Pericardial Window: Treatment for Fluid Around the Heart
Learn about pericardial window surgery, a minimally invasive procedure to drain excess fluid from around the heart.
Understanding the Pericardial Window Procedure
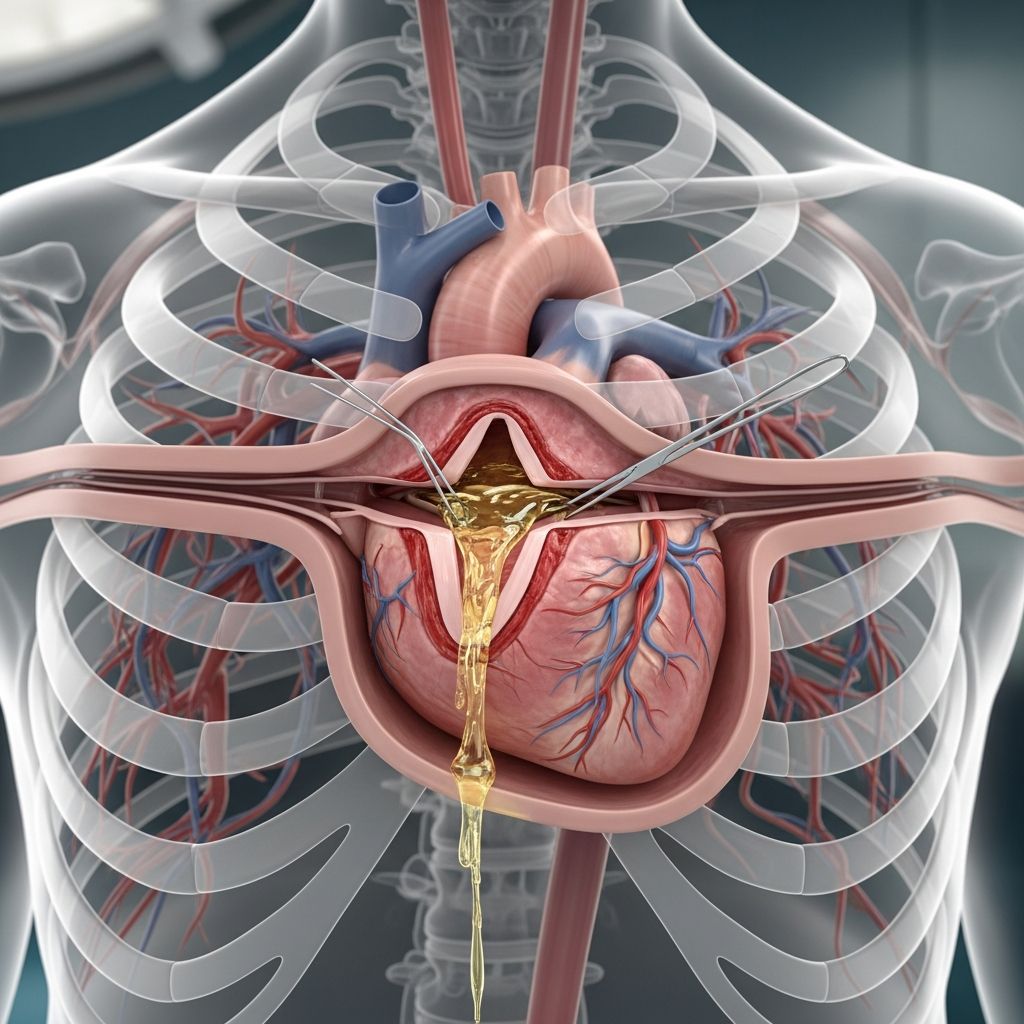
The heart is one of the body’s most vital organs, and it requires proper functioning conditions to maintain overall health. The heart is surrounded by a double-layered sac called the pericardium, which creates a protective barrier around this essential organ. Between these two layers lies a space known as the pericardial cavity, which normally contains a small amount of pericardial fluid. This fluid serves an important purpose—it prevents friction between the two layers of the pericardium and allows your heart to move more easily within the sac, reducing wear and tear on the organ.
However, in certain medical conditions, excess fluid can accumulate in the pericardial cavity. When this occurs, the condition is known as pericardial effusion. Because the pericardial cavity has limited space, this fluid accumulation leads to increased pressure around the heart, which can significantly impair its ability to function properly. When medication and other conservative treatments fail to resolve pericardial effusion, a surgical intervention known as a pericardial window (also called pericardiocentesis) may become necessary to restore normal heart function and prevent serious complications.
What Is a Pericardial Window?
A pericardial window is a minimally invasive surgical procedure designed to alleviate the symptoms and complications associated with pericardial effusion. During this procedure, surgeons make small incisions, typically 2 to 3 inches long, to access the pericardium. The procedure is performed under general anesthesia to ensure patient comfort and safety throughout the operation.
