Rheumatoid Arthritis: In-Depth Guide to Causes, Symptoms & Treatment
Comprehensive overview of RA: understanding causes, symptoms, conventional treatments, and complementary health approaches.

Understanding Rheumatoid Arthritis
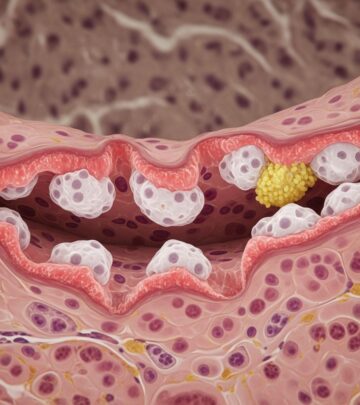
Rheumatoid arthritis (RA) is a chronic disease characterized by pain, swelling, and stiffness in the joints that can significantly impact daily functioning and quality of life. This autoimmune condition occurs when the immune system mistakenly attacks the synovium, the membrane lining the joints, causing inflammation and progressive joint damage. Unlike osteoarthritis, which results from wear and tear, RA is a systemic condition that can affect multiple body systems beyond the joints. The disease is more prevalent in women than men and typically begins in middle age, though it can develop at any age. Early diagnosis and aggressive treatment are crucial to preventing permanent joint damage, disability, and long-term complications.
What Causes Rheumatoid Arthritis?
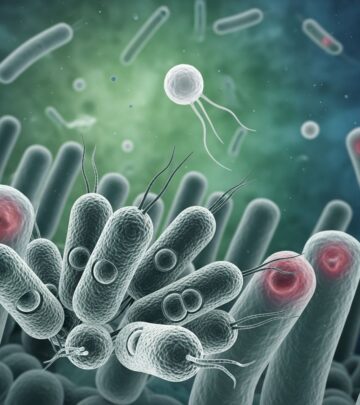
Rheumatoid arthritis develops when the body’s immune system malfunctions and attacks its own cells. In a healthy immune system, white blood cells protect the body from bacteria, viruses, and other harmful invaders. However, in people with RA, the immune system becomes confused and targets the synovial lining of joints, treating the body’s own cells as foreign threats. This autoimmune attack triggers the release of inflammatory chemicals that cause the synovium to thicken, become inflamed, and produce excess fluid, leading to pain, swelling, and reduced joint mobility.
Several risk factors contribute to the development of RA:
– Age: The condition can develop at any age but is more common in middle-aged and older adults- Gender: Women are two to three times more likely to develop RA than men- Genetics: Family history and certain genetic markers increase susceptibility- Environmental factors: Cigarette smoking, air pollutants, and occupational exposures have been linked to increased RA risk- Hormonal factors: Changes in hormone levels may influence disease development
Recognizing Symptoms of Rheumatoid Arthritis
The symptoms of RA typically develop gradually over weeks to months, though in some cases they can appear suddenly. Recognizing these early warning signs is essential for prompt diagnosis and treatment initiation.
Common Symptoms Include:
– Joint pain, tenderness, swelling, or stiffness persisting for six weeks or longer- Morning stiffness lasting 30 minutes or more- Involvement of multiple joints simultaneously- Symmetric joint involvement (affecting the same joints on both sides of the body)- Small joints affected first, particularly in the wrists, hands, and feet- Fatigue and general malaise- Low-grade fever- Loss of appetite- Red, warm, or tender joint areas
Early symptoms may be mild and intermittent, making diagnosis challenging. However, untreated RA can progress to affect larger joints and eventually spread to other body systems, including the eyes, heart, lungs, and circulatory system.
How Rheumatoid Arthritis Affects the Body
RA’s systemic nature means it can damage multiple organs and tissues beyond the joints. Progressive joint inflammation leads to cartilage and bone destruction, causing deformities and permanent loss of function. The disease can also cause:
– Lung disease and scarring (pulmonary fibrosis), leading to shortness of breath- Heart inflammation (myocarditis) and damage to the heart muscle- Blood vessel inflammation (vasculitis), affecting nerves, skin, and other organs- Anemia (lower than normal red blood cell count)- Eye inflammation and vision problems- Rheumatoid nodules (firm lumps under the skin)
Diagnosis of Rheumatoid Arthritis
Accurate diagnosis requires a comprehensive evaluation combining medical history, physical examination, and laboratory tests.
