Twin Reversed Arterial Perfusion (TRAP): Causes, Diagnosis & Treatment
Understanding TRAP sequence: A rare condition affecting monochorionic twin pregnancies requiring specialized care.
Understanding Twin Reversed Arterial Perfusion (TRAP) Sequence
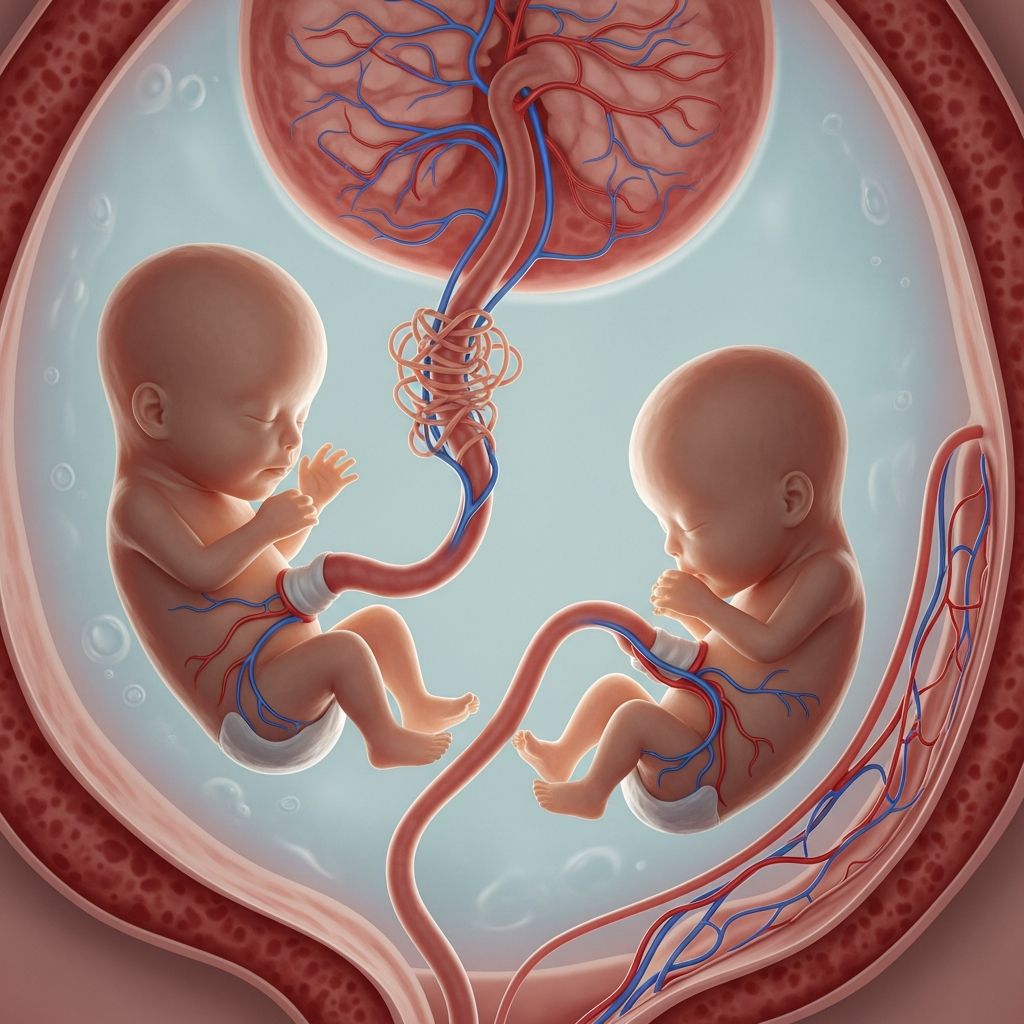
Twin reversed arterial perfusion (TRAP) sequence is a rare and serious condition that affects only pregnancies where identical twins share a placenta, a condition known as monochorionic twin pregnancies. This complex syndrome presents significant challenges to both the developing twins and the expectant parents who must navigate difficult medical decisions. TRAP sequence occurs when one twin, called the acardiac twin, develops without a functioning heart or with a severely underdeveloped cardiac system. The other twin, referred to as the pump twin, has a normally functioning heart that must work considerably harder to supply blood for both fetuses. This extraordinary demand on a single heart creates life-threatening risks that require specialized medical attention and careful monitoring throughout pregnancy.
