Reproductive Glands: Function, Health & Common Conditions
Understanding the role of reproductive glands in sexual health and overall wellness.
Understanding Reproductive Glands: Function, Health & Common Conditions
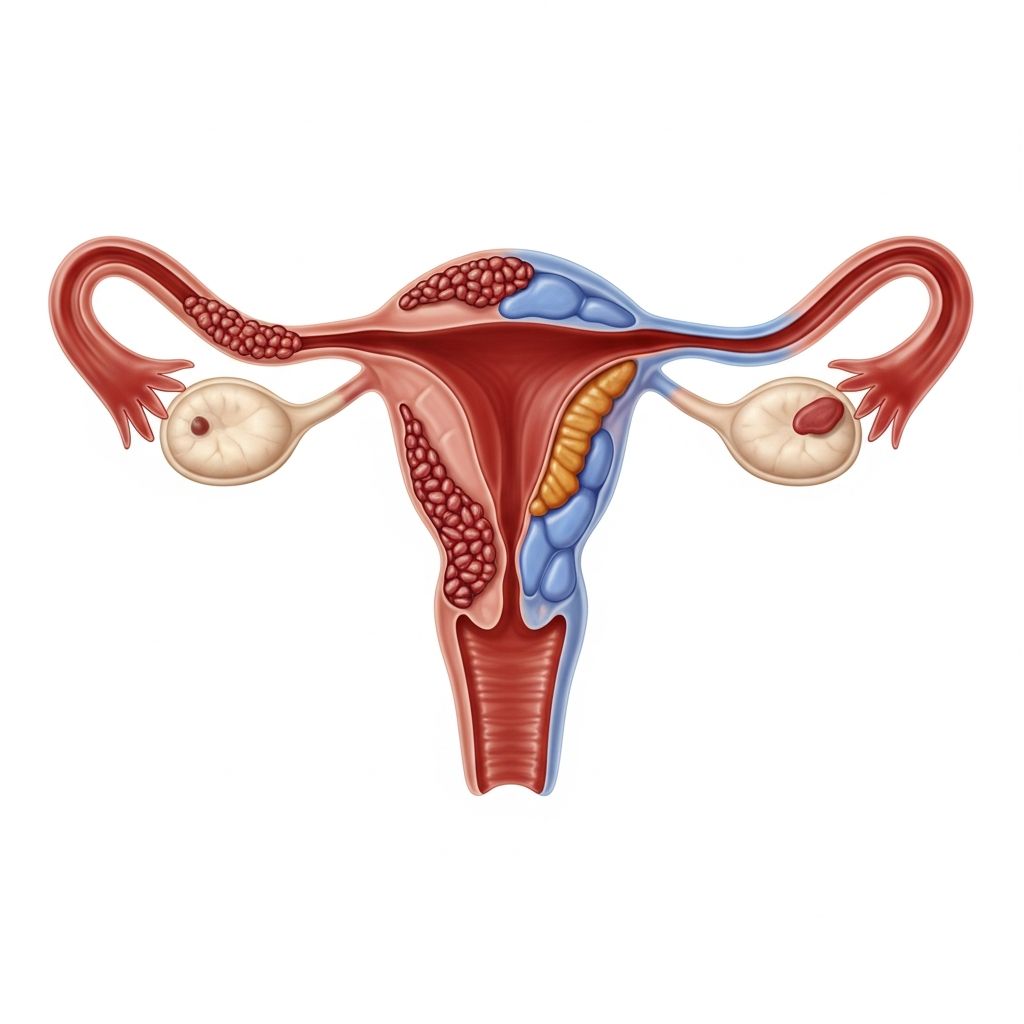
Reproductive glands are essential components of the endocrine system responsible for producing hormones that regulate sexual development, reproduction, and overall health. These glands—including the ovaries in females and testes in males—play a crucial role in maintaining hormonal balance throughout your lifetime. Understanding how these glands function and recognizing potential health concerns is vital for maintaining reproductive wellness.
What Are Reproductive Glands?
Reproductive glands are specialized organs that produce sex hormones and, in females, eggs. In males, the primary reproductive gland is the testes, which produces testosterone and sperm. In females, the primary reproductive glands are the ovaries, which produce estrogen and progesterone while releasing eggs during ovulation. These glands work in concert with other endocrine structures, including the pituitary gland and hypothalamus, to maintain reproductive function throughout your life.
Beyond their role in reproduction, these glands influence numerous body systems. Hormones produced by reproductive glands affect bone density, cardiovascular health, mental health, and metabolism. This is why reproductive health extends far beyond fertility concerns and impacts overall quality of life.
