Ulcerative Colitis Treatment: 5 Essential Goals And Options
Comprehensive guide to managing ulcerative colitis with medications, biologics, surgery, and emerging therapies for remission.
Ulcerative Colitis Treatment: Options and Strategies
Ulcerative colitis (UC) is a chronic inflammatory bowel disease affecting the colon and rectum, causing symptoms like diarrhea, abdominal pain, and rectal bleeding. Treatment focuses on reducing inflammation, achieving remission, preventing flares, and minimizing complications. Strategies vary by disease severity—from mild to severe—and extent, including proctitis, left-sided colitis, extensive colitis, and pancolitis. Options include medications like aminosalicylates, corticosteroids, immunomodulators, biologics, small molecules, and surgery when medical therapy fails.
What Is Ulcerative Colitis?
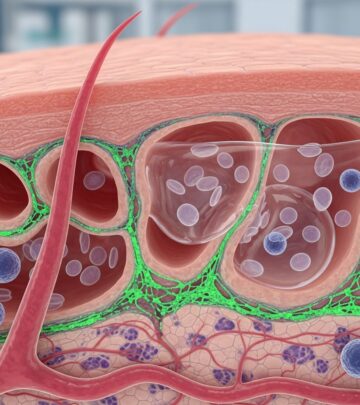
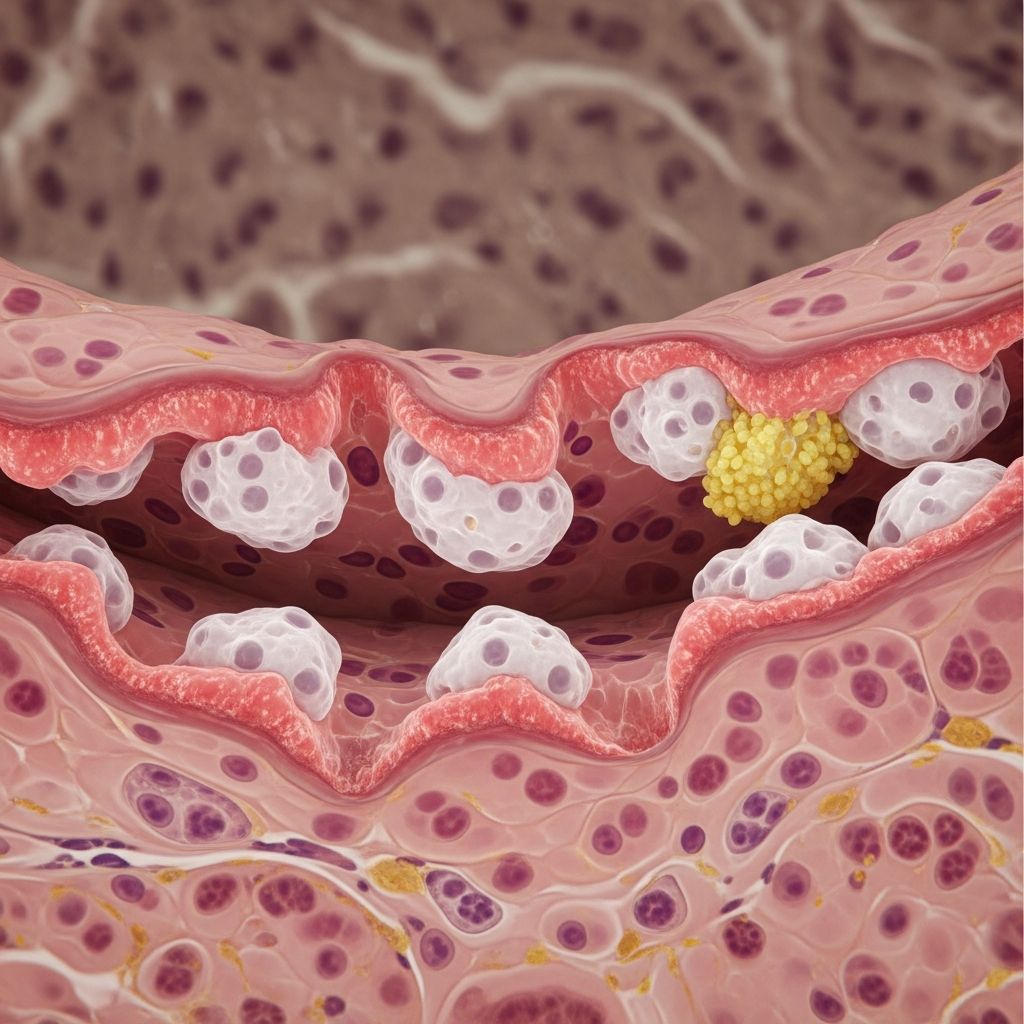
UC involves continuous inflammation of the colon’s mucosal lining, starting in the rectum and potentially extending proximally. Unlike Crohn’s disease, it spares the small intestine. Symptoms range from bloody diarrhea and urgency to fatigue and weight loss. Diagnosis uses endoscopy, biopsy, and imaging. Early intervention prevents progression to fulminant colitis or colorectal cancer risk.
