Plague
Comprehensive guide to plague: causes, symptoms, transmission, treatment, and prevention of this deadly bacterial infection.
Authoritative facts from DermNet New Zealand and high-credibility sources including CDC, WHO, and peer-reviewed literature.
What is plague?
Plague is a serious bacterial infection caused by Yersinia pestis, a zoonotic pathogen primarily found in rodents and their fleas. This disease has afflicted humans for millennia, most notoriously during the Black Death in the 14th century, which killed an estimated 30-60% of Europe’s population. Today, plague persists in endemic areas, with 1-2 thousand cases reported annually worldwide, mainly in Africa, Asia, and the Americas.
The bacterium thrives in small mammals like rats, ground squirrels, and prairie dogs. Humans become incidental hosts through flea bites, handling infected animals, or inhaling respiratory droplets in pneumonic cases. Without prompt treatment, plague has a case-fatality rate of 30-100%, but antibiotics reduce mortality to 4-15% if administered early.
Who gets plague?
Plague affects individuals exposed to infected animals or fleas, particularly in rural or sylvatic (wild) cycles. High-risk groups include:
- Hunters, trappers, and veterinarians handling rodents or carnivores like cats that prey on infected wildlife.
- Residents in endemic regions such as the southwestern United States (e.g., New Mexico, Arizona), Madagascar, Democratic Republic of Congo, and parts of Asia.
- Travelers to plague-endemic areas without precautions.
- Those in close contact with infected patients in pneumonic plague outbreaks, though human-to-human transmission is rare except for this form.
Globally, over 90% of cases occur in Africa. In the US, 7-17 cases are reported yearly, mostly bubonic form from flea bites. Children and immunocompromised individuals face higher risks due to weaker immune responses.
What causes plague?
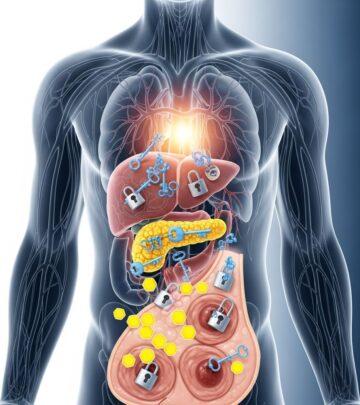
Yersinia pestis is a Gram-negative, rod-shaped bacterium equipped with virulence factors like the F1 capsule antigen and plasminogen activator (pla gene), enabling immune evasion and tissue invasion. Transmission occurs via:
- Flea bites (primary route): Infected fleas regurgitate bacteria into the bite wound during feeding. Key vectors include Xenopsylla cheopis (oriental rat flea) and squirrel fleas.
- Direct contact: Handling tissues or fluids from infected animals, causing percutaneous inoculation.
- Inhalation: Aerosolized droplets from pneumonic plague patients or lab accidents, leading to primary pneumonic plague.
The bacterium multiplies in macrophages, travels to lymph nodes, and secretes toxins causing inflammation and necrosis. If untreated, it disseminates systemically.
What are the clinical features of plague?
Plague manifests in three primary forms, with overlapping symptoms like high fever (>38°C/100.4°F), chills, headache, weakness, and myalgias. Incubation is 1-7 days (typically 2-6).
Bubonic plague (80-95% of cases)
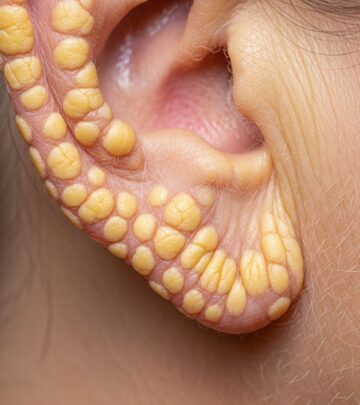
The most common form, resulting from flea bites. Bacteria reach regional lymph nodes, causing painful swelling called buboes (1-10 cm, tense, tender). Common sites: groin (femoral), armpit (axillary), neck (cervical). Patients exhibit intense pain preventing movement; buboes may suppurate. A pustule or eschar may appear at the bite site in 25% of cases. Untreated mortality: 30-60%.
Septicemic plague (10-30% of cases)
Bacteria invade the bloodstream, causing fever, chills, abdominal pain, shock, and disseminated intravascular coagulation (DIC). Blackened acral gangrene (fingers, toes, nose) earns it the name “Black Death.” Bleeding under skin/organs occurs; mortality nears 100% untreated.
Pneumonic plague (<5% naturally occurring)
The deadliest form (mortality 90-100% untreated), involving lungs. Symptoms: rapid-onset pneumonia with dyspnea, chest pain, hemoptysis (bloody sputum). Primary (inhalation) or secondary (from bubonic/septicemic). Highly contagious via droplets; rapid progression to respiratory failure.