The Role of Estrogen in Female Health
Estrogen is a primary sex hormone essential for maintaining sexual and reproductive health in females. Estrogen levels naturally fluctuate during your menstrual cycle and decline during menopause. The hormone exists in three major forms, each playing specific roles at different life stages.
Estrogen During Puberty and Development
During puberty, estrogen levels rise significantly, triggering the development of secondary sex characteristics such as breast development, increased hip width, and body composition changes. This hormonal surge marks the beginning of reproductive maturity and sets the stage for menstrual cycles to begin.
Estrogen and the Menstrual Cycle
Estrogen plays an important part in your menstrual cycle alongside hormones made in your brain (FSH and LH) and progesterone. These hormones maintain a delicate balance to keep periods regular. During the follicular phase, estrogen levels rise gradually, triggering ovulation. Estrogen peaks in the days leading up to ovulation, marking your most fertile period. At this time, estrogen thins your cervical mucus, allowing sperm to swim more easily to fertilize an egg.
Estrogen also thickens the uterine lining (endometrium) to prepare it for pregnancy. If fertilization doesn’t occur, estrogen and progesterone levels drop, signaling the body to shed the uterine lining, resulting in menstruation.
Estrogen and Sexual Function
Beyond reproduction, the presence of estrogen makes it more comfortable to have intercourse by keeping your vaginal walls thick, elastic and lubricated, reducing pain associated with penetrative sex. This aspect of estrogen’s function contributes significantly to sexual health and quality of life throughout your reproductive years.
Estrogen During Perimenopause and Menopause
Estrogen levels drop during perimenopause, the time right before menopause, which may last several years. Menopause officially begins when you haven’t had a period for 12 months, typically occurring around age 51. During this transition, the primary estrogen in your body changes from estradiol (E2) to estrone (E1).
The decline in estrogen during menopause often leads to noticeable symptoms including vaginal dryness, mood changes, night sweats, and hot flashes. Understanding these changes as normal biological processes can help you seek appropriate management strategies and maintain quality of life during this transition.
Estrogen’s Role Beyond Reproduction
While estrogen is primarily known for its reproductive functions, it affects multiple body systems. Estrogen regulates important processes in your skeletal, cardiovascular, and central nervous systems that impact your overall health. These effects include bone density maintenance, cholesterol regulation, vascular function, and cognitive health.
Research continues to uncover estrogen’s role in various health conditions. Studies have linked estrogen to certain endocrine disorders and gastrointestinal diseases, demonstrating the hormone’s far-reaching influence on overall wellness.
Estrogen in Male Health
Estrogen affects male reproductive health, too, impacting sex drive and the ability to get an erection and make sperm. While males produce significantly less estrogen than females, this hormone remains important for male reproductive function. Too little estrogen can lead to low sex drive, while excessive estrogen can cause infertility, erectile dysfunction, and gynecomastia (enlarged breasts). Males concerned about estrogen levels should consult with an endocrinologist or functional medicine specialist.
Where Estrogen Is Produced
Your ovaries make most of your estrogen during your reproductive years. Your adrenal glands (the glands on your kidneys) and adipose tissue (body fat) secrete estrogen, too. The placenta (the organ that allows nutrient-sharing between parent and fetus) secretes estrogen during pregnancy. This distributed production system ensures adequate hormone levels throughout your body and life stages.
How Estrogen Works in Your Body
Once released into the bloodstream, estrogen travels throughout your body until it reaches target tissues. There, estrogen binds to a protein, called an estrogen receptor, that gets the process moving. Estrogen receptors are located throughout your body. This receptor-based system allows estrogen to affect diverse tissues and systems simultaneously.
Progesterone and Its Importance
While estrogen receives significant attention, progesterone plays an equally important role in reproductive health. Produced primarily by the corpus luteum (remnant of the ovulated follicle), progesterone prepares and maintains the uterine lining for pregnancy. If pregnancy doesn’t occur, progesterone levels drop, triggering menstruation.
Throughout the menstrual cycle, progesterone and estrogen work synergistically. Progesterone also affects mood, sleep, and temperature regulation, contributing to overall well-being beyond reproduction.
Testosterone and Male Reproductive Health
Testosterone, produced primarily by the testes, drives male sexual development, sperm production, and sexual function. This hormone peaks during puberty, promoting muscle development, deepening of the voice, and increased body hair. Throughout adulthood, testosterone maintains sexual function, bone density, and muscle mass.