Diagnostic Process:
Medical History
Your healthcare provider will ask detailed questions about joint symptoms, including onset, duration, severity, and aggravating factors. They will also inquire about family history of RA or other autoimmune diseases and any systemic symptoms like fatigue or fever.
Physical Examination
The doctor will examine your joints for tenderness, swelling, warmth, and range of motion limitations. They will assess for rheumatoid nodules (bumps under the skin) and may check for low-grade fever.
Laboratory Tests
Blood tests are essential for RA diagnosis and include:
– Erythrocyte Sedimentation Rate (ESR): Measures inflammation in the blood- C-Reactive Protein (CRP): Another inflammation marker; elevated levels suggest active disease- Rheumatoid Factor (RF): An antibody found in approximately 80% of people with RA- Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibodies: Present in 60-70% of RA patients; highly specific for the disease
Imaging Studies
X-rays or other imaging may be used to assess joint damage and monitor disease progression over time.
Conventional Treatment Approaches
While there is no cure for rheumatoid arthritis, early and aggressive treatment can reduce inflammation, relieve symptoms, prevent joint damage, and improve overall functioning. Treatment strategies are individualized based on disease severity, patient age, overall health, and response to therapy.
Treatment Goals
The primary objectives of RA treatment are to:
– Stop inflammation or reduce it to the lowest possible level (achieve remission)- Relieve pain and other symptoms- Prevent joint and organ damage- Improve function and quality of life- Reduce long-term complications and disability
Pharmacological Treatments
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are the cornerstone of RA treatment and work by slowing disease progression and preventing joint destruction. These drugs can induce remission when started early. Conventional synthetic DMARDs include methotrexate, sulfasalazine, and leflunomide. Biologic DMARDs, which target specific immune system components, have revolutionized RA treatment and include TNF inhibitors, IL-6 inhibitors, and B-cell inhibitors.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs reduce pain and inflammation but do not slow disease progression. They are typically used as adjuncts to DMARDs for symptom management.
Corticosteroids
Low-dose corticosteroids reduce inflammation and are often used short-term during flares or as bridge therapy while waiting for DMARDs to take effect.
Treatment Strategies
Modern RA management follows specific strategies:
– Early, Aggressive Treatment: Initiating therapy quickly to suppress inflammation rapidly- Treat-to-Target (T2T): Working toward remission or low disease activity with specific treatment goals- Tight Control: Maintaining inflammation at the lowest possible level through regular monitoring and medication adjustments- Regular Monitoring: Frequent follow-up visits to assess treatment efficacy, monitor for joint damage, and manage side effects
Complementary Health Approaches for Rheumatoid Arthritis
Complementary approaches can play a supportive role in RA management when used alongside conventional medical treatment. These approaches are classified by their therapeutic delivery method:
Nutritional Approaches
Nutritional complementary therapies include special diets, dietary supplements, herbs, probiotics, and microbial-based therapies. Some research suggests that anti-inflammatory diets rich in omega-3 fatty acids may help reduce RA symptoms, though more rigorous studies are needed. Patients interested in dietary modifications should consult with their healthcare provider before making significant changes.
Psychological Approaches
Psychological complementary methods include meditation, hypnosis, music therapy, and relaxation techniques. These approaches may help manage pain perception, reduce stress, and improve overall well-being.
Relaxation Techniques
Autogenic training, biofeedback, and other relaxation techniques have been studied in RA patients with some promising results. However, the amount of research remains limited, preventing definitive conclusions about efficacy. Relaxation techniques generally have minimal side effects, though rare harmful effects have been reported in people with serious physical or mental health conditions. These techniques can be safely explored as complementary approaches to conventional treatment.
Physical Approaches
Physical complementary therapies include acupuncture, massage therapy, and spinal manipulation. Some evidence suggests these modalities may provide temporary pain relief and improved function when combined with conventional treatment.
Combined Approaches
Several therapies combine psychological and physical components:
Yoga and Tai Chi
Yoga and tai chi combine gentle movement, breathing, and mindfulness. Clinical practice guidelines from the American College of Rheumatology and the Arthritis Foundation strongly recommend tai chi for managing joint pain and stiffness. Yoga is conditionally recommended for individuals with knee OA and may benefit RA patients as well. These practices improve flexibility, strengthen supporting muscles, enhance balance, and reduce stress.
Dance Therapy
Dance therapy combines physical movement with emotional expression and music, potentially improving mood, function, and pain management.
