Shigella Infection: Symptoms, Treatment, and Prevention
Complete guide to shigella infection: Learn about symptoms, transmission, and effective prevention strategies.
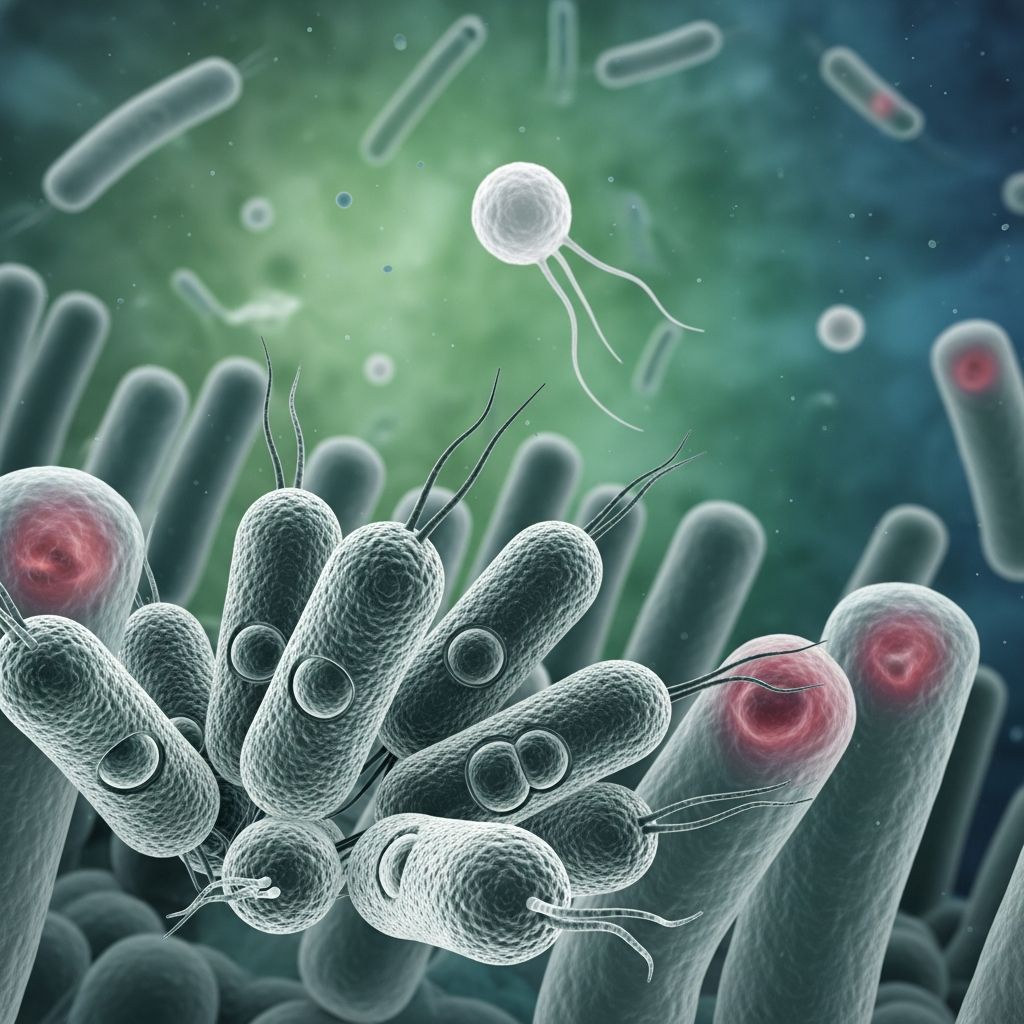
What Is Shigella Infection?
Shigella infection, also called shigellosis, is an acute diarrheal disease caused by bacteria called Shigella. This highly contagious infection belongs to a group of gram-negative bacteria and can easily spread from person to person, making it a significant public health concern. Shigellosis is an important cause of diarrheal disease worldwide, most commonly affecting children under 5 years old.
The disease is caused by four main species of Shigella bacteria: S. sonnei, S. flexneri, S. boydii, and S. dysenteriae. In the United States alone, there are approximately 500,000 cases of shigellosis reported each year. The infection typically presents as a mild, self-limited diarrheal illness, though severity can vary depending on the infecting species and the strength of a person’s immune system.
How Shigella Spreads
Shigella bacteria are remarkably contagious and require only a minimal number of organisms to cause infection. As few as 10 organisms are needed to cause disease, making it one of the most easily transmissible gastrointestinal pathogens. Understanding transmission routes is crucial for prevention efforts.
The primary transmission method is through fecal-oral contact. People can contract shigellosis when they put something in their mouths or swallow something that has come into contact with the stool of a person who is sick with shigellosis. Shigella germs survive in the stool of infected individuals while they have diarrhea and for up to 1–2 weeks after diarrhea has resolved.
