Pityriasis Rubra Pilaris Pathology
Detailed histopathological examination of pityriasis rubra pilaris, a rare papulosquamous skin disorder with distinctive epidermal changes.
Pityriasis rubra pilaris (PRP) pathology
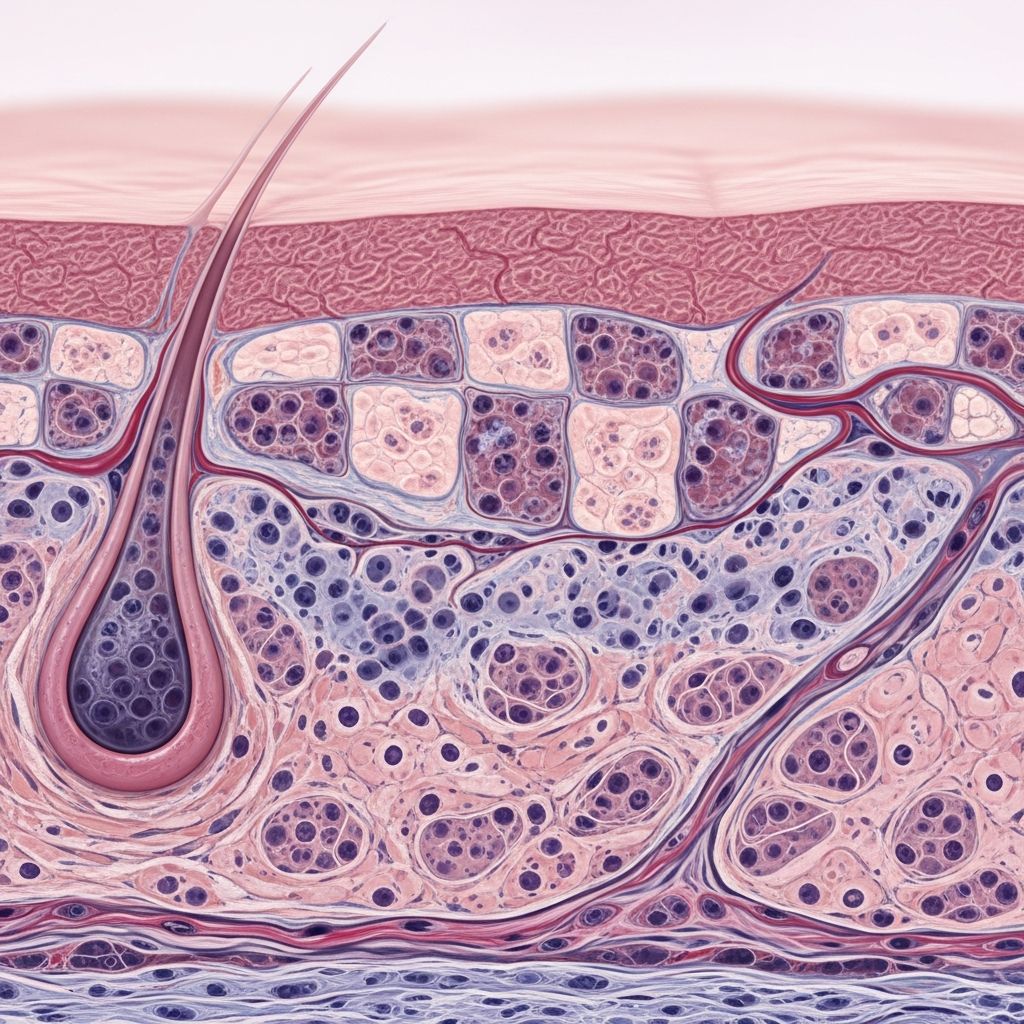
Pityriasis rubra pilaris (PRP) is a rare, chronic inflammatory skin disorder characterized by papulosquamous eruptions with follicular plugging and perifollicular erythema. Clinically, it manifests as reddish-orange plaques, palmoplantar keratoderma, and keratotic follicular papules that coalesce into well-demarcated lesions. Histopathologically, PRP exhibits distinctive features that aid in diagnosis, distinguishing it from mimics like psoriasis and mycosis fungoides.