The primary objective of a pericardial window is to surgically remove a small portion of the pericardium, effectively creating an opening or “window” that allows excess fluid to drain from the pericardial space. This drainage relieves the pressure that has been building up around the heart, allowing it to resume normal contractions and circulation patterns. By establishing this drainage pathway, the procedure prevents complications such as cardiac tamponade, a life-threatening condition where fluid buildup restricts the heart’s ability to pump blood effectively.
Diagnostic Tests to Determine Need for the Procedure
Before recommending a pericardial window procedure, your physician will conduct a comprehensive evaluation to confirm the diagnosis of pericardial effusion and assess its severity. Several diagnostic tests may be employed to gather essential information:
- Chest X-Rays: Provide initial imaging to visualize the heart and surrounding structures, potentially showing signs of fluid accumulation.
- Electrocardiogram (EKG/ECG): Records electrical activity of the heart to detect abnormalities caused by fluid pressure.
- Blood Tests: Help identify underlying causes such as infection, inflammation, or malignancy.
- Echocardiogram (ECHO): Uses ultrasound technology to visualize the heart and precisely measure fluid accumulation in the pericardial space.
- Computed Tomography (CT Scan): Provides detailed cross-sectional images to assess fluid volume and distribution.
- Magnetic Resonance Imaging (MRI): Offers high-resolution images of the heart and surrounding tissues.
- Cardiac Catheterization: May be used to measure pressures and obtain fluid samples when necessary.
The echocardiogram has become the diagnostic method of choice for evaluating pericardial effusions due to its portability, wide availability, and accuracy in measuring fluid volume. Your doctor will determine which combination of these tests provides the most useful information for your specific situation.
Preparing for Pericardial Window Surgery
Adequate preparation is essential for ensuring a successful surgical outcome. Your doctor and the treatment team will take time to explain what you can expect before, during, and after the procedure, as well as potential risks involved. To prepare effectively, you should discuss several important topics with your healthcare provider:
Pre-Operative Consultations
Medications and Supplements: Inform your doctor about all medications, herbal products, and dietary supplements you are currently taking. Some medications may need to be discontinued before surgery, while others might need to be adjusted. Your doctor will provide specific recommendations for each medication.
Allergies and Sensitivities: Disclose any allergies to medicines, latex, tape, iodine, or anesthetic agents. This information is critical for preventing adverse reactions during the procedure.
Medical History: Report any history of bleeding disorders or clotting problems, as these can affect surgical planning and increase the risk of complications.
Body Modifications: Inform your doctor about any body piercings on your chest or abdomen, as these may need to be removed before surgery.
Radiation Exposure: Discuss any concerns about radiation exposure, particularly if you are pregnant or may be pregnant, as some diagnostic procedures involve radiation.
What to Expect During Pericardial Window Surgery
Understanding the procedural steps can help reduce anxiety and prepare you mentally for the experience. A pericardial window procedure typically takes between one and two hours to complete and is usually performed in an operating room.
Step-by-Step Procedure Overview
Preparation and Anesthesia: You will change into a hospital gown upon arrival at the operating room. A nurse will establish an intravenous (IV) line in your arm, which will be used to administer medications and fluids throughout the procedure. Your doctor will typically administer general anesthesia to make you unconscious and unaware during surgery. In some cases, doctors may opt for conscious sedation instead, administering medication to help you relax while maintaining minimal awareness.
Airway Management: Once you are adequately sedated, your doctor may insert a breathing tube (endotracheal tube) through your throat into your lungs and connect you to a mechanical ventilator. This equipment will breathe for you during the surgery, ensuring adequate oxygen supply to your body.
Surgical Access: Your surgeon will make an incision a few inches below your breastbone or between your ribs, depending on the surgical approach chosen. Specialized surgical tools are then inserted through this incision to access the pericardium.
Creating the Window: The surgeon carefully removes a small portion of the pericardium, creating an opening that allows fluid to drain from the pericardial space. This drainage pathway prevents fluid reaccumulation and relieves pressure on the heart.
Fluid Drainage: Following the creation of the pericardial window, a chest tube is placed between the layers of the pericardium or in the chest cavity to facilitate ongoing fluid drainage. A sample of the drained fluid may be sent to a laboratory for analysis to identify potential underlying causes of the effusion.
Closure: The muscle and skin incisions are carefully closed with sutures, and a sterile bandage is applied to protect the surgical site.
Recovery and Post-Operative Care
The recovery period following a pericardial window procedure requires careful monitoring and adherence to specific guidelines to promote optimal healing and prevent complications.
Immediate Post-Operative Period
After surgery, you will be transferred to either a stepdown unit or the cardiothoracic intensive care unit (CTICU), depending on your overall condition and the complexity of your case. Most patients remain hospitalized for 5 to 7 days following the procedure.