What is TRAP Sequence?
Twin reversed arterial perfusion sequence is characterized by a unique circulatory anomaly that occurs in monochorionic twin pregnancies. In normal circumstances, blood flows through the umbilical artery away from the fetus toward the placenta, and returns through the umbilical vein carrying oxygen-rich blood from the placenta. However, in TRAP sequence, this normal blood flow pattern is reversed. Blood enters the acardiac twin through the umbilical artery and exits through the umbilical vein in the opposite direction from what occurs in typical fetal development. This reversed arterial perfusion occurs through vascular connections called anastomoses that naturally develop in the shared placenta.
The acardiac twin survives entirely dependent on blood supplied by the pump twin through these placental connections. This blood has already circulated through the pump twin’s body and carries lower oxygen levels than normal fetal blood. As a result, the acardiac twin typically develops with severe abnormalities. The cranial structures, including the head and upper body, are usually most severely affected due to receiving the most deoxygenated blood. The lower body parts develop more normally since they receive blood with slightly higher oxygen content. Many acardiac twins lack a functional heart, head, or upper extremities, existing as severely malformed tissue masses sustained only by the placental blood supply from their twin.
Incidence and Prevalence
TRAP sequence is an exceptionally rare condition, occurring in approximately 1 percent of monochorionic twin pregnancies. When considering all births overall, the incidence is approximately 1 in 35,000. Despite its rarity, TRAP sequence represents one of the most serious complications that can develop in multiple pregnancies. The condition occurs randomly and unpredictably, with no known preventive measures. Once TRAP sequence develops, it requires immediate specialized medical attention and close monitoring to optimize outcomes for the pump twin.
The Pump Twin: Understanding the At-Risk Twin
The pump twin appears normal on initial ultrasound examination and possesses all the necessary anatomical structures for normal fetal development. However, the pump twin faces extraordinary physiological stress because its heart must perform the work of two hearts. This single cardiac system must pump blood not only for its own body but also through the placental connections to perfuse the acardiac twin. This doubled workload creates significant cardiovascular strain that can lead to serious complications.
As the acardiac twin continues to grow larger during pregnancy, the workload on the pump twin’s heart increases proportionally. The larger the acardiac twin becomes, the greater the volume of blood that must be diverted to support it, leaving relatively less oxygen-rich blood available for the pump twin’s own vital organs. This progressive strain can trigger heart failure, a life-threatening condition in which the pump twin’s heart becomes unable to meet the circulatory demands placed upon it.
The Acardiac Twin: Clinical Features
The acardiac twin typically exhibits severe developmental abnormalities affecting multiple body systems. The most characteristic feature is the complete absence of a functioning heart or the presence of only rudimentary cardiac tissue incapable of sustaining independent circulation. Beyond cardiac abnormalities, the acardiac twin frequently lacks normal development of the head, brain, and upper body structures. These twins may be missing limbs or have severely underdeveloped extremities. Despite these profound anatomical abnormalities, the acardiac twin does develop some tissues and organs, though often in an abnormal fashion, sustained entirely by the oxygen-poor blood received from the pump twin.
The acardiac twin cannot survive independently outside the womb because it possesses no functioning cardiac system capable of generating its own blood circulation. Survival depends entirely on the placental connection and the pump twin’s cardiac function. Once the umbilical cord is cut at delivery, the acardiac twin immediately loses its blood supply and cannot be sustained by any medical intervention.
Diagnosis and Evaluation
Accurate diagnosis of TRAP sequence requires specialized ultrasound techniques performed by experienced fetal medicine specialists. The diagnostic evaluation begins with detailed ultrasound imaging that can identify the characteristic features of this condition. Fetal echocardiography, a specialized ultrasound focusing specifically on fetal cardiac structure and function, provides crucial information about the pump twin’s heart. This detailed cardiac imaging assesses whether the pump twin’s heart shows signs of strain, enlargement, or dysfunction that would indicate compromised cardiac function.