Goals of therapy: induce remission (resolve symptoms and heal mucosa), maintain remission, and improve quality of life. Tailored plans consider patient age, comorbidities, pregnancy status, and prior responses. Multidisciplinary care involves gastroenterologists, dietitians, and surgeons.
Treatment Goals for Ulcerative Colitis
- Induce remission: Rapid symptom control and mucosal healing using anti-inflammatory drugs.
- Maintain remission: Long-term therapy to prevent relapses, often with maintenance agents.
- Minimize side effects: Balance efficacy with safety, using lowest effective doses.
- Manage complications: Address extraintestinal manifestations like arthritis or anemia.
- Achieve mucosal healing: Endoscopic targets for better outcomes and reduced surgery risk.
Treatment escalates stepwise: start with aminosalicylates (5-ASA), add steroids for flares, then immunomodulators or biologics for steroid-dependent cases. Surgery cures UC by removing the colon but impacts lifestyle.
Treatment by Severity
UC severity guides therapy: mild (fewer than 4 stools/day, no systemic signs), moderate (more stools, mild anemia), severe (6+ bloody stools, fever, tachycardia), fulminant (toxic megacolon, perforation risk).
Mild to Moderate Ulcerative Colitis
For mild distal disease (proctitis or left-sided), topical 5-ASA suppositories or enemas (1g nightly) achieve remission in 80-90%. Oral mesalamine (2.4-4.8g/day) for extensive mild-moderate. Combinations of oral and rectal 5-ASA superior to monotherapy. If unresponsive, add oral budesonide-MMX (9mg/day) or systemic steroids.
| Severity | First-Line Therapy | Alternatives |
|---|---|---|
| Mild Proctitis | Mesalamine suppository 1g HS | Hydrocortisone foam; add oral 5-ASA |
| Mild-Moderate Left-Sided | Mesalamine enema 4g HS + oral 2.4g/day | Budesonide enema; prednisone |
| Mild-Moderate Extensive | Oral mesalamine 4.8g/day | Rectal 5-ASA + oral; steroids |
Moderate to Severe Ulcerative Colitis
Oral prednisone (40-60mg/day) induces remission in 70% within 7-14 days. Taper slowly to avoid rebound. IV steroids (methylprednisolone 60mg/day or hydrocortisone 300-400mg/day) for hospitalized patients. Non-responders (no improvement in 3-5 days) get cyclosporine (2mg/kg IV infusion) or infliximab rescue.
Severe and Fulminant Ulcerative Colitis
Hospitalize for IV fluids, electrolytes, bowel rest, and broad-spectrum antibiotics (e.g., ciprofloxacin + metronidazole). IV corticosteroids first-line. Rescue therapies: IV cyclosporine or infliximab (5mg/kg). Colectomy if no response in 48-96 hours or perforation signs. Anti-TNF like infliximab reduces colectomy risk by 50% at 90 days.
Aminosalicylates (5-ASA)
First-line for mild-moderate UC. Mesalamine (Asacol, Lialda, Apriso), sulfasalazine, balsalazide, olsalazine deliver 5-ASA to colon via pH-dependent or prodrug mechanisms. Doses: 2.4-4.8g/day oral; 1g suppository or 4g enema rectally. Once-daily formulations improve adherence. Folic acid (1mg/day) with sulfasalazine due to folate malabsorption. Effective for induction (50-70%) and maintenance (60-80%).
