Penile Cancer: Symptoms, Causes & Treatment
Understand penile cancer: Learn about symptoms, causes, diagnosis, and effective treatment options available.
Penile Cancer: Understanding This Rare Urologic Malignancy
Penile cancer is a rare malignancy that develops when healthy cells in the penis change and grow out of control. While it accounts for less than 1% of cancers in men, understanding this condition is crucial for early detection and optimal treatment outcomes. When caught early, penile cancer can be highly curable, making awareness and prompt medical attention essential. Treatment approaches vary based on tumor characteristics and may involve surgery, chemotherapy, radiation therapy, or a combination of these modalities.
What Is Penile Cancer?
Penile cancer occurs when malignant cells develop in the tissues of the penis. The majority of penile cancers—approximately 95%—are squamous cell carcinomas, which begin in the thin, flat cells that cover the surface of the penis. This type originates in the skin cells and can vary in aggressiveness depending on its grade and stage at diagnosis. Other less common types of penile cancer include melanoma, basal cell carcinoma, and adenocarcinoma, though these represent a smaller percentage of cases.
Understanding the nature of penile cancer helps patients and their families grasp why certain treatment approaches are recommended and what to expect during their cancer journey. The disease’s rarity means that seeking care from specialists experienced in urologic oncology is particularly important for receiving the best possible outcomes.
Risk Factors and Causes of Penile Cancer
Several factors can increase a man’s risk of developing penile cancer. These risk factors include:
- Phimosis (tightness of the foreskin preventing retraction)
- Poor genital hygiene
- Smoking and tobacco use
- Human papillomavirus (HPV) infection
- Age over 50
- History of sexually transmitted infections
- Penile inflammatory conditions
- Balanitis (inflammation of the glans)
While these risk factors increase susceptibility, not all men with these factors will develop penile cancer. Some individuals may have no identifiable risk factors yet still develop the disease. Understanding these factors can help men take preventive measures and remain vigilant about changes in their genital health.
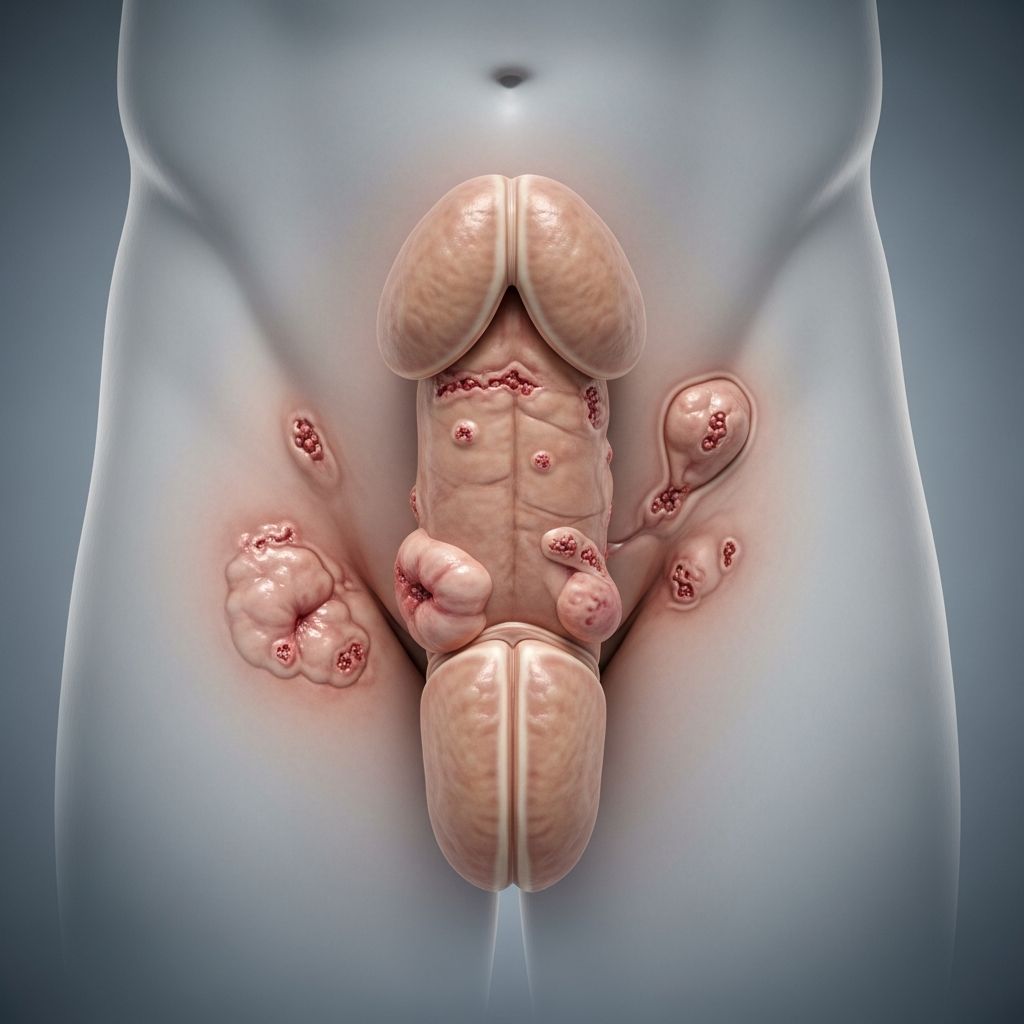
Recognizing Penile Cancer Symptoms
Being aware of potential warning signs is critical for early detection. Common symptoms of penile cancer include:
- A lump or mass on the penis
- Changes in skin color or appearance
- Unusual discharge from the penis
- Pain or tenderness in the affected area
- Bleeding or blood in urine
- Sores or ulcers on the penis
- Thickening or scaling of the skin
- Swelling of the penis or groin area
If you notice any of these changes, it’s important not to ignore them. While many penile conditions are benign, any unusual changes warrant prompt evaluation by a healthcare provider. Early detection significantly improves treatment outcomes and the likelihood of preserving penile function.