Art Therapy
Art-based interventions may reduce stress and improve psychological well-being, indirectly supporting physical health.
Psychological and Nutritional Combinations
Mindful eating combines nutritional awareness with psychological mindfulness, promoting healthier food choices and stress reduction through conscious eating practices.
Lifestyle Management for Rheumatoid Arthritis
Comprehensive RA management requires attention to multiple lifestyle factors:
Exercise and Physical Activity
Regular aerobic exercise and strength training help maintain joint function, improve overall fitness, and reduce disease activity. Exercise should be tailored to individual capacity and performed during periods of lower inflammation.
Weight Management
Maintaining a healthy weight reduces stress on affected joints and may improve treatment response. Excess body weight can increase inflammation markers and worsen symptoms.
Patient Education
Understanding RA, its progression, and treatment options empowers patients to actively participate in disease management and make informed healthcare decisions.
Rest and Activity Balance
Appropriate rest during flares and pacing of activities prevents joint overuse while maintaining function during periods of disease control.
When to Seek Medical Attention
Consult a healthcare provider if you experience:
– Joint pain, swelling, or stiffness lasting more than six weeks- Morning stiffness lasting 30 minutes or longer- Multiple joints affected simultaneously- Persistent fatigue unexplained by other causes- New or worsening joint symptoms- Side effects from current medications
Frequently Asked Questions About Rheumatoid Arthritis
Q: Is rheumatoid arthritis curable?
A: Currently, there is no cure for RA. However, early treatment with DMARDs can induce remission, where symptoms disappear or become minimal, allowing patients to lead active, functional lives.
Q: Can complementary approaches replace conventional RA treatment?
A: No. Complementary approaches should be used alongside, not instead of, conventional medical treatment. DMARDs and other medications are essential for preventing joint damage. Complementary therapies can provide additional symptom relief and improve well-being.
Q: How quickly does RA develop?
A: RA typically develops gradually over weeks to months, though onset can occasionally be sudden. Prompt recognition of early symptoms and initiation of treatment are critical for preventing permanent joint damage.
Q: Can RA affect organs other than joints?
A: Yes. RA is a systemic disease that can affect the heart, lungs, eyes, blood vessels, and other organs. This is why comprehensive medical management and regular monitoring are essential.
Q: Are there lifestyle modifications that help manage RA?
A: Yes. Regular exercise, weight management, stress reduction, adequate rest, and patient education all support RA management and improve outcomes when combined with medical treatment.
Q: What is remission in RA?
A: Remission refers to a state where RA symptoms are minimal or absent, inflammation is controlled, and no new joint damage is occurring. This is the treatment goal and is increasingly achievable with modern medications and treatment strategies.
Conclusion
Rheumatoid arthritis is a serious chronic autoimmune disease requiring comprehensive medical management. Early diagnosis and aggressive treatment with disease-modifying drugs are essential for preventing permanent joint damage and disability. While no cure exists, modern treatment approaches enable many patients to achieve remission or low disease activity, maintaining function and quality of life. Complementary health approaches, including exercise, relaxation techniques, yoga, and tai chi, can provide valuable additional support when integrated with conventional treatment. Patients should work closely with their healthcare team to develop individualized treatment plans that address their specific needs and goals.
References
- Rheumatoid Arthritis: In Depth — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024. https://www.nccih.nih.gov/health/rheumatoid-arthritis-in-depth
- Rheumatoid Arthritis: Causes, Symptoms, Treatments and More — Arthritis Foundation. 2024. https://www.arthritis.org/diseases/rheumatoid-arthritis
- Rheumatoid Arthritis: A Brief Overview of the Treatment — PubMed Central, National Center for Biotechnology Information. 2019. https://pmc.ncbi.nlm.nih.gov/articles/PMC6422329/
- Rheumatoid Arthritis – Diagnosis and Treatment — Mayo Clinic. 2024. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653
- Arthritis and Complementary Health Approaches — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024. https://www.nccih.nih.gov/health/providers/digest/arthritis-and-complementary-health-approaches
- 6 Things To Know About Complementary Health Approaches for Rheumatoid Arthritis — National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health. 2024. https://www.nccih.nih.gov/health/tips/6-things-to-know-about-complementary-health-approaches-for-rheumatoid-arthritis
- Rheumatoid Arthritis Clinical Practice Guidelines — American College of Rheumatology. 2024. https://rheumatology.org/rheumatoid-arthritis-guideline
Read full bio of Sneha Tete