Primary Cutaneous CD30+ Lymphoproliferative Disorders
Understanding the spectrum of indolent skin lymphomas featuring CD30+ T-cells: LyP and pcALCL.
Primary cutaneous CD30+ lymphoproliferative disorders (LPD) represent a spectrum of indolent-behaving extranodal T-cell neoplasms confined primarily to the skin, defined by prominent CD30 expression on atypical lymphocytes. These disorders constitute approximately 30% of cutaneous T-cell lymphomas (CTCL), making them the second most common subtype after mycosis fungoides.
Introduction
Primary cutaneous CD30+ LPD encompass two main entities:
lymphomatoid papulosis (LyP)
andprimary cutaneous anaplastic large cell lymphoma (pcALCL)
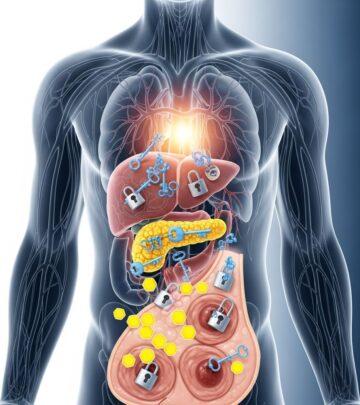
, along with borderline cases that blur the lines between them. Despite alarming histopathologic features mimicking aggressive malignancies, these conditions typically follow a benign, waxing-and-waning course with excellent prognosis. LyP presents as recurrent self-resolving papulonodular eruptions, while pcALCL manifests as solitary or localized tumorous lesions. Accurate clinicopathologic correlation is essential, as misdiagnosis can lead to overtreatment.CD30, a cell surface glycoprotein belonging to the tumor necrosis factor receptor superfamily, is expressed by activated lymphocytes and serves as a key diagnostic marker. Its ligation influences lymphoid cell proliferation, survival, and apoptosis. These disorders highlight the paradox of malignant-appearing histology with indolent behavior, underscoring the importance of clinical context in lymphoma classification.
Demographics
Primary cutaneous CD30+ LPD are rare, with an estimated incidence of 0.24 per 100,000 person-years for LyP and 0.04 for pcALCL. They affect all ages, races, and both sexes, though subtle differences exist:
- LyP: Peaks in adults (median age 45 years), but up to 20% of cases occur in children under 20. Slight male predominance (M:F ratio 1.5:1).
- pcALCL: Predominantly middle-aged to elderly adults (median age 60-65 years), with marked male predominance (M:F ratio 2-3:1). Rare in children.
No strong racial predilection is noted, though most reported cases originate from Caucasian populations due to referral biases in dermatology literature.
Causes
The exact aetiopathogenesis remains unclear, but several hypotheses implicate dysregulated immune responses and genetic alterations:
- CD30 signaling pathway dysregulation promotes lymphoid cell survival and proliferation.
- Clonal T-cell receptor (TCR) gene rearrangements in 40-60% of LyP and 65-90% of pcALCL cases suggest neoplastic rather than purely reactive processes.
- Association with other lymphomas: Up to 20-40% of LyP patients develop secondary cutaneous or systemic lymphomas, including mycosis fungoides.
- Potential viral triggers (e.g., herpesviruses) or environmental factors are postulated but unproven.
- pcALCL rarely harbors ALK translocations (unlike systemic ALCL), but other genetic abnormalities like NF-κB pathway activation occur.
These disorders arise from mature post-thymic CD4+ T-cells in most cases, with variant phenotypes expressing CD8 or lacking pan-T-cell markers.
Clinical Features
Lymphomatoid Papulosis (LyP)
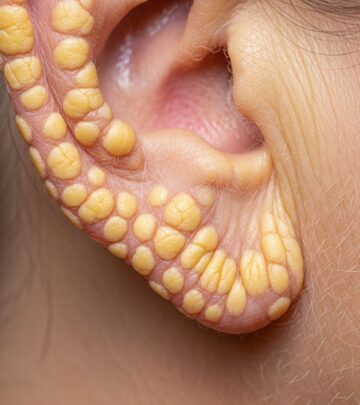
LyP is characterized by recurrent crops of self-healing papules and nodules that evolve over weeks: erythematous papules progress to hemorrhagic or necrotic papulonodules (0.5-2 cm), often ulcerate centrally, and resolve with varioliform scarring. Lesions number from few to hundreds, with disease duration spanning decades. Distribution favors trunk and extremities; mucosal involvement is rare. Individual lesions persist 2-12 weeks, with new crops appearing asynchronously.