Diagnosis of Penile Cancer
Accurate diagnosis is essential for determining the appropriate treatment plan. The diagnostic process typically involves several steps and may include various tests and procedures.
Initial Consultation and Physical Examination
The diagnostic journey begins with a comprehensive consultation where your healthcare provider will review your medical history and discuss any symptoms you’ve experienced. During the physical examination, the doctor will carefully inspect the penis for abnormal growths, lumps, changes in skin appearance, or other concerning features. This initial evaluation helps identify areas that require further investigation.
Biopsy Confirmation
A biopsy is the only definitive way to confirm penile cancer diagnosis. During this procedure, your healthcare provider removes a small tissue sample from the suspicious area. The biopsy may be performed in an office setting or in an operating room under anesthesia, depending on the size and location of the lesion. The tissue sample is then examined under a microscope by a pathologist to determine if cancer cells are present.
Imaging Studies
Once biopsy confirms penile cancer, imaging tests help determine the cancer’s extent and whether it has spread. These imaging modalities include:
- CT (Computed Tomography) scans—providing detailed cross-sectional images
- MRI (Magnetic Resonance Imaging)—offering detailed soft tissue visualization
- Ultrasound—using sound waves to visualize internal structures
- Chest imaging—to check for distant spread
These tests help determine how far the cancer has spread within the penis, to lymph nodes, or to other parts of the body, which is crucial for staging and treatment planning.
Pathology Reports and Staging
Following the biopsy and imaging tests, a detailed pathology report will specify the cancer type, grade (aggressiveness), and stage (extent). Penile cancer staging typically uses the TNM classification system, which considers:
- T (Tumor): The size and depth of the primary tumor
- N (Nodes): Whether cancer has spread to nearby lymph nodes
- M (Metastasis): Whether cancer has spread to distant organs
Based on TNM classifications, penile cancer is assigned a stage from 0 (least advanced) to IV (most advanced). Lower-stage cancers are generally confined to the penis, while higher-stage cancers may have spread to lymph nodes or distant organs.
Treatment Options for Penile Cancer
Treatment planning for penile cancer depends on multiple factors including tumor size, depth of invasion, whether it has spread, grade, stage, patient age, overall health status, and individual treatment goals. A multidisciplinary team typically collaborates to develop a personalized treatment plan that may include your primary care physician, oncologist, urologist, radiation oncologist, and dermatologist.
Surgical Treatment
Surgery is typically the primary treatment for penile cancer. Cleveland Clinic surgeons are experts in minimally invasive surgical techniques that aim to preserve penile function when possible. Surgical options include:
- Wide Local Excision: Removes the tumor and surrounding normal tissue margins
- Laser Therapy: Uses focused light beams to destroy cancer cells
- Mohs Micrographic Surgery: Removes tissue layer by layer, examining each under a microscope
- Partial Penectomy: Removes part of the penis while preserving function
- Total Penectomy: Removes the entire penis when necessary
- Inguinal Lymph Node Dissection: Removes lymph nodes in the groin to check for cancer spread
When lymph nodes show evidence of cancer spread, lymph node dissection becomes part of the treatment plan. Advanced surgical techniques allow surgeons to remove affected lymph nodes while minimizing complications and preserving function.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It may be used alone or in combination with other treatments. Radiation approaches for penile cancer include:
- External Beam Radiation Therapy (EBRT): Delivers radiation from outside the body
- Brachytherapy: Places radioactive material directly into or near the cancer
- Intensity-Modulated Radiation Therapy (IMRT): Precisely targets tumors while sparing healthy tissue
- Image-Guided Radiation Therapy (IGRT): Uses imaging to guide radiation delivery
Radiation therapy may be recommended for patients with advanced disease, those unable to undergo surgery, or as adjuvant therapy following surgery to reduce recurrence risk.
Chemotherapy
Systemic chemotherapy uses anti-cancer drugs that circulate throughout the body to target cancer cells. Chemotherapy may be used for advanced penile cancer, either as neoadjuvant therapy (before surgery) to shrink tumors or as palliative care for advanced disease. Combination chemotherapy regimens are often more effective than single-agent therapy.
