Scabies CME
Comprehensive CME on scabies: aetiology, diagnosis, management, and institutional control strategies for healthcare professionals.

Scabies
Scabies is a common ectoparasitic infestation affecting all age groups and regions worldwide, responsible for significant morbidity due to intense pruritus and secondary bacterial infections.
What is scabies?
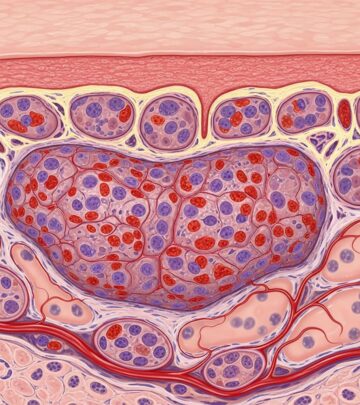
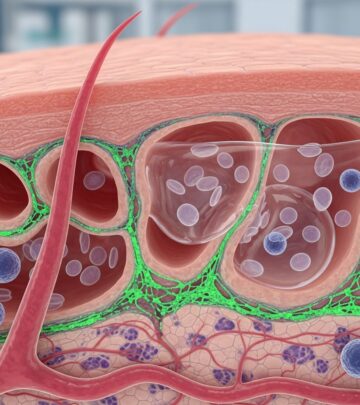
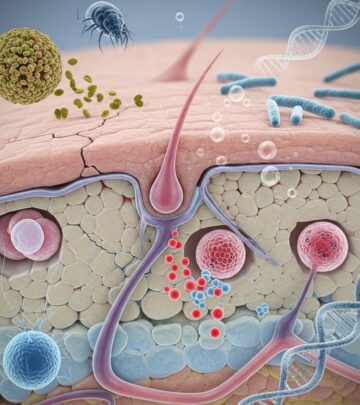
Scabies is an infestation of the skin by the human itch mite Sarcoptes scabiei var. hominis. The female mite measures approximately 0.3–0.4 mm, burrows within the stratum corneum, and deposits eggs and faecal pellets (scybala) that provoke a delayed type IV hypersensitivity reaction, manifesting as severe pruritus and characteristic lesions. Transmission primarily occurs through prolonged skin-to-skin contact, with fomite transmission rare in classic cases but significant in crusted scabies.
Who gets scabies?
Scabies affects individuals across all demographics, with higher incidence in crowded conditions, low socioeconomic settings, children, and institutional environments such as nursing homes. In New Zealand, it disproportionately impacts Māori and Pacific peoples in areas of deprivation. Immunosuppressed patients, including those with HIV, elderly debilitated individuals, and those on corticosteroids, are prone to crusted (Norwegian) scabies.
Causes
The causative agent is Sarcoptes scabiei var. hominis, a mite specific to humans. After transmission via close contact, fertilised females burrow into the epidermis, laying 2–3 eggs daily over 4–5 weeks before dying. Sensitisation occurs 4–6 weeks post-infestation in naive hosts, leading to symptoms; reinfestation elicits symptoms within 1–4 days. Crusted scabies arises in immunocompromised hosts due to failure of immune clearance, resulting in hyperinfestation with millions of mites.
Clinical features
Classic scabies presents 4–6 weeks post-infestation with intense nocturnal pruritus and an erythematous papular rash, often excoriated. Pathognomonic linear burrows (2–15 mm) are seen on finger webs, wrists, elbows, axillae, umbilicus, and genitalia in adults; in infants, palms, soles, and scalp are involved.
Nodular scabies features persistent pruritic nodules (2–20 mm) in genital and axillary areas due to hypersensitivity.
Crusted scabies manifests as widespread hyperkeratotic plaques, nail dystrophy, and thick crusts, especially on palms, soles, and scalp, with minimal pruritus.
| Classic Scabies | Nodular Scabies | Crusted Scabies |
|---|---|---|
| Burrows, papules, intense itch | Inflammatory nodules in folds/genitals | Hyperkeratosis, thousands of mites, scalp involvement |
| 10–15 mites/skin | Persistent post-treatment nodules | Highly contagious, immunocompromised |
Complications
Chronic excoriation leads to impetiginisation with Staphylococcus aureus or Streptococcus pyogenes, causing cellulitis, abscesses, or post-streptococcal glomerulonephritis. In New Zealand, scabies links to acute rheumatic fever via group A streptococcal pyoderma. Hypersensitivity reactions include urticaria, nummular eczema, and vasculitis. Crusted scabies risks severe secondary bacteraemia.
