Synovial Metaplasia Pathology: Definition & Clinical Significance
Understanding synovial metaplasia: A specialized tissue response to trauma and prosthetic materials in dermatopathology.

Synovial Metaplasia Pathology: A Comprehensive Overview
Synovial metaplasia represents a distinctive pathological change characterized by the development of tissue structures that histologically resemble normal synovium in locations where synovial tissue does not normally exist. This phenomenon is encountered most frequently in tissues surrounding silicone breast prostheses and in healing tissue adjacent to joint prostheses, though it may also occur in the skin and soft tissues, particularly in healing or healed traumatic or surgical wounds. Understanding this pathological entity is crucial for dermatopathologists and clinicians to avoid misdiagnosis and provide appropriate clinical management.
Definition and Pathological Classification
Synovial metaplasia is fundamentally a change in cell differentiation where normal connective tissue cells transform into cells that structurally and functionally resemble synovial membrane. The condition is often referred to as a metaplastic synovial cyst when it presents in a cystic form within the dermis or subcutaneous tissues. Unlike a true cyst, which is lined by epithelial cells, a metaplastic synovial cyst is technically a pseudocyst—an irregularly shaped cavity that lacks a true epithelial lining but is instead surrounded by a characteristic membrane resembling hyperplastic synovium.
The pathological designation of “metaplastic synovial cyst” is considered appropriate because it accurately reflects both the structural features and the biological nature of the lesion. This classification helps distinguish it from other cutaneous cystic lesions and aids in establishing a standardized approach to diagnosis and management.
Pathogenesis and Etiology
The development of synovial metaplasia is intrinsically linked to tissue trauma and foreign body presence. The primary etiological factors include:
- Surgical procedures: Previous surgical intervention in the affected area is present in the majority of cases.
- Prosthetic materials: Silicone prostheses, particularly breast implants, are among the most common triggers of synovial metaplasia.
- Repetitive trauma: Constant mechanical stress, pressure, or manipulation of tissue can initiate the metaplastic process.
- Foreign material injection: Air or oil injection, hyaluronic acid fillers, orthopedic prostheses, and breast implants have all been documented as potential triggers.
- Mechanical disruption: Normal synovium is embryologically derived from mechanical disruption of connective tissues that occurs during fetal movement in vivo, suggesting that the synovium-like membrane in cutaneous metaplasia arises from similar connective tissue disruption.
The temporal relationship between trauma and lesion development is variable, with the interval between initial trauma and the onset of synovial metaplasia ranging from a few weeks to several years. This variable timeline suggests a complex biological process involving tissue remodeling and adaptive responses to the initial insult.
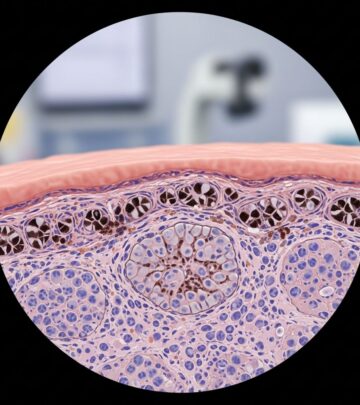
Histopathological Features
The microscopic examination of synovial metaplasia reveals characteristic features that distinguish it from other dermatological conditions. The key histopathological findings include:
| Histopathological Feature | Description |
|---|---|
| Cystic Structure | Irregularly shaped cystic space without an epithelial lining (pseudocyst) surrounded by dense fibrosis |
| Synovial-like Lining | Characteristic membrane with eosinophilic spindle-shaped cells and processes toward the lumen, identical to normal synovium |
| Cellular Composition | Mixture of epithelioid, fibroblastic, mononuclear inflammatory, and multinucleated giant cells |
| Villous Projections | Variable degrees of villous structures extending toward the center of the cystic cavity |
| Surrounding Tissue | Reactive changes in dermis or subcutaneous tissue, including fibrosis and inflammation |
| Epidermal Features | Possible fistula tract connecting the epidermis to the cyst |
The membrane lining demonstrates strong staining with vimentin, indicating mesenchymal origin, and scattered positivity with alpha-1-antichymotrypsin and lysozyme. Notably, there is an absence of basement membrane antigens and elastic fibers, which further distinguishes this lesion from true epithelial cysts.
Immunohistochemical Characteristics
Immunohistochemical analysis plays a supportive role in confirming the diagnosis of synovial metaplasia, though it is not mandatory for diagnosis when characteristic histopathological findings are present. The typical immunophenotype includes:
- Positive staining: Strong vimentin positivity, indicating mesenchymal/fibroblastic differentiation
- Negative staining: Keratin, S-100, and carcinoembryonic antigen (CEA) are consistently negative
- CD-68 positivity: May be observed, consistent with histiocytic/macrophage involvement in the inflammatory response
- Lysozyme and alpha-1-antichymotrypsin: Scattered positivity reflecting the presence of mononuclear inflammatory cells
These immunohistochemical patterns confirm the mesenchymal nature of the lesion and help exclude other diagnostic possibilities such as epithelial cysts or lymphoid proliferations.
Clinical Presentation
Clinically, synovial metaplasia most commonly presents as a tender intradermal nodule frequently associated with scar tissue. The clinical manifestations are variable and may include:
- Solitary or multiple nodules, typically tender to palpation
- Erythematous appearance in many cases, though some lesions may be skin-colored
- Association with previous surgical scars or trauma sites
- Possible central punctured orifice, suggesting drainage or fistulization
- No predilection for specific anatomical sites or sex
- Can occur at any age, though often related to prior surgical intervention
The lesion may clinically resemble suture granulomas, which is an important consideration in the differential diagnosis. On imaging, ultrasonographic examination typically reveals a hypoechoic structure with possible posterior acoustic enhancement.
