Pseudomonas Infection: Causes, Symptoms & Treatment
Learn about Pseudomonas infections, risk factors, symptoms, and treatment options for this serious bacterial infection.
What Is a Pseudomonas Infection?
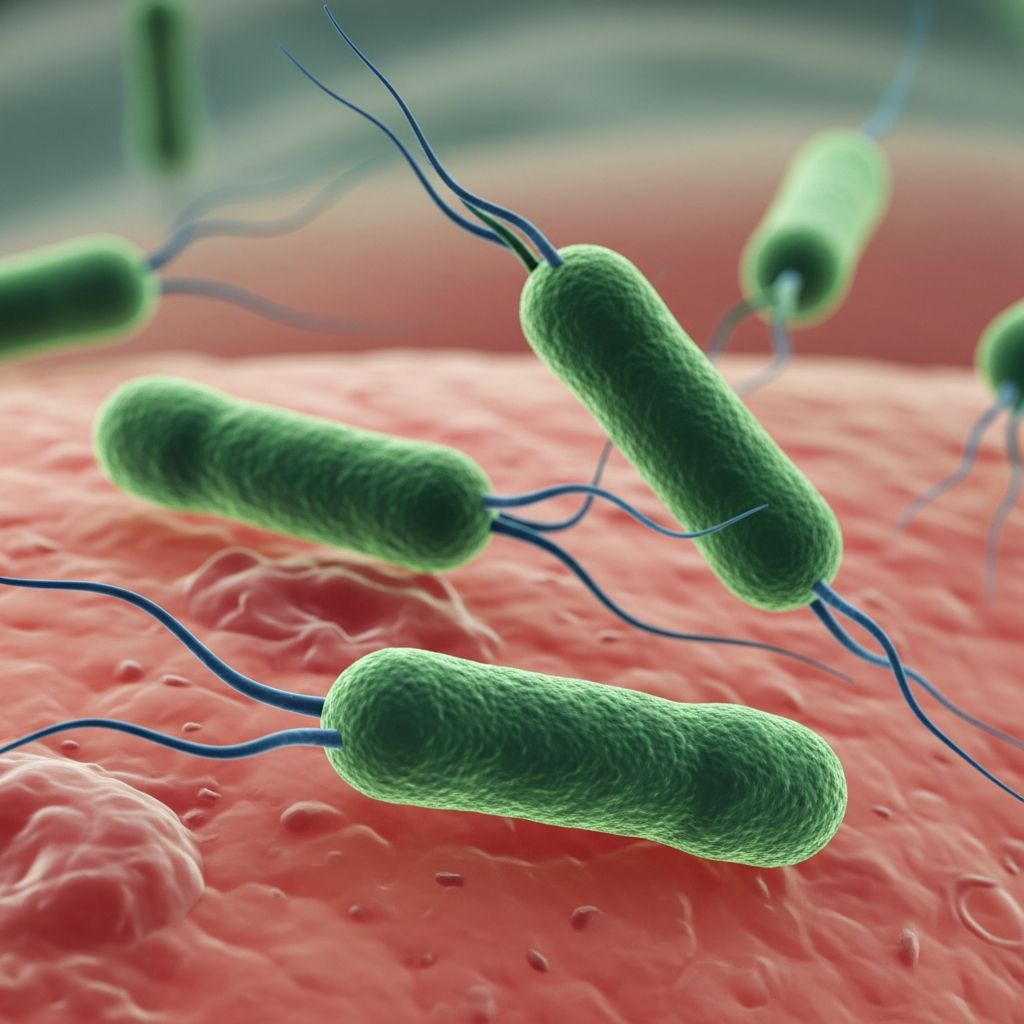
A Pseudomonas infection is a bacterial infection caused by the gram-negative bacterium Pseudomonas, most commonly Pseudomonas aeruginosa. This bacterium is opportunistic in nature, meaning it primarily affects individuals with weakened immune systems or those in healthcare settings. Pseudomonas aeruginosa is one of the most common and serious infections people acquire while hospitalized, and it can affect multiple body systems including the blood, lungs, urinary tract, skin, bones, eyes, ears, and central nervous system. The bacterium thrives in moist environments and is commonly found in soil, water, and various healthcare settings where it can contaminate medical equipment and surfaces.
How Pseudomonas Infections Develop
Pseudomonas aeruginosa is an opportunistic pathogen that attacks individuals with debilitated immune systems. The bacterium commonly enters the body through breaks in the skin or via medical devices such as urinary catheters, ventilators, or wound drainage systems. In healthcare settings, the infection can spread through contact with contaminated surfaces, equipment, or the hands of healthcare providers. Person-to-person transmission can occur through contaminated hands or exposure to contaminated respiratory droplets. Outside hospital environments, individuals may become infected through exposure to contaminated soil or water, particularly in warm, moist conditions like hot tubs or swimming pools.
Risk Factors and At-Risk Populations
Certain populations face significantly higher risk for Pseudomonas infections due to compromised immune function or environmental exposure. Understanding these risk factors is essential for prevention and early detection.