Histopathology description
The epidermis in PRP displays
regular acanthosis
andpsoriasiform hyperplasia
, forming elongated rete ridges with a thickened stratum corneum. A hallmark is the irregular hyperkeratosis featuring alternating zones of orthokeratosis and parakeratosis in both vertical and horizontal directions, often described as a ‘checkerboard’ or ‘shoulder parakeratosis’ pattern around follicular structures. Follicular plugging is prominent, with hyperkeratotic material tracking down follicular openings, creating keratotic plugs.The granular layer is typically normal or focally hyperplastic (hypergranulosis) beneath parakeratotic areas, contrasting with the hypogranulosis seen in psoriasis. Suprapapillary plates are thickened, and rete ridges are broad with narrow dermal papillae. Dermal changes include a sparse, superficial perivascular lymphohistiocytic infiltrate, which may appear lichenoid in some cases. Rarely, focal acantholysis or spongiosis may occur, occasionally resembling Grover’s disease or Darier disease.
These features are consistent across PRP subtypes, though severity varies. In classic adult-onset PRP, pronounced follicular involvement predominates, while atypical forms may show milder hyperplasia.
Microscopic (histologic) images
- Figure 1: Low-power view showing psoriasiform hyperplasia with irregular parakeratosis and follicular plugging. The epidermis exhibits regular acanthosis, and orthokeratotic columns alternate with parakeratotic foci tracking into follicles.
- Figure 2: Medium-power magnification highlighting the ‘checkerboard’ pattern of ortho- and parakeratosis, shoulder parakeratosis around follicles, and thickened suprapapillary plates.
- Figure 3: High-power image demonstrating focal acantholysis within hyperplastic epidermis, sparse dermal infiltrate, and prominent follicular keratin plugs.
These images illustrate the pathognomonic vertical and horizontal parakeratosis alternating with orthokeratosis, a feature emphasized in studies of over 55 PRP cases.
Pathology resources tip
For further visual references on PRP histopathology, consult peer-reviewed atlases or databases like PubMed Central’s StatPearls, which provide detailed images of PRP lesions alongside clinical correlates.
Differential diagnosis
PRP’s histologic overlap with other papulosquamous disorders necessitates careful differentiation. Key mimics include:
- Psoriasis: Features spongiform pustules, neutrophils in the stratum corneum, thin suprapapillary plates, and diminished granular layer. PRP lacks neutrophils and shows thick suprapapillary plates with alternating parakeratosis.
- Syphilis (secondary): Psoriasiform eruption with lichenoid infiltrate, plasma cells, and endothelial swelling. Plasma cells are absent in PRP.
- Mycosis fungoides: Mixed psoriasiform, spongiotic, and lichenoid patterns with atypical lymphocytes. PRP lacks epidermotropism and Pautrier microabscesses.
- Follicular disorders (e.g., Darier disease): More pronounced acantholysis and dyskeratosis; PRP acantholysis is focal and rare.
| Feature | PRP | Psoriasis | Mycosis Fungoides |
|---|---|---|---|
| Acanthosis | Regular, psoriasiform | Regular, psoriasiform | Irregular, epidermotropic |
| Parakeratosis | Checkerboard (vertical/horizontal) | Uniform | Focal, with lymphocytes |
| Granular layer | Normal/thickened | Hypogranulosis | Variable |
| Infiltrate | Sparse lymphohistiocytic | Neutrophils | Atypical lymphocytes |
| Follicular plugging | Prominent | Absent | Rare |
This table summarizes distinguishing histologic criteria, supported by comparative analyses.
Special stains
Special stains are rarely required for PRP diagnosis, as routine H&E sections suffice. However:
- PAS (Periodic acid-Schiff): Useful to exclude fungal infections (e.g., tinea) mimicking follicular plugging. Negative in PRP.
- Immunohistochemistry (IHC): Not routinely needed but may employ CD1a or Langerin for inconclusive cases to rule out mycosis fungoides.