Additional transmission routes include:
- Contaminated food or water
- Close personal contact with an infected individual
- Poor hand hygiene after using the toilet
- Direct contact in crowded, unsanitary conditions
Shigella bacteria are particularly acid-resistant and survive passage through the stomach to access the intestines, which explains why such a small infective dose is necessary to establish infection.
Symptoms and Signs of Shigella Infection
The symptoms of shigella infection typically begin within 1 to 4 days following exposure to the bacteria. Most people experience a consistent pattern of gastrointestinal symptoms, though severity varies among individuals.
Common symptoms include:
- Diarrhea (often bloody and mucoid)
- Severe abdominal pain and cramping
- Fever
- A strong, painful urge to pass stool even when bowels are empty
- Nausea and vomiting
The bloody and often mucoid diarrhea is the main symptom of shigellosis and is characteristic of the infection. In most immunocompetent individuals, the disease course is self-limited and lasts approximately 5 to 7 days. However, the disease is typically more severe and prolonged in young children, older adults, international travelers, individuals living with HIV, and those living in crowded, unsanitary conditions.
Who Is at Higher Risk?
Certain populations face increased risk of contracting shigella infection or experiencing severe disease. Understanding these risk factors can help identify vulnerable individuals who may require more aggressive medical management.
High-risk populations include:
- Children under 5 years old
- Older adults and elderly individuals
- People living with HIV or other immunocompromised conditions
- Malnourished or chronically ill patients
- Individuals in crowded or unsanitary living conditions
- International travelers to endemic areas
- Men who have sex with men
- People with poor access to clean water and hygiene facilities
These groups are more susceptible to severe complications, including hemolytic-uremic syndrome and postreactive arthritis, necessitating prompt medical attention and targeted treatment strategies.
How Shigella Infection Develops in the Body
Understanding the pathophysiology of shigella infection explains why symptoms are so specific and why the disease can be so uncomfortable. The infection process involves multiple stages of bacterial invasion and inflammatory response.
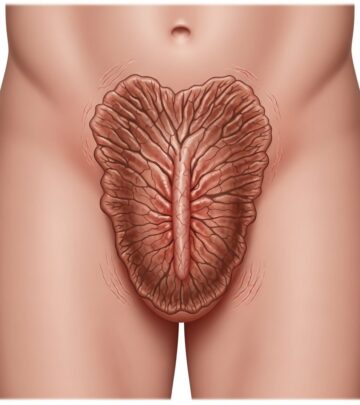
After ingestion, Shigella bacteria multiply in the small intestine and then enter the colon, where the colonic mucosa becomes the site of pathogenic events. The bacteria secrete virulence factors that cause extreme inflammation and mediate enterotoxic effects, allowing colonization and invasion of the colonic epithelium.
Shigella bacteria produce up to 3 different enterotoxins, including ShET1, ShET2, and Shiga toxin. These enterotoxins create ulcers in the intestinal mucosa, particularly the colon, and add a hemorrhagic component to the infection. The resulting inflammatory response damages the epithelium, degrades the epithelial barrier, and leads to diarrhea.
The classic dysentery syndrome of symptomatic shigellosis comprises small-volume stools containing leukocytes from the inflammatory response, erythrocytes from intestinal ulceration, and bacteria themselves. This explains the characteristic bloody, mucoid appearance of the stool in shigella infections.
Diagnosis of Shigella Infection
Proper diagnosis is essential for confirming shigella infection and guiding appropriate treatment decisions. Healthcare providers use several diagnostic approaches to identify the infection and assess disease severity.
Primary diagnostic tests include:
- Stool microscopy, culture, and sensitivity testing — The gold standard for diagnosis, allowing identification of the Shigella species and determination of antibiotic susceptibility
- Complete blood count (CBC) — To assess for leukocytosis and other blood abnormalities
- Serum BUN and creatinine — To evaluate kidney function, particularly important in severe cases
Additional tests may be considered in specific situations:
- Shigella serotyping to identify the specific strain
- Peripheral blood smear for detailed cell analysis
- Abdominal X-ray if complications are suspected
- Flexible sigmoidoscopy in severe or prolonged cases
Antimicrobial susceptibility testing is critical to ensure appropriate therapeutic selection, as antibiotic resistance is rising within the Shigella genus, and extensively drug-resistant strains have been identified.
Treatment Options for Shigella Infection
Treatment approaches vary depending on disease severity and individual risk factors. While many cases resolve without medication, others require medical intervention to prevent complications and reduce transmission.
Supportive Care
Mild cases typically require only supportive care, including adequate hydration and rest. Maintaining fluid intake is crucial to prevent dehydration, which is the primary concern in diarrheal illnesses.
