Skin Problems in Childcare Staff: Risks and Prevention
Understanding occupational skin diseases affecting childcare workers and prevention strategies.

Skin Problems in Childcare Staff
Childcare work represents a significant employment sector worldwide, with numbers expected to expand considerably, particularly in developing countries as more women enter the workforce and families increasingly turn to formal childcare arrangements rather than informal family-based care. However, this occupation carries substantial risks for work-related skin disorders that can significantly impact workers’ health, productivity, and career longevity.
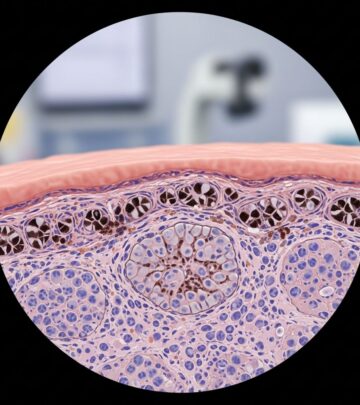
Understanding Occupational Skin Disease
Occupational skin diseases are dermatological conditions that result from or are exacerbated by the nature of a person’s employment. These conditions occur when the skin’s protective barrier is compromised through mechanical, chemical, or biological means, including cuts, abrasions, exposure to irritants and allergens, or contact with viruses and bacteria. The economic impact of occupational skin disorders is substantial, manifesting in missed work days and potentially forcing workers to change professions if conditions become severe.
In developed nations, stricter workplace regulations and increased emphasis on worker safety have contributed to reduced rates of occupational skin disorders. However, childcare workers remain at elevated risk despite these protections due to the unique demands of their work environment.
Occupational Risks in Childcare Settings
Childcare workers face multiple occupational hazards that increase their vulnerability to skin conditions:
- Wet work exposure: Frequent hand washing, sanitizing surfaces, and handling wet activities create prolonged skin moisture exposure
- Chemical exposure: Disinfectants, cleaning agents, and sanitizing products used throughout the childcare environment
- Biological hazards: Close contact with infants, toddlers, and preschoolers exposes workers to various pathogens
- Art supplies: Paints, adhesives, and craft materials contain potential irritants
- Personal protective equipment: Frequent glove use can cause irritation and trap moisture against the skin
- Physical trauma: Cuts, abrasions, and bite injuries from children in care
The most common causes of work-related contact dermatitis among childcare workers include contact with soaps, cleaning materials, and working with persistently wet hands. These factors combine to create an environment where skin barrier disruption occurs more frequently than in many other occupations.
Common Skin Disorders in Childcare Workers
Contact Dermatitis
Contact dermatitis is the most frequently occurring skin problem in childcare workers. This condition represents at least 80% of all occupational skin disease cases and can be subdivided into two primary types: irritant contact dermatitis and allergic contact dermatitis.
Irritant contact dermatitis develops when chemical exposure damages skin faster than the skin can repair itself. Common triggers in childcare settings include harsh soaps, disinfectants, and cleaning solutions. Allergic contact dermatitis occurs when the immune system reacts to specific allergens, which may include rubber compounds in latex gloves, certain disinfectants like chlorhexidine, and other chemical sensitizers.
Symptoms of contact dermatitis include:
- Red, itchy rash
- Vesicles or papules
- Blisters and swelling
- Scaling and peeling skin
- Burning sensations
- Open sores in severe cases
Infections and Infestations
Infectious conditions represent another common occupational risk for childcare workers. Due to close contact with young children, staff members are at increased risk for various bacterial and viral infections.
Bacterial infections, particularly those caused by staphylococci and streptococci, are common in childcare settings and present as boils, carbuncles, pustules, and areas of inflammation. These infections spread through direct skin-to-skin contact and contaminated surfaces. Childcare workers may also develop methicillin-resistant Staphylococcus aureus (MRSA) infections through similar transmission routes.
Head lice represent a frequent and ongoing problem in childcare settings. Lice spread through direct head-to-head contact and shared personal items such as combs, hats, and bedding. Repeated infestations are common, requiring persistent management and prevention strategies.