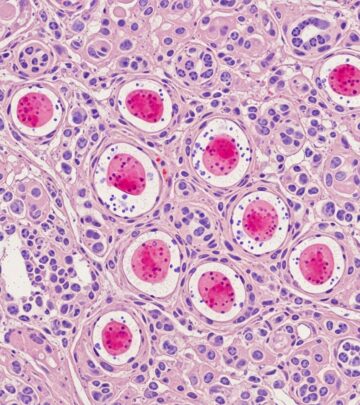
Five histologic subtypes exist:
- Type A (75%): Wedges of mixed inflammatory infiltrate with scattered large CD30+ anaplastic cells (15-100% of infiltrate).
- Type B (5%): Epidermotropic small atypical CD30+ lymphocytes resembling mycosis fungoides.
- Type C (10%): Cohesive sheets of large CD30+ cells mimicking pcALCL.
- Type D (5%): CD8+ epidermotropic medium-sized pleomorphic cells.
- Type E (<5%): Angiodestructive CD8+ CD30+ infiltrates with extensive necrosis.
Primary Cutaneous Anaplastic Large Cell Lymphoma (pcALCL)
pcALCL presents with solitary or localized nodules/tumors (>2 cm), often ulcerated, coalescing into plaques. Multifocal skin involvement occurs in 20%. Extracutaneous spread (regional nodes) in 10%, but distant dissemination is rare. Legs involvement portends worse prognosis.
Histologically, >75% tumor cells are large anaplastic/pleomorphic CD30+ cells with abundant cytoplasm. Loss of pan-T antigens (CD2, CD3, CD5, CD7) is common.
Complications
Despite indolent behavior, complications include:
- Secondary lymphomas in 20% of LyP (mycosis fungoides, pcALCL, Hodgkin lymphoma).
- pcALCL progression to extracutaneous disease (50% five-year survival if generalized).
- Scarring, infection from ulcerations.
- Psychosocial impact from chronic recurrent lesions.
Diagnosis
Requires integration of clinical history, morphology, histopathology, immunophenotype, and clonality studies:
| Feature | LyP | pcALCL |
|---|---|---|
| Lesion size/persistence | <2 cm, self-resolve weeks | >2 cm, persistent |
| CD30+ cells | 15-100%, scattered | >75%, cohesive |
| TCR clonality | 40-60% | 65-90% |
Immunohistochemistry: CD30+, CD4+ (most), variable CD8+. ALK- distinguishes from systemic ALCL. TCR gene rearrangement by PCR confirms clonality.
Differential Diagnoses
- Reactive: Arthropod bites, pityriasis lichenoides (PLEVA).
- Other CTCL: Transformed mycosis fungoides, pc aggressive epidermotropic CD8+ lymphoma, gamma/delta T-cell lymphoma.
- Systemic ALCL: ALK+, multifocal nodal disease precedes skin.
Treatment
Tailored to extent and subtype:
- Observation: For limited LyP (<5-10 lesions).
- Skin-directed: Topical corticosteroids, nitrogen mustard, phototherapy (NB-UVB, PUVA) for LyP; radiotherapy for localized pcALCL.
- Systemic: Low-dose methotrexate (first-line for multifocal disease), bexarotene.
- Targeted: Brentuximab vedotin (anti-CD30) highly effective (ORR 75-100%).
- Surgical excision: Solitary pcALCL lesions.
Outcome
Excellent prognosis: LyP 100% 5-year survival; pcALCL 95% (skin-limited), 50% if extracutaneous. Long-term monitoring required for secondary malignancies.
Frequently Asked Questions (FAQs)
What is primary cutaneous CD30+ LPD?
A spectrum of skin-limited T-cell lymphomas featuring CD30+ cells, including LyP and pcALCL, with indolent behavior.
Is LyP cancerous?
Clonal but behaves benignly; associated with risk of other lymphomas in 20%.
How is pcALCL distinguished from LyP?
Larger persistent tumors, >75% CD30+ cohesive cells vs. self-resolving papules.
What is the best treatment for multifocal LyP?
Low-dose methotrexate or phototherapy; brentuximab vedotin for refractory cases.
Does pcALCL spread?
Rarely beyond skin (10%); regional nodes do not worsen prognosis.
References
- Primary cutaneous CD30+ lymphoproliferative disorders — DermNet NZ. 2023. https://dermnetnz.org/topics/primary-cutaneous-cd30-positive-lymphoproliferative-disorders
- CD30-positive primary cutaneous lymphoproliferative disorders — NIH/PMC. 2019-02-01. https://pmc.ncbi.nlm.nih.gov/articles/PMC6355473/
- Primary cutaneous CD30(+) lymphoproliferative disorders — PubMed. 2016-08. https://pubmed.ncbi.nlm.nih.gov/27509411/
- The spectrum of CD30+ T cell lymphoproliferative disorders in the skin — AME Groups. 2020. https://cco.amegroups.org/article/view/23334/22727
- CD30+ lymphoproliferative disorders — Haematologica. 2008. https://haematologica.org/article/view/5744
Read full bio of Sneha Tete