Electron microscopy occasionally reveals keratin filament abnormalities but is not practical for routine use.
Oral / genital pathology
Oral involvement in PRP is uncommon but may show hyperkeratotic plaques on tongue or buccal mucosa with similar psoriasiform changes. Genital lesions mirror cutaneous findings: erythematous plaques with scale and follicular prominence, lacking acanthosis as prominently.
Dermoscopy (optional information)
Dermoscopy aids clinical-pathologic correlation, revealing keratotic plugs with central hair, yellow-pink halos, and dotted vessels in follicular papules. This complements histopathology by highlighting perifollicular erythema and plugging pre-biopsy.
Frequently Asked Questions
What is the hallmark histopathologic feature of PRP?
The ‘checkerboard’ pattern of alternating orthokeratosis and parakeratosis both vertically and horizontally, with shoulder parakeratosis and follicular plugging.
How does PRP histopathology differ from psoriasis?
PRP shows thick suprapapillary plates, normal/hyperplastic granular layer, no neutrophils, and follicular involvement; psoriasis has thin plates, hypogranulosis, and spongiform pustules.
Is special staining necessary for PRP diagnosis?
No, H&E is diagnostic; PAS rules out fungi if needed.
Can PRP show acantholysis?
Rarely, focal acantholysis may mimic Grover’s or Darier disease, but it’s not a dominant feature.
What subtypes share these histologic features?
All six subtypes (classic juvenile/adult, atypical, circumscribed, HIV-associated) exhibit core features like psoriasiform acanthosis and checkerboard parakeratosis.
Clinical Context and Prognosis
Understanding pathology informs management. PRP’s idiopathic nature involves keratinocyte hyperproliferation and immune dysregulation, potentially driven by TNF-α and IL-12/23 pathways. Biopsy confirmation guides therapy, from topicals for limited disease to biologics (e.g., ustekinumab) for refractory erythroderma. Prognosis varies: classic forms remit in 3-5 years, atypical persists chronically.
Severe cases feature erythroderma (90-100% BSA), palmoplantar keratoderma with fissures, nail dystrophy, and systemic symptoms like fatigue, arthralgias, and psychosocial distress including suicidal ideation. Early pathologic diagnosis prevents complications like ectropion or secondary infections.
In children, circumscribed juvenile PRP affects knees/elbows with identical histology but self-limits. HIV-associated PRP responds to antiretroviral therapy alongside skin-directed treatments.
Research Insights
Recent studies affirm histologic criteria from 1980s analyses, with molecular profiling revealing upregulated keratins (K6, K16) in hyperproliferative epidermis. Biologics targeting IL-23/IL-17 pathways show promise, mirroring psoriasis responses but with PRP-specific follicular emphasis.
Genetic subtypes (atypical juvenile) link to CARD14 mutations, explaining persistent hyperplasia. Future diagnostics may integrate RNA sequencing for precise subtyping.
References
- Pityriasis Rubra Pilaris – StatPearls — Bolognia JL, Schaffer JV, Cerroni L (eds). 2023-10-01. https://www.ncbi.nlm.nih.gov/books/NBK482436/
- Pityriasis rubra pilaris (PRP) pathology — DermNet NZ. 2023. https://dermnetnz.org/topics/pityriasis-rubra-pilaris-pathology
- Histologic criteria for the diagnosis of pityriasis rubra pilaris — Weedon D. Am J Dermatopathol. 1986. https://pubmed.ncbi.nlm.nih.gov/3766917/
- Pityriasis Rubra Pilaris — JAMA Dermatology. 2019-05-01. https://jamanetwork.com/journals/jamadermatology/fullarticle/2723286
- Pityriasis Rubra Pilaris and variants — Dermatology Advisor. 2024. https://www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/pityriasis-rubra-pilaris-and-variants-devergies-disease-lichen-acuminatus-lichen-psoriasis-lichen-ruber-acuminatus-lichen-ruber-pilaris-pityriasis-pilaris/
Read full bio of medha deb