Color flow Doppler ultrasound is an essential diagnostic tool that visualizes blood flow patterns and confirms the pathognomonic finding of reversed arterial flow in the acardiac twin. This Doppler imaging demonstrates blood flowing backward through the arterial anastomoses, confirming the diagnosis of TRAP sequence. The characteristic pattern of blood flowing in the opposite direction from normal fetal circulation is virtually diagnostic of this condition.
Important biometric measurements are obtained during the diagnostic ultrasound evaluation. Growth discrepancies between the twins, particularly in abdominal circumference measurements, are typical findings in TRAP sequence. These measurements help establish the diagnosis and provide prognostic information about the likely course of the pregnancy.
Prognostic Factors and Risk Stratification
Several factors help predict the likely outcome for pregnancies complicated by TRAP sequence. The most important prognostic indicator is the weight ratio between the acardiac and pump twins. If the acardiac twin weighs more than 75 percent of the pump twin’s weight, the pump twin faces a dramatically increased risk of death, occurring in approximately 95 percent of such cases. This weight ratio is crucial because it directly correlates with the workload imposed on the pump twin’s heart.
Without treatment, the pump twin has only a 25 to 50 percent chance of survival. Left untreated, TRAP sequence is fatal to the pump twin in 50 to 75 percent of pregnancies due to progressive heart failure as the workload becomes unsustainable. The acardiac twin has 100 percent mortality, as it cannot survive outside the womb and is not compatible with independent life.
Additional poor prognostic factors include continued growth of the acardiac twin, development of polyhydramnios (excessive amniotic fluid), enlargement of the pump twin’s heart (cardiomegaly), and accumulation of fluid around the heart (pericardial effusion). Low pulsatility index in the umbilical artery of the pump twin, as measured by Doppler ultrasound, also indicates a poor prognosis.
Pregnancy Complications Associated with TRAP Sequence
TRAP sequence frequently causes multiple serious complications that threaten both the pregnancy and the survival of the pump twin. More than half of pregnancies affected by TRAP sequence develop polyhydramnios, characterized by excessive accumulation of amniotic fluid. This occurs because the increased blood flow to the acardiac twin’s kidneys results in overproduction of fetal urine, the primary source of amniotic fluid. The buildup of excess fluid places the pregnancy at risk for premature rupture of membranes and preterm labor.
Preterm labor occurs in approximately 75 percent of pregnancies complicated by TRAP sequence. Delivery before 37 weeks of gestation creates significant risks for the pump twin, including respiratory distress syndrome, intraventricular hemorrhage, and other complications associated with prematurity. Approximately 90 percent of pregnancies with an acardiac twin weight ratio above 70 percent experience preterm delivery.
Progressive heart failure develops in the pump twin as the cardiac workload becomes unsustainable. Congestive heart failure occurs in approximately 30 percent of pregnancies with high weight ratios between the twins. Hydrops, a life-threatening condition characterized by abnormal fluid accumulation throughout the pump twin’s body including the lungs, heart sac, and abdominal cavity, represents a medical emergency. These complications frequently necessitate early delivery despite the risks associated with prematurity.
Treatment Options for TRAP Sequence
When TRAP sequence is diagnosed and the pump twin is determined to face increased risk for heart failure, fetal surgical intervention may be recommended. The goal of treatment is to eliminate blood flow to the acardiac twin by closing off the vascular connections that sustain its abnormal circulation. By interrupting the blood supply to the acardiac twin, the workload on the pump twin’s heart is immediately reduced, allowing the pump twin’s cardiac system to function more normally and sustainably.
Minimally invasive fetal surgical techniques are available to accomplish this goal. These procedures can be performed with relatively low risk to the pump twin and the pregnancy. The intervention involves accessing the placental cord connections and using techniques such as bipolar cord coagulation or selective feticide to stop blood flow to the acardiac twin. These procedures are minimally invasive compared to open fetal surgery and carry a relatively low rate of procedure-related complications.
Successful treatment dramatically improves the prognosis for the pump twin. After successful intervention to eliminate blood flow to the acardiac twin, the pump twin’s survival rate improves significantly, and the risk of heart failure is substantially reduced. The procedure does not affect the pump twin’s ability to achieve normal delivery or impact future childbearing capacity.
