Sjögren-Larsson Syndrome
Rare genetic disorder causing ichthyosis, spasticity, and intellectual disability: symptoms, causes, diagnosis, and management.

Author: A/Prof Marius Rademaker, Dermatologist, Hamilton, New Zealand. Reviewed/edited July 2024.
What is Sjögren-Larsson syndrome?
SjögrenLarsson syndrome (SLS; MIM #270200) is a rare autosomal recessive neurocutaneous disorder characterised by the clinical triad of non-scaly ichthyosis, spastic diplegia or paraparesis, and intellectual disability. It is caused by mutations in the ALDH3A2 gene, resulting in a deficiency of fatty aldehyde dehydrogenase (FALDH). This leads to accumulation of toxic fatty aldehydes and alcohols, primarily affecting the skin, central nervous system (CNS), and eyes.
The disorder was first described in 1957 by Swedish physicians Torsten Sjögren and Tage Larsson in 28 related patients from Västernorrland County, Sweden. Worldwide incidence is unknown but estimated at 1:250,000 in the general population, higher in isolated populations such as in northern Sweden (1:20,0001:40,000).
Who gets Sjögren-Larsson syndrome?
SLS affects males and females equally. Symptoms are evident from birth or early infancy. Preterm birth is common. It occurs worldwide but founder mutations are reported in Sweden (c.1234G>A), Saudi Arabia (c.771_772insG), and among Portuguese gypsies (c.685C>T).
What causes Sjögren-Larsson syndrome?
SLS results from biallelic pathogenic variants in ALDH3A2 on chromosome 17p11.2, encoding FALDH. This enzyme oxidises long-chain lipid aldehydes to fatty acids and fatty alcohols to fatty aldehydes, crucial for lipid metabolism and cell membrane integrity.
Over 100 mutations identified, including missense, nonsense, frameshift, splice-site, and large deletions. Most are private; no clear genotypephenotype correlation. FALDH deficiency causes:
- Skin: Impaired lamellar granule function and elta-hydroxylation of sphingolipids, leading to ichthyosis.
- CNS: White matter lipid toxicity causing demyelination, gliosis, and spasticity.
- Eyes: Retinal crystalline maculopathy from lipid accumulation.
What are the clinical features of Sjögren-Larsson syndrome?
Skin features
Ichthyosis appears in the first weeksmonths as erythema and fine scaling, evolving into yellow-brown, plate-like hyperkeratosis sparing flexures. Unique features include:
- Crystalline or translucency of skin (“retinal glint“).
- Pruritus (itch) in 50%.
- Non-scaly ichthyosis (unlike typical ichthyosis where scales flake off).
Skin on face, palms, and soles usually spared. Ectropion rare.
Neurological features
Onset by age 12 years with delayed motor milestones due to spastic diplegia/paraparesis (lower limbs > upper). Features include hyperreflexia, clonus, contractures, and scissoring gait. Half require wheelchairs; others use aids.
- Intellectual disability: Mildmoderate (developmental age 56 years); speech dyspraxia/dysarthria common.
- Seizures: 40% have epilepsy.
- Other: Microcephaly, kyphoscoliosis, peripheral neuropathy.
Eye features
Present in >90%; bilateral crystalline maculopathy (glistening white/yellow dots in retina/macula). Causes nystagmus, photophobia, strabismus; vision mildly impaired. Optic atrophy in some.
Other features
- Short stature, dental anomalies (spaced teeth, enamel hypoplasia).
- Hyperkeratotic plaques on elbows/knees.
- Rare: Cardiac arrhythmias, nephropathy.


How is Sjögren-Larsson syndrome diagnosed?
Clinical triad + supportive tests. Diagnosis confirmed by:
- Genetic testing: ALDH3A2 variants (95% detection rate).
- Enzyme assay: Reduced FALDH in fibroblasts (gold standard).
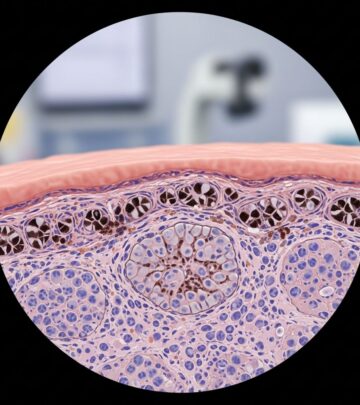
- Skin biopsy: Acanthosis, hyperkeratosis, reduced lamellar bodies.
Differential diagnosis: Includes other ichthyosis syndromes (e.g., Netherton, peeling skin), leukodystrophies, cerebral palsy mimics.
| Feature | SLS | Refsum Disease | KID Syndrome |
|---|---|---|---|
| Ichthyosis onset | Neonatal | Later | Neonatal |
| Spasticity | Yes | No | No |
| Retinal crystals | Yes | RP | No |
What is the treatment for Sjögren-Larsson syndrome?
Symptomatic and supportive; no cure. Multidisciplinary care essential.
Skin care
- Daily emollients (e.g., white soft paraffin).
- Keratolytics: urea 1020%, lactic acid, salicylic acid.
- Topical retinoids (tazarotene) for hyperkeratosis.
- Antihistamines/avoid triggers for itch.
Neurological management
- Physiotherapy, orthotics, botulinum toxin for spasticity.
- Baclofen, diazepam, gabapentin.
- Antiepileptics (e.g., valproate).
- Speech/occupational therapy.
Ocular care
Regular ophthalmology; sunglasses for photophobia.
Experimental
Zileuton (5-lipoxygenase inhibitor) reduced leukotriene B4 in trials, improving ichthyosis. Gene therapy preclinical.
What is the prognosis for Sjögren-Larsson syndrome?
Normal lifespan; symptoms non-progressive after childhood. Main issues: mobility, quality of life. Early intervention improves outcomes. Average lifespan ~15 years males, 26 females (older data).
Frequently asked questions about Sjögren-Larsson syndrome
What is the inheritance pattern of SLS?
Autosomal recessive: both parents carriers (25% risk per pregnancy).
Can SLS be prevented?
Genetic counselling, prenatal testing for known mutations.
Is there a cure?
No, but management improves symptoms significantly.
Does SLS affect life expectancy?
Usually normal with good care; complications rare.
How common is SLS?
<1:250,000; higher in certain populations.
References
- Sjögren-Larsson Syndrome: A Comprehensive Guide — MapMyGenome. 2023. https://learn.mapmygenome.in/resourceguide/Rarediseaseresources/sj%C3%B6gren-larsson-syndrome
- Sjögren-Larsson Syndrome — NORD (National Organization for Rare Disorders). 2024-01-15. https://rarediseases.org/rare-diseases/sjogren-larsson-syndrome/
- Sjögren-Larsson syndrome — MedlinePlus Genetics (U.S. National Library of Medicine). 2023-11-01. https://medlineplus.gov/genetics/condition/sjogren-larsson-syndrome/
- Sjogren-Larsson Syndrome: Mechanisms and Management — PMC (NCBI). 2020-01-14. https://pmc.ncbi.nlm.nih.gov/articles/PMC6954685/
- Sjögren-Larsson syndrome — Alex TLC (The Leukodystrophy Charity). 2024. https://alextlc.org/condition/sjogren-larsson-syndrome/
Read full bio of medha deb