Associated Clinical Conditions
Synovial metaplasia has been documented in association with several specific scenarios:
Breast Prosthesis-Related Metaplasia: One of the most significant and well-documented associations is the development of true synovial metaplasia in the periprosthetic capsule surrounding silicone breast implants. In these cases, electron microscopy and chemical analysis have demonstrated the presence of silicone and other inorganic deposits at the surface of and within the synovial layer, indicating that the metaplastic response is triggered by silicone itself rather than by the surgical procedure alone. The periprosthetic capsule demonstrates three distinct histological layers: intimae, subintima, and fibrous capsule, with the intimate layer exhibiting the characteristic synovial features.
Transepidermal Fistulae: In cutaneous manifestations of synovial metaplasia, the metaplastic foci are often associated with cyst formation and transepidermal fistulae, creating communication between the dermal lesion and the skin surface. This finding reflects the body’s attempt to drain the cystic content through the overlying epidermis.
Differential Diagnosis
Several conditions must be considered and excluded when evaluating suspected synovial metaplasia:
Implantational Epidermal Cyst: This is perhaps the most important differential diagnosis, as both entities can arise after local trauma or surgery and present with similar clinical features. However, the critical distinction lies in the histological findings: implantational epidermal cysts possess a true epithelial lining, whereas synovial metaplasia lacks this epithelial lining and instead demonstrates a synovium-like membrane. Additionally, implantational epidermal cysts are classified as true cysts due to their epithelial lining, while synovial metaplasia represents a pseudocyst.
Suture Granuloma: These lesions develop in response to suture material and typically present with granulomatous inflammation. The characteristic synovial lining of metaplastic synovial cysts distinguishes them from suture granulomas histologically.
Other Cutaneous Cysts: Standard epidermoid cysts, pilar cysts, and other benign cystic lesions can be differentiated by the absence of the distinctive synovial membrane lining present in synovial metaplasia.
Clinical Management and Prognosis
The standard treatment for symptomatic synovial metaplasia is complete surgical excision. In reported cases, excision has been followed by neither recurrence nor complications during the follow-up period, suggesting that complete removal of the lesion provides a durable cure. The prognosis is generally favorable, with no documented high recurrence rates when the entire lesion is adequately removed.
Awareness of this rare entity among clinicians and dermatopathologists is crucial for accurate diagnosis and appropriate management, as misdiagnosis may lead to unnecessary treatments or delayed recognition of the true pathology.
Frequently Asked Questions
Q: What is the difference between synovial metaplasia and a true synovial cyst?
A: Synovial metaplasia, particularly in cutaneous manifestations, forms a pseudocyst—an irregular cavity without an epithelial lining that is instead lined by a membrane resembling hyperplastic synovium. True synovial cysts, in contrast, are actual cysts with a true epithelial lining. Additionally, true synovial cysts arise in locations with native synovial tissue, such as around joints, whereas metaplastic synovial cysts represent an ectopic occurrence of synovial features in non-synovial-bearing tissues.
Q: Is immunohistochemical testing mandatory for diagnosing synovial metaplasia?
A: No, immunohistochemical analysis is not mandatory for diagnosis. When characteristic histopathological findings are present—including the irregular pseudocyst structure, synovium-like lining, and appropriate cellular composition—the diagnosis can be established through routine light microscopy alone. However, immunohistochemistry can serve as a supportive tool when morphological features are ambiguous.
Q: What is the typical time interval between trauma and the development of synovial metaplasia?
A: The duration between the initial trauma or surgical procedure and the clinical onset of synovial metaplasia is highly variable, ranging from a few weeks to several years. This variability suggests that the metaplastic process involves complex tissue remodeling and adaptive biological responses.
Q: Are there any sites of predilection for synovial metaplasia?
A: No, there is no documented site predilection for synovial metaplasia. The condition can arise at any anatomical location where prior trauma or surgical intervention has occurred. However, it is most commonly associated with breast prosthesis sites and areas with a history of joint surgery.
Q: What is the recommended treatment for synovial metaplasia?
A: Complete surgical excision is the standard and recommended treatment. When the entire lesion is adequately removed, recurrence and complications are not commonly observed during follow-up, supporting the effectiveness and durability of this approach.
Q: Can synovial metaplasia occur without a history of surgery or trauma?
A: While the vast majority of documented cases are associated with a history of surgical procedures or trauma, the broader pathogenic mechanism involves mechanical disruption of connective tissues. However, virtually all well-documented cases have had preceding trauma or surgical intervention, making a negative history quite unusual.
References
- Synovial metaplasia of the skin — PubMed/NCBI. 1985. https://pubmed.ncbi.nlm.nih.gov/3578644/
- Cutaneous Metaplastic Synovial Cyst of the Cheek — PubMed Central/NCBI. 2011. https://pmc.ncbi.nlm.nih.gov/articles/PMC3229074/
- True synovial metaplasia of a periprosthetic breast capsule — Revista Española de Patología. 2008. http://patologia.es/volumen41/vol41-num4/41-4n08.htm
- Synovial metaplasia pathology — DermNet NZ. 2013. https://dermnetnz.org/topics/synovial-metaplasia-pathology
- Synovial metaplasia, a specialized form of repair: a case report and review of the literature — Gale/Academic OneFile. 2012. https://go.gale.com/ps/i.do?id=GALE|A87564063
Read full bio of medha deb