Key Considerations for Parents
Parents facing a diagnosis of TRAP sequence confront difficult decisions about pregnancy management. The diagnosis requires compassionate counseling from experienced maternal-fetal medicine specialists who can discuss prognosis, treatment options, and likely outcomes. Each family’s values, preferences, and circumstances should guide the decision-making process regarding whether to pursue fetal intervention, expectant management with close monitoring, or pregnancy termination.
Close collaboration between maternal-fetal medicine specialists, neonatologists, pediatric cardiologists, and other specialists is essential to optimize outcomes. Pregnancies complicated by TRAP sequence should be delivered at tertiary care centers capable of providing intensive neonatal care if the pump twin survives to delivery.
Frequently Asked Questions
Q: Can TRAP sequence be prevented?
A: No, TRAP sequence cannot be prevented. It occurs randomly and unpredictably in monochorionic twin pregnancies. The exact cause remains uncertain but is thought to result from abnormal blood pressure or blood flow patterns that develop very early in pregnancy.
Q: Will the pump twin definitely die if treatment isn’t provided?
A: Without treatment, approximately 50 to 75 percent of pump twins die from heart failure. However, some pregnancies with TRAP sequence can result in pump twin survival even without intervention, though this is less common. The likelihood depends on factors such as the weight ratio between the twins and the severity of cardiac strain.
Q: Can the acardiac twin be saved?
A: No, the acardiac twin cannot be saved or treated. This twin cannot survive outside the womb because it lacks a functioning heart and possesses severe developmental abnormalities incompatible with life. Treatment focuses entirely on saving the pump twin by reducing the workload on its heart.
Q: How is TRAP sequence different from other complications of monochorionic twin pregnancies?
A: TRAP sequence is distinct from other monochorionic complications like twin-to-twin transfusion syndrome (TTTS). In TRAP, one twin has no functioning heart, whereas in TTTS both twins have functioning hearts but blood preferentially flows from one twin to the other through placental connections. The management and prognosis differ significantly between these conditions.
Q: What is the long-term outlook for survivors of TRAP sequence?
A: Pump twins who survive TRAP sequence, particularly those who receive fetal intervention, can have normal long-term outcomes. These children develop normally without cardiac complications in most cases. Normal vaginal delivery is possible, and future pregnancies are not affected by having had TRAP sequence in a prior pregnancy.
Q: How often should monitoring occur in pregnancies with TRAP sequence?
A: Pregnancies with TRAP sequence require close surveillance, typically with ultrasound examinations every 1 to 2 weeks. More frequent monitoring may be necessary if signs of deterioration develop, such as increasing polyhydramnios, cardiac enlargement, or hydrops in the pump twin.
References
- Twin Reversed Arterial Perfusion Sequence and Bipolar Cord Coagulation for Acardiac Acephalic Twins — Children’s Hospital of Philadelphia. 2024. https://www.chop.edu/conditions-diseases/twin-reversed-arterial-perfusion-sequence-and-bipolar-cord-coagulation-for-acardiac-acephalic-twins
- Twin Reversed Arterial Perfusion (TRAP) Sequence — National Center for Biotechnology Information (NIH). 2015. https://pmc.ncbi.nlm.nih.gov/articles/PMC4632132/
- Twin Reversed Arterial Perfusion Sequence (TRAP) — University Hospitals Fetal Center. 2024. https://www.uhhospitals.org/services/obgyn-womens-health/conditions-and-treatments/high-risk-pregnancy/conditions-and-treatments/fetal-diagnosis-and-treatment/fetal-conditions-and-treatments/twin-reversed-arterial-perfusion-sequence
- Twin Reversed Arterial Perfusion (TRAP) Sequence — Nationwide Children’s Hospital. 2024. https://www.nationwidechildrens.org/conditions/twin-reversed-arterial-perfusion-trap-sequence
- Twin Reversed Arterial Perfusion (TRAP) Sequence — Riley Children’s Health. 2024. https://www.rileychildrens.org/health-info/twin-reversed-arterial-perfusion-trap-sequence
- Twin Reversed Arterial Perfusion (TRAP) Sequence or Acardiac Twin — UCSF Fetal Treatment Center. 2024. https://fetus.ucsf.edu/trap-sequence/
Read full bio of medha deb