Sporotrichosis Pathology
Detailed histopathological analysis of sporotrichosis, a subcutaneous mycosis caused by Sporothrix schenckii, including clinical features and diagnostic insights.
Sporotrichosis is a chronic subcutaneous mycosis caused by the dimorphic fungus Sporothrix schenckii and related species. It primarily affects the skin following traumatic inoculation of fungal elements from environmental sources such as plant material, earning it the nickname “rose gardener’s disease.” Pathologically, it is characterized by epidermal hyperplasia overlying a mixed inflammatory infiltrate with granulomatous features and sparse fungal organisms that require diligent search for identification.
Histology
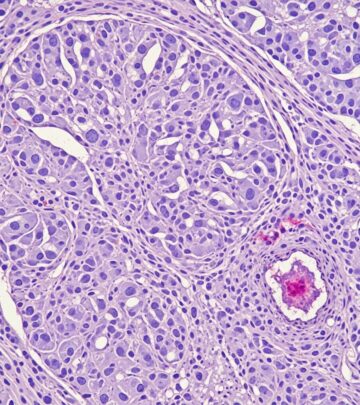
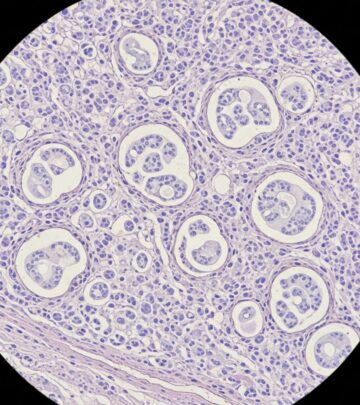
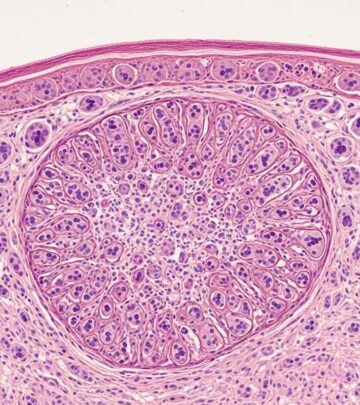
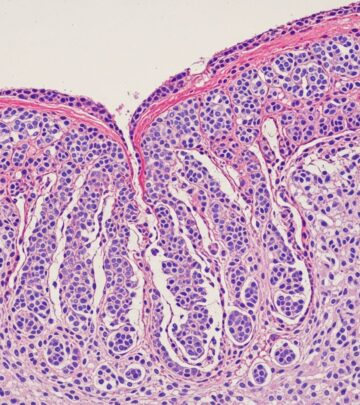
The hallmark histological feature of sporotrichosis is
pseudoepitheliomatous hyperplasia
of the epidermis, which appears as marked acanthosis and elongation of rete ridges, often mimicking squamous cell carcinoma. This epidermal reaction overlies a dense dermal inflammatory infiltrate that extends into the subcutis in advanced cases.The inflammatory response is polymorphous, comprising acute and chronic components. Key elements include:
- Neutrophilic microabscesses: Small collections of neutrophils within the dermis, often surrounded by histiocytes.
- Granulomatous inflammation: Loose aggregates of epithelioid histiocytes, multinucleated giant cells (both Langhans and foreign body types), and lymphocytes.
- Lymphoplasmacytic infiltrate: Plasma cells and lymphocytes interspersed throughout.
- Epidermal involvement: Inflammation may spill over into the epidermis, causing spongiosis or microabscesses in the stratum corneum.
In lymphocutaneous forms, the infiltrate follows lymphatic channels, showing perivascular and periadnexal distribution. Chronic lesions may develop fibrosis, while early lesions emphasize acute suppuration.