Human Bite Injuries
Due to contact with babies, toddlers, and preschoolers, human bite injuries may occur. Young children often express frustration or assert dominance through biting, particularly during developmental stages when verbal communication remains limited. These injuries can break the skin barrier, creating pathways for infection and requiring proper wound management and monitoring.
Host and Workplace Risk Factors
Personal Risk Factors
Individual characteristics increase susceptibility to occupational skin disease in childcare workers:
- Female sex: Women comprise the majority of childcare workers and experience higher rates of occupational dermatitis
- Atopic history: Personal or family history of atopic dermatitis, asthma, or allergic rhinitis increases vulnerability
- Younger age: Occupational contact dermatitis, particularly irritant types, occurs more frequently in younger workers
- Skin barrier dysfunction: Pre-existing skin conditions compromise the skin’s protective capacity
Workplace Environmental Factors
The childcare work environment contains multiple dermatological hazards:
- Cleaning agents and disinfectants (glutaraldehyde, ortho-phthalaldehyde, chlorhexidine)
- Tasks involving wet work and frequent hand washing
- Lack of health and safety training
- Inadequate personal protective equipment access
- Poor workplace ventilation
- Insufficient skin care product availability
Workplace Assessment and Prevention
Effective occupational health management in childcare facilities requires comprehensive workplace assessment. This involves evaluating chemical inventories, identifying high-risk tasks, assessing the adequacy of protective equipment, and determining whether workers receive adequate training on hazard prevention.
Prevention strategies with demonstrated protective effects include:
- Education and training: Comprehensive programs on hazard recognition and prevention measures
- Barrier protection: Access to appropriate gloves (nitrile alternatives for latex-sensitive individuals) and protective clothing
- Skin care products: Provision of non-fragranced moisturizers and gentle cleansers
- Engineering controls: Improved ventilation and access to less irritating cleaning alternatives
- Administrative controls: Rotation of tasks to reduce cumulative exposure
- Medical surveillance: Regular skin health checks and early intervention programs
Diagnosis and Clinical Presentation
Childcare workers presenting with occupational skin disorders typically display characteristic patterns based on exposure type and duration. Contact dermatitis manifests with redness, vesicles, papules, itching, pain, and burning sensations, often localized to the hands and forearms where chemical exposure is most intensive.
Diagnosis relies on clinical assessment, occupational history, and sometimes specialized testing. Patch testing can identify specific allergens responsible for allergic contact dermatitis, helping guide avoidance strategies. Distinguishing between irritant and allergic contact dermatitis is essential, as management approaches differ significantly.
The clinical assessment should include:
- Detailed occupational history and specific tasks performed
- Timeline of symptom onset and progression
- Distribution of skin lesions
- Exposure to known irritants or allergens
- Previous occupational or personal dermatological history
- Current preventive measures and their adequacy
Treatment Approaches
Management of occupational skin diseases in childcare workers involves both symptomatic treatment and exposure reduction. Mild contact dermatitis may resolve with topical corticosteroids and strict avoidance of causative agents. More severe cases may require systemic medications or specialist dermatological referral.
Infection management depends on the causative organism. Bacterial infections typically require appropriate antimicrobial therapy, though antibiotic stewardship principles should guide prescribing to minimize resistance development. Head lice require pediculicidal treatments and environmental measures to prevent reinfection.
Wound care for bite injuries emphasizes cleaning, infection prevention, and monitoring for secondary infection signs. Tetanus prophylaxis may be necessary depending on vaccination status and wound characteristics.
Impact and Long-Term Outcomes
Work-related skin conditions in childcare staff can have significant consequences extending beyond immediate dermatological effects. Chronic dermatitis may cause nighttime discomfort leading to sleep deprivation, affecting workplace performance and safety. Some workers experience psychological distress from visible skin lesions and social stigma. In severe cases, occupational skin disease necessitates career changes or occupational transitions.