During your hospital stay, medical staff will closely monitor your vital signs, including heart rate, breathing, blood pressure, and oxygen saturation levels. You will likely have a drainage tube remaining in place to remove fluid from your heart or chest cavity. It is normal to experience some soreness at the surgical site, but severe pain should not occur. Pain medications are available if needed to manage discomfort.
Nutrition and Hydration
You will typically be able to drink starting the day after surgery. As your body tolerates it, you can gradually return to regular foods. Your medical team will provide specific guidance on dietary progression based on your individual recovery.
Mobilization and Activity
Early mobilization is an important component of recovery. Ambulation (walking) is usually initiated on the first or second day following surgery. This activity promotes circulation, prevents blood clots, and supports overall recovery.
While you can probably resume normal activities fairly quickly, you should proceed gradually and avoid overexertion initially. Heavy lifting and vigorous exercise should be avoided until your body has completely healed. Your doctor will provide specific instructions regarding activity restrictions and progression.
Long-Term Recovery Guidelines
| Recovery Phase | Timeline | Activities and Restrictions |
|---|---|---|
| Immediate Post-Op | Days 1-2 | Bed rest with monitored ambulation; pain management; vital sign monitoring |
| Early Recovery | Days 3-7 | Gradual increase in walking; normal diet as tolerated; chest tube removal; hospital discharge |
| Home Recovery | Weeks 1-4 | Light activities only; avoid heavy lifting; follow wound care instructions; attend follow-up appointments |
| Full Recovery | Weeks 4-8 | Gradual return to normal activities; resume exercise as tolerated; return to work if appropriate |
Potential Risks and Complications
While pericardial window is considered a relatively safe procedure for treating pericardial effusion, all surgical interventions carry some degree of risk. Potential complications can include infection at the surgical site, bleeding, damage to surrounding cardiac structures, or in rare cases, heart failure. Your surgical team will take every precaution to minimize these risks through careful technique and comprehensive post-operative monitoring.
Conditions Treated by Pericardial Window
Pericardial window is an effective treatment for various conditions causing pericardial effusion. These conditions may include malignancy (such as lung cancer), infection, inflammation, trauma, or idiopathic causes where no specific underlying condition can be identified. The procedure is particularly valuable in patients with recurrent effusions or those whose effusions are causing hemodynamic compromise.
Frequently Asked Questions
Q: How long does a pericardial window procedure typically take?
A: The procedure typically takes between one and two hours to complete, depending on the complexity of your case and any additional findings during surgery.
Q: Will I be asleep during the procedure?
A: Yes, you will receive general anesthesia, which means you will be unconscious throughout the procedure. In rare cases, conscious sedation may be used instead.
Q: How long will I need to stay in the hospital?
A: Most patients remain hospitalized for 5 to 7 days following a pericardial window procedure, though this may vary based on individual recovery progress.
Q: When can I return to normal activities?
A: You can usually resume light normal activities fairly quickly, though you should avoid heavy lifting and vigorous exercise for several weeks. Your doctor will provide specific guidance based on your recovery.
Q: What are the signs of complications I should watch for?
A: Contact your doctor immediately if you experience severe chest pain, difficulty breathing, fever, excessive bleeding from the incision, or signs of infection such as redness or swelling.
Q: Can the fluid come back after the procedure?
A: The pericardial window allows continued drainage, significantly reducing the risk of fluid reaccumulation. However, if reaccumulation occurs, additional treatment options are available.
Q: What causes pericardial effusion?
A: Pericardial effusion can result from various conditions including malignancy, infection, inflammation (pericarditis), trauma, kidney disease, or may occur without an identifiable cause (idiopathic).
References
- Pericardial Window — RWJBarnabas Health. Accessed 2025. https://www.rwjbh.org/treatment-care/heart-and-vascular-care/tests-procedures/pericardial-window/
- Pericardial Window for Lung Cancer — MyLungCancerTeam. Accessed 2025. https://www.mylungcancerteam.com/treatments/pericardial-window
- Pericardiectomy and Pericardial Window for the Treatment of Pericardial Disease — Raina et al. Current Cardiology Reports, Vol. 24, 2022. https://pubmed.ncbi.nlm.nih.gov/36029363/
- Pericardial Window — Harris Health System Health Library. Accessed 2025. https://healthlibrary.harrishealth.org/Library/TestsProcedures/Cardiovascular/135,359
- Pericardial Effusion and Tamponade: Evaluation, Imaging Modalities, and Management — Johns Hopkins University. Comprehensive Therapy, Vol. 21, No. 7, 1995. https://pure.johnshopkins.edu/en/publications/pericardial-effusion-and-tamponade-evaluation-imaging-modalities–4
Read full bio of medha deb