Hospitalized Patients
Patients in healthcare settings face the highest risk, particularly those:
– Using breathing machines (ventilators)- With indwelling medical devices such as catheters or feeding tubes- With open wounds from surgery or severe burns- In intensive care units (ICUs) for extended periods
Individuals with Chronic Conditions
Certain pre-existing health conditions significantly increase susceptibility to Pseudomonas infections:
– Diabetes mellitus- Cystic fibrosis and other chronic lung diseases- HIV/AIDS and other immunocompromising conditions- Cancer and malignancies requiring immunosuppressive treatment- Recent organ transplantation
Other High-Risk Groups
Additional populations at increased risk include individuals taking medications that suppress the immune system, those with severe wounds or burns, and people who have recently undergone medical procedures outside the United States where different strains may be prevalent.
Symptoms of Pseudomonas Infection
The symptoms of Pseudomonas infection vary significantly depending on which part of the body is affected. Early recognition of these symptoms is crucial for prompt diagnosis and treatment. Common manifestations include fever, which often indicates a severe infection. Specific symptoms by location of infection include:
Respiratory Tract Infections
When Pseudomonas aeruginosa infects the lungs, it typically causes pneumonia characterized by severe coughing, congestion, shortness of breath, and respiratory distress. Patients may require mechanical ventilation support. In individuals with cystic fibrosis, recurring lung infections with Pseudomonas aeruginosa are particularly problematic and can lead to progressive decline in lung function.
Skin and Wound Infections
Skin involvement may present as a characteristic rash with pustules or pimples filled with pus. Infected wounds produce distinctive green-colored pus or discharge that may emit a fruity odor, which is a hallmark sign of Pseudomonas contamination.
Urinary Tract Infections
Pseudomonas can cause urinary tract infections, particularly in patients with indwelling urinary catheters. Symptoms include dysuria, frequency, urgency, and cloudiness or discoloration of urine.
Other Site-Specific Symptoms
Eye infections present with pain, redness, and swelling. Ear infections cause pain and discharge. Bone and joint infections result in joint pain and swelling, with back or neck pain that may persist for weeks. Gastrointestinal infections cause headache and diarrhea. Bloodstream infections can lead to sepsis with systemic symptoms including high fever, hypotension, and organ dysfunction.
Diagnosis of Pseudomonas Infection
Accurate diagnosis of Pseudomonas infection is essential for appropriate treatment selection. Healthcare providers employ several diagnostic methods to confirm the presence of Pseudomonas aeruginosa and determine antibiotic susceptibility.
The primary diagnostic method involves culturing specimens from the infected site. Blood, wound drainage, body fluids, tissue samples, sputum, and urine are sent to the laboratory for bacterial culture. The culture identifies the causative organism and provides crucial information about which antibiotics will be effective against the specific strain isolated.
Supporting diagnostic tools include physical examination, stethoscope assessment for respiratory infections, ultrasound imaging, and radiological studies such as X-rays or computed tomography scans that may reveal lesions or abnormalities within the body. However, bacterial culture remains the gold standard for definitive diagnosis of Pseudomonas infection and antimicrobial susceptibility testing is performed to guide antibiotic selection, particularly important for identifying multidrug-resistant strains.
Treatment Options for Pseudomonas Infection
Treatment of Pseudomonas infections typically requires a comprehensive approach combining antimicrobial therapy with supportive care measures tailored to the patient’s clinical condition.
Antibiotic Therapy
Antipseudomonal antibiotics are used in combination to treat infections caused by susceptible strains. These may include fluoroquinolones, aminoglycosides, beta-lactam antibiotics, or carbapenems depending on susceptibility testing results. Combination therapy is often preferred over monotherapy to improve efficacy and reduce the development of resistance. However, treatment options are limited for multidrug-resistant Pseudomonas aeruginosa (MDR P. aeruginosa), particularly carbapenem-resistant strains, which are resistant to nearly all available antibiotics.
Supportive Care Measures
Depending on the severity and site of infection, patients may require hospitalization. For respiratory infections, mechanical ventilation support may be necessary. Surgical intervention may be indicated for source control, including wound debridement and drainage of abscesses. Fluid management, pain control, and treatment of any underlying conditions are essential components of comprehensive care.
Challenges in Treatment
The rise of antibiotic-resistant Pseudomonas strains presents significant treatment challenges. Some types are resistant to nearly all antibiotics, including carbapenems, classified as multidrug-resistant (MDR) Pseudomonas aeruginosa. In 2017, MDR P. aeruginosa caused an estimated 32,600 infections among hospitalized patients and approximately 2,700 deaths in the United States alone. Carbapenem-resistant Pseudomonas aeruginosa (CP-CRPA) is particularly concerning as it can transfer its genetic resistance to other bacteria, spreading antibiotic resistance further. The World Health Organization has identified CP-CRPA as a high priority pathogen, and the CDC lists it as a serious public health threat.