Complications associated with prolonged dermatitis include secondary bacterial infections, development of respiratory conditions such as asthma and allergic rhinitis in susceptible individuals, and chronicity where acute conditions transition to persistent dermatological disorders.
Regulatory Context and Worker Protections
Occupational skin disease falls within the scope of workplace health and safety regulations in many jurisdictions. Employers have responsibilities to assess workplace hazards, implement control measures, provide appropriate training, and ensure access to personal protective equipment. Workers should receive instruction on recognizing early skin changes and reporting concerns to occupational health services.
Health surveillance programs monitoring for occupational skin disease help identify emerging problems and allow for timely intervention before conditions become disabling. Documentation of workplace-related skin conditions creates important health records and supports workers’ compensation claims when appropriate.
Frequently Asked Questions
Q: Which skin condition most commonly affects childcare workers?
A: Contact dermatitis is the most frequently occurring skin problem in childcare workers, accounting for the majority of occupational skin disease cases in this profession due to exposure to cleaning agents, disinfectants, and frequent wet work.
Q: Can latex gloves prevent occupational skin diseases in childcare settings?
A: While gloves provide barrier protection, they can paradoxically cause skin irritation through moisture trapping and latex sensitization. Latex-free nitrile gloves represent a better alternative for many workers, though proper glove hygiene and occasional glove-free periods allow skin recovery.
Q: How can childcare facilities reduce occupational skin disease rates?
A: Comprehensive approaches include providing worker education on hazard prevention, ensuring access to appropriate protective equipment, offering skin care products, using less irritating cleaning alternatives, and implementing medical surveillance programs to identify early skin changes.
Q: Are childcare workers at higher risk for head lice infections compared to other occupations?
A: Yes, childcare workers experience frequent head lice exposure due to close contact with infants and young children, making this a persistent occupational health challenge requiring ongoing prevention and treatment strategies.
Q: What should a childcare worker do if they develop skin symptoms they suspect are work-related?
A: Workers should report symptoms to occupational health services or their healthcare provider promptly, providing detailed information about workplace exposures and tasks. Early intervention prevents condition progression and may allow modifications reducing further exposure.
Q: Can occupational skin disease in childcare workers lead to permanent career changes?
A: Yes, if conditions become severe and don’t respond to treatment, occupational skin disease may necessitate career transitions, particularly if continued exposure to causative agents is unavoidable.
Conclusion
Occupational skin disease represents a significant health challenge for childcare workers worldwide. The combination of wet work, chemical exposure, and biological hazards creates an environment where contact dermatitis, infections, and infestations flourish. Effective management requires comprehensive approaches encompassing workplace hazard assessment, worker education, appropriate protective equipment provision, and medical surveillance. By implementing evidence-based prevention strategies and ensuring rapid intervention when symptoms develop, childcare facilities can substantially reduce the burden of occupational skin disease among their workforce, enabling these essential workers to maintain healthy skin and productive careers.
References
- Skin problems in childcare staff — DermNet. 2024. https://dermnetnz.org/topics/skin-problems-in-childcare-staff
- Prevalence of work-related skin symptoms and associated factors in health workers exposed to cleaning agents in two Southern African tertiary hospitals — National Center for Biotechnology Information (NCBI/PMC). 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10530256/
- Is Your Job Causing an Occupational Skin Disease? — Columbia Skin Clinic. 2024. https://columbiaskinclinic.com/skin-care/occupational-skin-diseases/
- Work-related skin problems: causes, conditions and care regimes — Mohs. 2021. https://mohs.co.uk/work-related-skin-problems-causes-conditions-and-care-regimes/
- Workers Who Risk Their Skin — Gen Re. 2015. https://www.genre.com/us/knowledge/publications/2015/august/cflh15-1-campbell-en
- Schools and Daycares: MRSA Prevention and Response — Centers for Disease Control and Prevention (CDC). 2024. https://www.cdc.gov/mrsa/prevention/schools-and-daycares.html
Read full bio of Sneha Tete