Microscopic Images Description
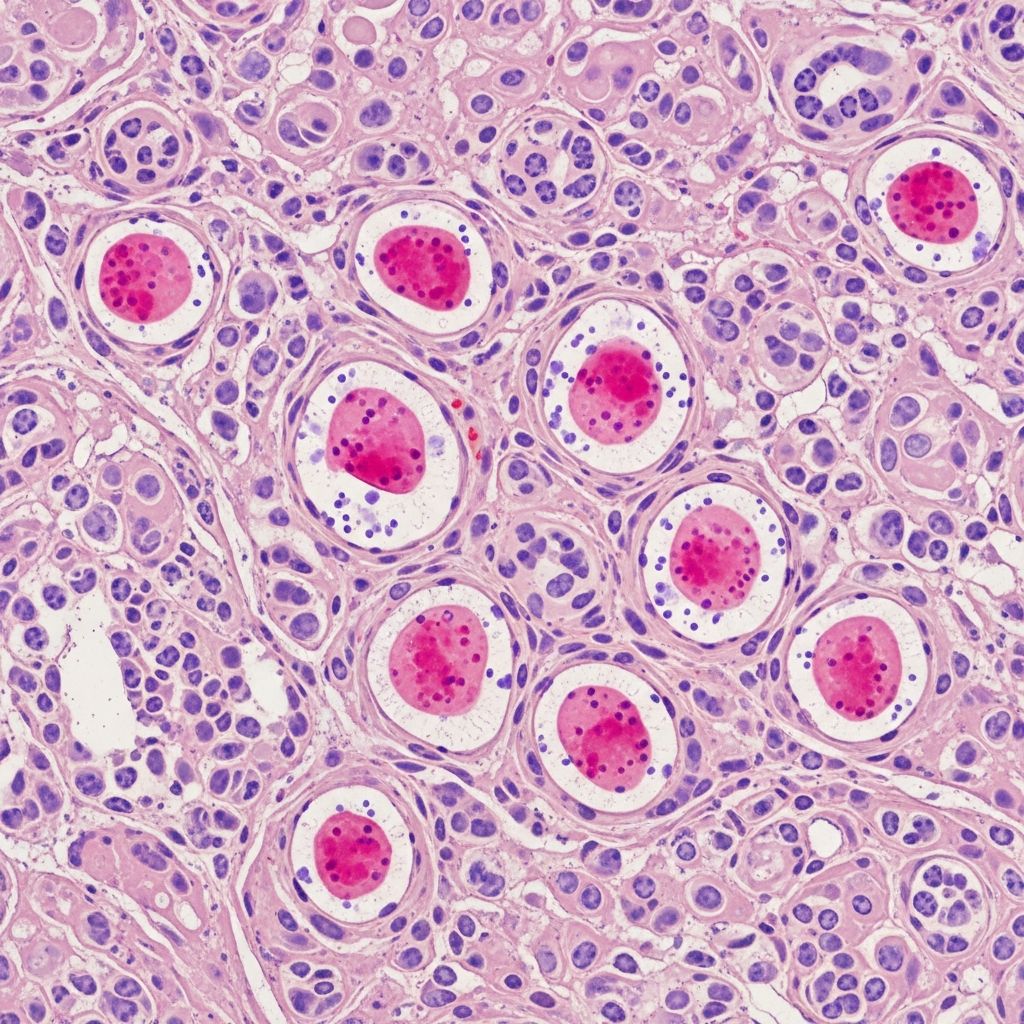
Low-power views reveal epidermal hyperplasia with a wedge-shaped dermal infiltrate (figure 1 equivalent). Medium power highlights the mixed nature with giant cells and neutrophils (figure 2). High power is essential for spotting organisms, often cigar-shaped yeasts amid inflammation (figure 4, arrows).
Microbiology
Sporothrix schenckii is a thermally dimorphic fungus: mold at 25°C and yeast at 37°C. In tissue, it manifests as small (2-10 μm), oval to cigar-shaped yeasts with narrow-based budding. The organisms are notoriously sparse, necessitating examination of multiple levels and special stains.
| Feature | Description | Stain |
|---|---|---|
| Yeast size | 2-10 μm, oval/cigar-shaped | H&E, GMS |
| Budding | Narrow-based, single bud | PAS, GMS |
| Wall | Thin, rarely thick-walled sclerotic bodies | GMS (best) |
| Arrangement | Scattered, intracellular in giant cells | All |
Special stains enhance visibility:
- Gomori methenamine silver (GMS): Black yeasts on green background; most sensitive.
- Periodic acid-Schiff (PAS): Magenta yeasts.
- Mucicarmine: Occasionally positive capsule.
- H&E shows yeasts as faintly eosinophilic with surrounding clear halo.
Culture confirmation on Sabouraud agar yields creamy colonies with septate hyphae and conidia. Molecular methods like PCR are emerging for rapid ID.