Antibiotic Therapy
Antibiotics may be required to shorten the duration of illness, reduce bacterial shedding, or prevent complications, particularly in individuals at increased risk for severe disease. Empiric antibiotics are specifically recommended for:
- Children and adults with severe disease
- Older adults
- Malnourished or chronically ill patients
- Individuals in institutional settings where spread must be reduced
However, antibiotic resistance is rising significantly within the Shigella genus, and extensively drug-resistant shigellae have been identified in recent years. Therefore, antimicrobial susceptibility testing is highly recommended to guide antibiotic selection, as drug resistance may vary regionally.
Treatment decisions should be made in consultation with healthcare providers who can consider local resistance patterns and individual patient factors.
Prevention Strategies
Prevention is paramount in controlling shigella infection, particularly in institutions and high-risk settings. Basic hygiene measures and environmental controls are the cornerstone of prevention efforts.
Essential Prevention Measures
- Hand washing — Wash hands thoroughly with soap and clean water after using the toilet, before eating, and when caring for children or sick individuals
- Access to clean water — Ensure safe drinking water and proper sanitation facilities
- Food safety — Cook food thoroughly, especially in institutions and camps
- Environmental sanitation — Maintain proper hygiene in crowded conditions and during natural disasters
- Personal hygiene — Avoid sharing personal items, towels, or eating utensils with infected individuals
Vaccination development is ongoing, with vaccines in developmental stages that may provide additional protection in the future.
Complications of Shigella Infection
While most cases resolve without complications, severe infections can lead to serious health consequences. Certain Shigella species, particularly S. dysenteriae, pose greater risk.
Potential complications include:
- Hemolytic-uremic syndrome (HUS) — A serious complication associated with S. dysenteriae type 1 due to its production of Shiga toxin
- Postreactive arthritis — Joint inflammation following infection
- Severe dehydration — Particularly dangerous in young children and elderly individuals
- Toxic megacolon — Severe colonic dilation in rare cases
- Intestinal perforation — An uncommon but serious complication
Prompt diagnosis and appropriate treatment significantly reduce the risk of these complications.
Prognosis and Recovery
The outlook for shigella infection is generally favorable when managed appropriately. Shigellosis is usually a self-limited disease that resolves within 5 to 7 days. In more severe cases where patients seek medical care, the diagnosis should be included in the differential diagnosis, and treatment should be initiated promptly.
If shigellosis is diagnosed and treated on time, the prognosis is good, and patients usually recover without long-term sequelae. Immunity can occur after a Shigella infection and appears to be serogroup-specific, meaning prior infection may provide some protection against the same bacterial strain in the future.
However, reinfection with different Shigella species or strains is possible, reinforcing the importance of ongoing prevention measures.
Frequently Asked Questions About Shigella
Q: How quickly do shigella symptoms appear?
A: Symptoms typically begin within 1 to 4 days following exposure to Shigella bacteria. Some sources indicate onset can occur as early as 1–2 days after contact with infected individuals.
Q: Can shigella infection be fatal?
A: While shigella infection is typically self-limited and resolves without treatment in most immunocompetent individuals, severe cases—particularly in young children, elderly people, or those with S. dysenteriae infection—can lead to serious complications. Deaths are rare in developed countries with access to modern medical care but can occur in areas with limited healthcare resources.
Q: How long is someone contagious with shigella?
A: People shed Shigella bacteria in their stool while experiencing diarrhea and for up to 1–2 weeks after the diarrhea has resolved, making them potentially contagious throughout this entire period.
Q: Should I take antibiotics for shigella?
A: Not all cases require antibiotics. Treatment depends on disease severity and individual risk factors. Antibiotics are typically recommended for severe disease, high-risk individuals (young children, elderly, immunocompromised), and those in institutional settings. Your healthcare provider can determine the best approach for your situation.
Q: Is there a vaccine for shigella?
A: Currently, no shigella vaccine is available for routine use. However, vaccines are in developmental stages and may provide protection in the future.
Q: Can I get shigella from swimming?
A: Yes, shigella can spread through contaminated water. Swimming in contaminated water sources or inadequately chlorinated pools poses a risk, making water safety an important prevention measure.
References
- Shigellosis — StatPearls, National Center for Biotechnology Information (NCBI Bookshelf), National Institutes of Health. 2025-08-10. https://www.ncbi.nlm.nih.gov/books/NBK482337/
- Shigellosis — California Department of Public Health (CDPH). 2024. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Shigellosis.aspx
- Shigella Infection – Symptoms, Diagnosis and Treatment — BMJ Best Practice. 2025. https://bestpractice.bmj.com/topics/en-us/1174
- Shigella Prevention and Control Toolkit — Centers for Disease Control and Prevention (CDC). 2021-03. https://www.cdc.gov/shigella/pdf/Shigella-prevention-and-control-toolkit-508.pdf
- Shigella — Head Start. U.S. Department of Health & Human Services. https://headstart.gov/physical-health/article/shigella
Read full bio of medha deb