Diagnosis
Diagnosis relies on history (pruritus in contacts), examination (burrows, distribution), and dermoscopy/microscopy.
- Dermoscopy: Delta-wing jet sign at burrow end.
- Microscopy: Scrape burrows/nails for mites, eggs, scybala. In infants, scrape subungual debris.
- Adhesive tape test: Effective for crusted cases.
- Biopsy: Shows intraepidermal burrow with mite/ova, spongiosis, eosinophilic infiltrate.
Burrow ink test: Ink applied to suspect burrow, wiped, linear track remains.
Differential diagnoses
- Atopic dermatitis, contact dermatitis, papular urticaria.
- Bullous pemphigoid (urticarial phase mimics).
- Fibreglass dermatitis (irritant, fewer eosinophils).
- Pruritus in pregnancy, senile pruritus.
Investigations
Microscopy remains gold standard, though low yield (10–20%). PCR emerging for mite DNA detection. Histopathology shows wedge-shaped infiltrate with eosinophils, mites in stratum corneum.
Treatment
Treat all household/close contacts simultaneously, regardless of symptoms.
Topical scabicides
- Permethrin 5% cream: First-line; apply head-to-toe, leave 8–14 hours, repeat day 7. Safe in pregnancy, children >2 months.
- Benzyl benzoate 25%: Alternative, odorous, irritant.
- Sulphur ointment 5–10%: For infants <2 months, pregnant women.
Oral ivermectin
200 µg/kg, repeat day 7–14; ideal for crusted scabies, outbreaks, poor compliance. Two doses suffice for classic; crusted requires 3–7 doses + keratolytics.
Crusted scabies
Combination: Oral ivermectin (days 1,2,8) + permethrin daily ×7 + keratolytics (salicylic acid 5%) + antibiotics if infected. Isolation until negative scrapings.
Post-scabies syndrome
Pruritus persists 2–4 weeks: Emollients, potent topical steroids, oral antihistamines. Nodular: Intralesional steroids.
Treatment failure causes: Incorrect application, resistance, reinfestation, insufficient contacts treated.
Prevention of spread
- Machine wash/decontaminate bedding/clothing at 60°C.
- Vacuum furnishings.
- No shared towels.
Control of epidemics of institutional scabies
Institutional outbreaks require cohorting suspects, tracing contacts (back 8 weeks), treating all regardless of symptoms.
- Case ascertainment: Examine high-risk (elderly, disabled).
- Containment: Isolate crusted cases until non-infectious.
- Mass treatment: Ivermectin preferred for logistics.
- Environment: Hot wash linens, disinfect.
- Follow-up: Repeat treatment week 2, monitor 4–6 weeks.
Success metrics: No new cases >6 weeks.
Information for patients
See patient information leaflets on scabies management, burrow identification, treatment adherence, contact treatment, and preventing reinfestation.
Frequently Asked Questions
Q: How soon after contact does scabies itch?
A: 4–6 weeks first infestation; 1–4 days if previously exposed.
Q: Can scabies affect the face?
A: Rarely in adults; common in infants, crusted scabies.
Q: Is ivermectin safe in pregnancy?
A: Category C; prefer topical permethrin.
Q: How to confirm burrow on exam?
A: Linear white-grey track 2–15 mm with delta sign dermoscopically.
Q: Treatment for nursing home outbreak?
A: Mass ivermectin dosing, environmental decontamination, repeat week 2.
References
- Crusted scabies – DermNet — DermNet NZ. 2023. https://dermnetnz.org/topics/crusted-scabies
- Scabies – Arthropod infestations – DermNet — DermNet NZ. 2023. https://dermnetnz.org/cme/arthropods/scabies-cme
- Scabies: diagnosis and management — bpac.org.nz. 2022-10. https://bpac.org.nz/2022/docs/scabies.pdf
- Scabies – StatPearls — NCBI Bookshelf. 2023-07-17. https://www.ncbi.nlm.nih.gov/books/NBK544306/
- Scabies pathology – DermNet — DermNet NZ. 2023. https://dermnetnz.org/topics/scabies-pathology
- Scabies: Pictures, causes, treatment — Medical News Today. 2023. https://www.medicalnewstoday.com/articles/16961
- Scabies: Diagnosis and Treatment — DermNet NZ. 2023. https://dermnetnz.org/topics/scabies
Read full bio of Sneha Tete