Complications of Pseudomonas Infection
Untreated or severe Pseudomonas infections can lead to serious complications. Antibiotic resistance can result in treatment failure, leading to increased healthcare costs, prolonged hospital stays, continued symptoms, and worsening clinical condition. Severe infections may progress to sepsis, a life-threatening condition where the immune system attacks the body’s own organs. Organ failure can occur when untreated or severe infections damage vital organ systems. In some individuals, particularly those with severely compromised immune systems, Pseudomonas infections can be life-threatening if not managed promptly and aggressively.
Prevention Strategies
Preventing Pseudomonas infection requires vigilance in both healthcare and community settings. Prevention approaches differ based on the setting but share common principles of infection control.
Individual and Caregiver Measures
– Keep hands clean, particularly before and after caring for wounds or handling medical devices- Remind healthcare providers and family members to wash hands before touching the patient or handling medical devices- Allow healthcare staff to clean the patient’s room daily in healthcare settings- Avoid tracking dirt from shoes into living spaces- Wash food carefully and drink safe water- Practice regular handwashing, especially after using the restroom or before eating
Healthcare Setting Measures
Healthcare facilities must implement core infection control practices to reduce transmission risk. These include having water management plans in place, as Pseudomonas thrives in moist environments. Regular cleaning and disinfection of equipment such as ventilators, catheters, restraints, and environmental surfaces is essential. Changing bandages frequently and avoiding prolonged catheter use when possible help reduce infection risk. Special attention should be paid to areas where moist conditions are common, such as bathrooms, cleaning equipment, and water systems.
Living with Pseudomonas Infection
For individuals with chronic conditions like cystic fibrosis who may experience recurring Pseudomonas infections, special considerations apply. Once infected with Pseudomonas aeruginosa, it can be difficult to completely eradicate the bacteria. Regular monitoring, prompt treatment of infections, and close follow-up care are essential. Early diagnosis and immediate initiation of treatment are critical for optimal outcomes and to prevent decline in lung function.
Current Public Health Response
Health agencies are actively working to address the Pseudomonas threat. The CDC provides testing through the Antimicrobial Resistance Laboratory Network to identify antimicrobial resistance cases and track transmission in healthcare settings. Data on Pseudomonas infections are tracked through the National Healthcare Safety Network, and resistance information is available through the AR & Patient Safety Portal. Health departments, federal agencies, and healthcare providers work collaboratively to prevent infections and slow the spread of resistant strains.
Frequently Asked Questions
Q: How common are Pseudomonas infections?
A: Pseudomonas aeruginosa is one of the most common and serious infections acquired in hospitals. In 2017 alone, multidrug-resistant strains caused an estimated 32,600 infections among hospitalized patients in the United States.
Q: Can Pseudomonas infection spread person-to-person?
A: Yes, Pseudomonas can spread through contaminated hands, respiratory droplets, and contact with infected wounds. This is why hand hygiene is crucial in healthcare settings and at home when caring for infected individuals.
Q: Is Pseudomonas infection always serious?
A: While mild infections may occur in healthy individuals, Pseudomonas is particularly dangerous for those with weakened immune systems, chronic lung disease, or hospitalization. In these populations, infections can become severe and life-threatening if not treated promptly.
Q: What makes some Pseudomonas strains resistant to antibiotics?
A: Pseudomonas aeruginosa has intrinsic resistance to many antibiotics and rapidly acquires resistance to new agents. Some strains develop multidrug resistance and can even transfer genetic resistance codes to other bacteria, similar to sharing answers to a test.
Q: How long does treatment for Pseudomonas infection take?
A: Treatment duration depends on the severity and site of infection, ranging from several days to weeks. Severe sepsis or complicated infections may require prolonged hospitalization and extended antibiotic therapy.
Q: Can I get Pseudomonas infection from a hot tub or swimming pool?
A: Yes, Pseudomonas aeruginosa thrives in warm, moist environments and can cause hot tub folliculitis, an infection of hair follicles. Proper maintenance and chlorination of pools and hot tubs help prevent this infection.
References
- About Pseudomonas aeruginosa — Centers for Disease Control and Prevention. 2023. https://www.cdc.gov/pseudomonas-aeruginosa/about/index.html
- Pseudomonas infections — EBSCO Research Starters. 2024. https://www.ebsco.com/research-starters/consumer-health/pseudomonas-infections
- How to Identify and Treat Pseudomonas Aeruginosa Infections — WebMD. 2024. https://www.webmd.com/a-to-z-guides/pseudomonas-infection
- Antimicrobial Treatment of Pseudomonas aeruginosa Severe Sepsis — PubMed/NCBI. 2022. https://pubmed.ncbi.nlm.nih.gov/36290092/
- Hot Tub Folliculitis: Rash, Symptoms, Causes & Treatment — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/diseases/23358-hot-tub-folliculitis
- Antibiotic Resistance: What Is It, Complications & Treatment — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/articles/21655-antibiotic-resistance
Read full bio of medha deb