Cytology
Fine-needle aspiration or scrapings from lesions show suppurative inflammation with granulomas. Yeasts are identifiable in 50-70% of cases with special stains, aiding presumptive diagnosis in resource-limited settings. Tzanck smears may reveal yeasts but lack specificity.
Clinical Features Supporting Pathology
Sporotrichosis presents in several forms, each with corresponding pathology:
| Form | Clinical | Pathology |
|---|---|---|
| Lymphocutaneous (75%) | Primary nodule + linear lymphatic nodules | Granulomas along lymphatics, microabscesses |
| Fixed cutaneous | Single verrucous plaque | Marked pseudoepitheliomatous hyperplasia |
| Disseminated | Multiple lesions (immunocompromised) | Less granulomatous, more suppurative |
| Extracutaneous | Osteoarticular, pulmonary, meningitis | Similar yeasts, tissue-specific inflammation |
Common in gardeners, farmers; incubation 1-12 weeks post-trauma.
Differential Diagnosis
Pathological mimics include:
- Leishmaniasis: Amastigotes (4-6 μm, kinetoplast on Giemsa).
- Nocardia: Filamentous branching bacteria (Gram, modified AFB).
- Chromoblastomycosis: Sclerotic bodies (copper pennies, 5-12 μm).
- Mycobacterial infections: Acid-fast bacilli.
- Pyoderma gangrenosum: Sterile neutrophilic infiltrate without organisms.
Dermoscopy aids: lobular white areas (hyperkeratosis), scaling, polymorphous vessels, blood spots.
Advanced Diagnostic Insights
Recent studies emphasize clinicopathological correlation. In one case, a 70-year-old with rose thorn injury showed hyperkeratosis, parakeratosis, epidermal hyperplasia, neutrophilic abscesses, and PAS+ yeasts. WHO notes microscopy/histopathology/culture as gold standards, with molecular tools in development. South African perspectives highlight Sporothrix brasiliensis emergence in outbreaks.
Imaging in osteoarticular forms shows lytic bone lesions; pulmonary mimics TB with cavitary disease.
Treatment Considerations from Pathology
Response monitoring via histology: resolution of microabscesses and organisms. Itraconazole (skin), amphotericin B (disseminated) guided by culture susceptibility.
Frequently Asked Questions (FAQs)
Q: What is the most common histological finding in sporotrichosis?
A: Pseudoepitheliomatous epidermal hyperplasia overlying granulomatous inflammation with neutrophilic microabscesses.
Q: How are Sporothrix organisms best visualized?
A: GMS stain highlights small, cigar-shaped yeasts with narrow-based budding; they are sparse on H&E.
Q: Which clinical form is most frequent?
A: Lymphocutaneous, with primary chancre and secondary lymphatic nodules.
Q: Is sporotrichosis contagious person-to-person?
A: Rarely; mainly zoonotic (cats in Brazil) or traumatic inoculation.
Q: What special stain is gold standard for fungi?
A: GMS for sensitivity; PAS for morphology.
Pathological Evolution Over Time
Early: Suppurative dermatitis. Intermediate: Granuloma formation. Late: Fibrosis with persistent yeasts if untreated. Immunocompromised: Sparse granulomas, dissemination.
References
- Cutaneous sporotrichosis with dermoscopic features: A case report — Dergipark. 2019-01-01. https://dergipark.org.tr/en/download/article-file/773027
- Sporotrichosis pathology image — DermNet NZ. 2023-01-01. https://dermnetnz.org/imagedetail/18514-sporotrichosis-pathology
- Sporotrichosis — DermNet NZ. 2024-01-01. https://dermnetnz.org/topics/sporotrichosis
- Sporotrichosis — World Health Organization. 2023-05-15. https://www.who.int/news-room/fact-sheets/detail/sporotrichosis
- Deep Fungal Infections of Skin and Role of Histopathology — PMC/NCBI. 2024-01-01. https://pmc.ncbi.nlm.nih.gov/articles/PMC11642464/
- Sporothrix and Sporotrichosis: A South African Perspective — Wiley Online Library. 2024-06-15. https://onlinelibrary.wiley.com/doi/full/10.1111/myc.13806
Read full bio of medha deb