Rare forms
- Pharyngeal plague: Sore throat, cervical buboes from ingesting infected tissues.
- Meningeal plague: Headache, stiff neck from CNS spread.
- Ocular plague: Conjunctivitis, eye pain.
| Form | Transmission | Key Symptoms | Untreated Mortality |
|---|---|---|---|
| Bubonic | Flea bite | Buboes, fever, pain | 30-60% |
| Septicemic | Flea bite/contact | Shock, gangrene, bleeding | ~100% |
| Pneumonic | Droplets/secondary | Hemoptysis, pneumonia | 90-100% |
How is the diagnosis of plague made?
Suspect plague in endemic areas with compatible exposure and symptoms. Rapid diagnosis is critical.
- Clinical: Buboes, fever, exposure history.
- Laboratory:
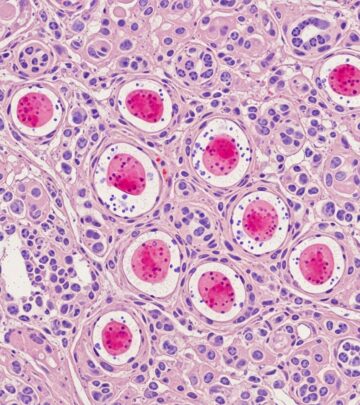
- Gram stain/culture of bubo aspirate, blood, sputum: bipolar ‘safety pin’ rods.
- PCR for pla/caf1 genes: highly sensitive, works post-antibiotics.
- Serology (F1 antigen): retrospective.
- Rapid tests: antigen detection.
Notify public health immediately; use BSL-3 labs.
What is the treatment for plague?
Empiric antibiotics within 18-24 hours of symptoms yield >80% survival. Preferred regimens per CDC/WHO:
| Drug | Adults | Children | Duration |
|---|---|---|---|
| Gentamicin | 5 mg/kg IM/IV daily | 2.5 mg/kg q8-12h | 10-14 days |
| Doxycycline | 100 mg BID PO/IV | 2.2 mg/kg BID | 10-14 days |
| Levofloxacin | 500 mg daily | 8 mg/kg daily | 10-14 days |
| Ciprofloxacin | 400 mg BID IV / 500 mg BID PO | 15 mg/kg BID | 10-14 days |
Supportive care: fluids, oxygen, drainage of buboes. Contacts receive 7-day prophylaxis (doxycycline).
What is the outcome for plague?
With early treatment, survival exceeds 85%. Complications include chronic lymphedema, gangrene amputations, ARDS, multiorgan failure. Survivors may have bubo scars or acral necrosis. Untreated pneumonic plague kills within 24-48 hours.
How can plague be prevented?
- Avoid exposure: Flea repellent (DEET), treat pets, avoid wild rodent areas.
- Rodent control: Sanitation, poison bait in endemic zones.
- Prophylaxis: Antibiotics for exposures.
- Vaccination: Not routine; available for high-risk lab workers.
- Isolation: Droplet precautions for pneumonic suspects.
Plague images
Clinical images typically show inflamed buboes in groin/armpits, acral gangrene, hemorrhagic sputum. (Descriptions based on medical literature; consult secure image databases for visuals.)
Frequently Asked Questions
Is plague contagious from person to person?
Bubonic/septicemic: No. Pneumonic: Yes, via respiratory droplets; isolate suspects.
Can plague be treated at home?
No—requires IV antibiotics in hospital. Seek immediate care for symptoms post-exposure.
Is plague still around today?
Yes, ~200 US cases since 1970s; thousands globally yearly.
What does a plague bubo look like?
Swollen, red-purple, exquisitely tender lymph node mass.
Can cats get plague?
Yes; cats develop cervical buboes/pharyngitis and can transmit pneumonic form.
References
- Plague (disease) — Wikipedia (citing primary sources). 2024. https://en.wikipedia.org/wiki/Plague_(disease)
- Signs and Symptoms of Plague — Centers for Disease Control and Prevention (CDC). 2024-10-17. https://www.cdc.gov/plague/signs-symptoms/index.html
- Plague — StatPearls, NCBI Bookshelf, National Library of Medicine. 2023-07-17. https://www.ncbi.nlm.nih.gov/books/NBK549855/
- Plague – Symptoms and causes — Mayo Clinic. 2024. https://www.mayoclinic.org/diseases-conditions/plague/symptoms-causes/syc-20351291
- Plague — MedlinePlus, U.S. National Library of Medicine. 2024. https://medlineplus.gov/plague.html
- Plague — World Health Organization (WHO). 2024. https://www.who.int/health-topics/plague
Read full bio of Sneha Tete