affect fingernails?
A: Yes, but toenails are affected 25x more often, usually singly with paronychia.
Q: Is laser treatment curative?
A: No, FDA-approved for temporary clear nail; combine with meds for better results.
Q: How long does treatment last?
A: 12-18 months; longer than dermatophytes due to poor penetration.
Q: Does diabetes increase risk?
A: Yes, via poor circulation and immunity; monitor closely.
Q: Can it spread to others?
A: Rare; not highly contagious like tinea, but share no nail tools.
References
- Treatment of nondermatophyte mold and Candida onychomycosis — Tosti A et al. Dermatol Clin. 2003-07-01. https://pubmed.ncbi.nlm.nih.gov/12956201/
- Non-dermatophyte mould onychomycosis — DermNet NZ. 2021-11. https://dermnetnz.org/topics/non-dermatophyte-mould-onychomycosis
- Onychomycosis: Current Trends in Diagnosis and Treatment — AAFP. 2013-12-01. https://www.aafp.org/pubs/afp/issues/2013/1201/p762.html/
- Toenail Fungus (Onychomycosis) — Cleveland Clinic. Recent update. https://my.clevelandclinic.org/health/diseases/11303-toenail-fungus
Read full bio of Sneha Tete