Multimodal Therapy
For advanced penile cancer, combining treatment modalities often provides better outcomes. Chemoradiation therapy combines chemotherapy with radiation to enhance treatment effectiveness. This approach may be followed by surgical consolidation if the cancer responds well.
Penectomy: Surgical Considerations
For patients requiring penectomy, understanding this procedure is important. Before surgery, comprehensive testing determines cancer type and stage to decide between partial or total penectomy. Healthcare providers also assess general health status through vital signs measurement and overall fitness for surgery.
Partial penectomy preserves portions of penile tissue and function when oncologically appropriate. Total penectomy becomes necessary when cancer extensively involves the penis or has invaded deeper structures. Reconstructive techniques and rehabilitation support help patients maintain urinary and sexual function when possible.
Prognosis and Survival Outcomes
Penile cancer has excellent outcomes when found and treated early. Prognosis depends on multiple factors including cancer stage, grade, patient age, and overall health status. Early-stage cancers confined to the penis have significantly better survival rates than advanced cancers with lymph node involvement or distant metastases.
Regular follow-up care after treatment is essential to monitor for recurrence. Your healthcare team will schedule periodic examinations and imaging studies as appropriate for your specific situation.
Quality of Life and Supportive Care
Managing penile cancer involves more than just medical treatment—quality of life considerations are paramount. Healthcare providers work to minimize treatment side effects and help preserve normal urinary and sexual function. Fertility preservation options, such as sperm banking, may be discussed before treatment begins.
Virtual follow-up visits offer convenient access to care from home, reducing travel burden during recovery. Comprehensive support addresses both physical healing and emotional well-being throughout the cancer journey. Counseling, support groups, and resources help patients and families cope with the psychological impact of diagnosis and treatment.
When to Seek Medical Attention
If you notice any changes in your penis—such as lumps, unusual skin color, pain, or discharge—don’t ignore these warning signs. Schedule an appointment with your healthcare provider promptly. Your doctor can evaluate the concern and determine whether further testing is needed. Early evaluation of suspicious changes dramatically improves the likelihood of early detection and successful treatment.
Key Takeaways
- Penile cancer is rare but highly treatable when detected early
- Approximately 95% of cases are squamous cell carcinomas
- Risk factors include poor hygiene, phimosis, smoking, and HPV infection
- Symptoms include lumps, skin changes, pain, and unusual discharge
- Diagnosis requires biopsy confirmation and imaging studies
- Treatment options include surgery, radiation, and chemotherapy
- Multidisciplinary care teams optimize outcomes and quality of life
- Early detection significantly improves prognosis and survival rates
Frequently Asked Questions
Q: How common is penile cancer?
A: Penile cancer is rare, accounting for less than 1% of cancers in men. However, early detection and treatment lead to excellent outcomes.
Q: What are the first signs of penile cancer I should watch for?
A: Watch for lumps or masses on the penis, changes in skin color or appearance, unusual discharge, pain, bleeding, sores, or swelling. Any persistent changes warrant medical evaluation.
Q: Is a biopsy necessary to diagnose penile cancer?
A: Yes, a biopsy is the only definitive way to confirm penile cancer diagnosis. It involves removing tissue for microscopic examination.
Q: Can penile cancer be cured?
A: Yes, penile cancer can be cured, especially when caught early. Treatment success depends on cancer stage, grade, and how quickly treatment begins.
Q: Will I lose my penis if diagnosed with penile cancer?
A: Not necessarily. Modern surgical techniques often allow partial penectomy that preserves penile function. Total penectomy is reserved for advanced cases.
Q: What is the recovery time after penile cancer surgery?
A: Recovery varies depending on the procedure performed. Most patients go home the same day for biopsies, while surgical procedures may require longer recovery periods. Your surgical team will provide specific recovery guidance.
Q: Can I preserve fertility if I have penile cancer?
A: Yes, fertility preservation options such as sperm banking may be available before treatment begins. Discuss this with your healthcare team.
Q: What should I do if I notice changes in my penis?
A: Schedule an appointment with your healthcare provider immediately. Early evaluation of any suspicious changes is critical for diagnosis and treatment.
References
- Urologic Cancer: Prostate, Bladder, Kidney and Testicular Treatment — Cleveland Clinic. 2025. https://my.clevelandclinic.org/departments/cancer/depts/urologic
- Penile Cancer: What Every Man Should Know — Urology Clinic PC. 2024. https://www.urologyclinicpc.com/patient-education/penile-cancer-what-every-man-should-know/
- Get Penile Cancer Treatment — Cleveland Clinic. 2025. https://my.clevelandclinic.org/services/penile-cancer-treatment
- Penectomy: Purpose, Procedure, Results & Recovery — Cleveland Clinic. 2025. https://my.clevelandclinic.org/health/treatments/22806-penectomy
- Penile Cancer Treatment Guidelines — National Comprehensive Cancer Network. 2024. https://www2.tri-kobe.org/nccn/guideline/urological/english/penile.pdf
- Penile Cancer Treatment (PDQ®) — National Institutes of Health, National Cancer Institute. 2024. https://www.ncbi.nlm.nih.gov/books/NBK65943/
Read full bio of medha deb