- Pros: Safe long-term, mucosal healing.
- Cons: Rare nephrotoxicity (monitor creatinine), headaches.
Corticosteroids
For moderate-severe flares unresponsive to 5-ASA. Oral prednisone 40mg/day taper; budesonide-MMX for ileal release minimizes systemic effects. Rectal foams/liquids for distal disease. IV for severe: methylprednisolone 16-20mg q8h or continuous infusion (no superiority over bolus). Not for maintenance due to osteoporosis, diabetes, infection risks.
Immunomodulators
For steroid-dependent UC or to spare biologics. Azathioprine (2-2.5mg/kg/day), 6-mercaptopurine (1-1.5mg/kg/day) inhibit purine synthesis, onset 3-6 months. Monitor TPMT levels pre-treatment. Methotrexate (25mg/week IM) alternative. Efficacy: 50-60% steroid-free remission.
- Side effects: Pancreatitis, myelosuppression, hepatotoxicity, lymphoma risk (rare).
Biologics and Small Molecules
For moderate-severe refractory UC. Target cytokines or trafficking.
- Anti-TNF: Infliximab (5mg/kg weeks 0,2,6 then q8w), adalimumab (160/80/40mg induction), golimumab. Response 60-70%, remission 30-40%. Test for antibodies.
- Anti-integrin: Vedolizumab (300mg IV q8w) gut-selective, safer infections.
- Anti-IL-12/23: Ustekinumab (IV induction then SC).
- JAK inhibitors: Tofacitinib (10mg BID induction, 5-10mg BID maint), upadacitinib.
- S1P modulator: Ozanimod reduces lymphocyte migration.
Infliximab effective in trials (ACT-1/2): higher remission vs placebo at weeks 8-54.
Surgery for Ulcerative Colitis
Curative: proctocolectomy with ileal pouch-anal anastomosis (IPAA) or end-ileostomy. Indications: refractory disease, cancer, perforation, dysplasia. 20-30% lifetime risk. IPAA restores continence but risks pouchitis (treat with cipro/metronidazole).
Other and Emerging Therapies
Probiotics for pouchitis maintenance. Nicotine patches for ex-smokers (limited). Fish oil omega-3s adjunctive. Investigational: tacrolimus (10-15ng/ml targets remission in refractory, high side effects), rosiglitazone, Trichuris suis ova (43% improvement vs 17% placebo).
Lifestyle and Supportive Care
Diet: low-residue during flares, no specific trigger avoidance proven. Loperamide for diarrhea (avoid severe). Hydration, nutrition support. Vaccinations, bone density screening on steroids. Smoking cessation worsens UC—unlike Crohn’s.
Frequently Asked Questions (FAQs)
What is the first-line treatment for mild ulcerative colitis?
Aminosalicylates like mesalamine enemas or oral formulations induce and maintain remission effectively with minimal side effects.
When is surgery considered for UC?
For medically refractory disease, acute severe colitis failing rescue therapy, or dysplasia/cancer. Proctocolectomy cures UC.
Are biologics safe long-term?
Yes, with monitoring for infections, malignancies. Gut-selective like vedolizumab lower systemic risks.
Can diet cure ulcerative colitis?
No, but low-fiber during flares helps symptoms. No universal diet; personalized nutrition aids management.
How do I prevent UC flares?
Adhere to maintenance therapy (e.g., mesalamine), manage stress, avoid NSAIDs, regular follow-ups.
References
- Ulcerative Colitis: Current Treatment Strategies and Future Prospects — PMC/NCBI. 2010-11-01. https://pmc.ncbi.nlm.nih.gov/articles/PMC3002512/
- Ulcerative Colitis – Digestive Disorders – Merck Manuals — Merck Manuals (updated regularly, accessed 2026). https://www.merckmanuals.com/home/digestive-disorders/inflammatory-bowel-diseases-ibd/ulcerative-colitis
Read full bio of medha deb