Testosterone levels naturally decline with age, typically decreasing about 1% per year after age 30. Low testosterone can result in reduced sex drive, erectile dysfunction, decreased muscle mass, and mood changes. Healthcare providers can evaluate testosterone levels through blood tests and discuss appropriate management if levels are abnormally low.
Common Reproductive Gland Conditions
Polycystic Ovary Syndrome (PCOS)
PCOS is a common endocrine disorder affecting ovarian function. It’s characterized by irregular periods, elevated androgen levels, and multiple small cysts on the ovaries. Women with PCOS often experience difficulty conceiving, irregular bleeding, and hormonal imbalances that require specialized medical management.
Hypogonadism
Low testosterone production in males can result from testicular dysfunction or problems with hormone-signaling pathways. Symptoms include reduced sex drive, erectile dysfunction, fatigue, and mood changes. Treatment options vary depending on the underlying cause.
Premature Ovarian Failure
Also called primary ovarian insufficiency, this condition involves early decline in ovarian function before age 40. It can result from genetic factors, autoimmune conditions, or unknown causes, leading to irregular periods and reduced fertility.
Hormone Imbalances
Both excessive and insufficient hormone production can create health problems. High estrogen can increase certain disease risks, while low estrogen contributes to menopausal symptoms and bone loss. Similarly, abnormal testosterone levels affect male and female health differently.
Understanding Estrogen Level Fluctuations
Estrogen levels rise and fall throughout life. The fluctuation is normal. For instance, it’s normal for estrogen levels to rise during puberty and decline as you approach menopause. It’s normal for estrogen levels to rise during ovulation so that your body can prepare itself for pregnancy. It’s normal for levels to dip during your period when the pregnancy changes aren’t needed.
However, consistently high or low levels of estrogen may signal a condition that requires your provider’s attention. If you experience symptoms suggesting hormonal imbalance, consulting with a healthcare provider is important for proper evaluation and diagnosis.
Testing Reproductive Hormone Levels
An estrogen test can measure your levels of estrone (E1), estradiol (E2) or estriol (E3). Your provider will do a simple blood draw and send it to a lab for analysis. Similarly, testosterone levels are measured through blood tests, typically taken in the morning when levels are highest.
Additional tests may include follicle-stimulating hormone (FSH) and luteinizing hormone (LH) to assess pituitary-ovarian function, or progesterone levels to confirm ovulation has occurred. Your healthcare provider will determine which tests are appropriate based on your symptoms and medical history.
Maintaining Reproductive Gland Health
Supporting reproductive gland health involves lifestyle factors and regular medical care. Maintaining a healthy weight, regular exercise, stress management, and adequate sleep all support hormonal balance. A diet rich in nutrients including vitamin D, selenium, and omega-3 fatty acids may benefit reproductive health.
Regular healthcare visits allow providers to monitor reproductive health, screen for conditions, and discuss concerns before they become significant problems. Women should have annual gynecological exams, while men should discuss reproductive health with their primary care provider or urologist.
Frequently Asked Questions
Q: At what age do reproductive glands stop functioning?
A: In females, ovarian function typically declines gradually starting in the 40s, with menopause officially occurring around age 51. In males, testosterone production gradually decreases with age but typically continues throughout life.
Q: Can reproductive hormone imbalances be treated?
A: Yes, depending on the underlying cause. Treatment options may include lifestyle modifications, medications, hormone replacement therapy, or procedures. Your healthcare provider can recommend appropriate options based on your specific situation.
Q: How do reproductive glands affect non-reproductive aspects of health?
A: Reproductive hormones influence bone density, cardiovascular health, mood, metabolism, and cognitive function. This is why reproductive health impacts overall well-being.
Q: Should I have my hormone levels tested?
A: If you’re experiencing symptoms suggesting hormonal imbalance, such as irregular periods, mood changes, or sexual dysfunction, discuss testing with your healthcare provider. Routine screening depends on age, symptoms, and medical history.
References
- Estrogen: Hormone, Function, Levels & Imbalances — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/body/22353-estrogen
- Female Reproductive Health — Johns Hopkins Medicine. https://www.hopkinsmedicine.org
- Endocrine System Overview — National Institutes of Health (NIH). https://www.nih.gov
- Reproductive Endocrinology: Clinical Guide — American College of Obstetricians and Gynecologists (ACOG). https://www.acog.org
- Male Reproductive Health — American Urological Association. https://www.auanet.org
Read full bio of medha deb