Ungual Squamous Cell Carcinoma In Situ
Understanding periungual Bowen disease: Clinical features, diagnosis, and treatment options.

Ungual Squamous Cell Carcinoma In Situ: Overview
Ungual squamous cell carcinoma in situ (SCCIS), commonly referred to as periungual Bowen disease, represents a superficial intraepidermal malignancy affecting the nail unit region. This condition is characterized by the proliferation of atypical squamous cells confined to the epidermis without invasion into the dermis or deeper structures. The ungual region, which includes the nail bed, nail folds, and surrounding periungual tissue, presents a unique anatomical challenge for both diagnosis and treatment due to its specialized structure and functional importance.
Unlike invasive cutaneous squamous cell carcinoma, ungual SCCIS remains localized to the epidermal layer, making it a potentially curable condition when detected early and managed appropriately. The condition represents approximately 5-10% of all squamous cell carcinomas affecting the nail unit, making it a relatively uncommon but clinically significant presentation of intraepidermal carcinoma.
Etiology and Risk Factors
The primary causative factor for ungual squamous cell carcinoma in situ is prolonged exposure to ultraviolet (UV) radiation from sunlight. UV radiation damages the deoxyribonucleic acid (DNA) within skin cell nuclei, leading to mutations and abnormal cloning of the p53 gene, which normally functions as a tumor suppressor. This mutational process results in the uncontrolled proliferation of atypical keratinocytes characteristic of SCCIS.
Additional risk factors contributing to the development of ungual SCCIS include:
- Chronic sun exposure, particularly in individuals with occupational exposure to sunlight
- Fair skin type and reduced ability to synthesize protective melanin
- Immunosuppression from medications or systemic conditions
- Arsenic ingestion or exposure
- Viral infections, including human papillomavirus (HPV)
- Chronic irritation or trauma to the nail unit
- Advanced age, as cellular repair mechanisms decline with aging
Patients with ungual SCCIS frequently have a history of other keratinocytic skin cancers, with up to 50% having concurrent or prior basal cell carcinoma, actinic keratosis, or other forms of squamous cell carcinoma elsewhere on the body.
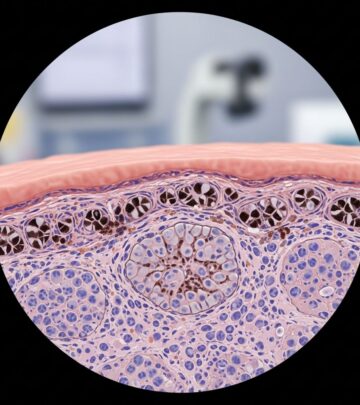
Pathological Characteristics
Histopathological examination reveals several distinctive features of ungual squamous cell carcinoma in situ. The epidermis demonstrates full-thickness dysplasia with atypical keratinocytes spanning from the basal layer through the granular layer. Key pathological findings include:
- Hyperkeratosis and parakeratosis (retention of nuclei in the stratum corneum)
- Prominent acanthosis with elongation and thickening of rete ridges
- Loss of the normal granular layer architecture
- Cytologic atypia of keratinocytes with pleomorphic nuclei and increased mitotic activity
- Enlarged hyperchromatic nuclei with increased nuclear-to-cytoplasmic ratios
- Potential hair follicle involvement in periungual locations
The stromal-epidermal interface typically remains intact, with no invasion into the underlying dermis. This preservation of the basement membrane distinguishes SCCIS from invasive squamous cell carcinoma and carries significant prognostic implications, as the lack of dermal invasion substantially reduces the risk of metastatic spread.
Pigmented variants of ungual SCCIS show increased melanin deposition throughout the epidermis and within melanophages in the superficial dermis. Pagetoid variants display discrete, enlarged solitary and nested atypical keratinocytes scattered through the upper epidermal layers, sometimes mimicking Paget disease or melanoma in situ. In these diagnostically challenging cases, immunoperoxidase staining serves as a discriminatory tool to establish the correct diagnosis.
Clinical Presentation
Ungual squamous cell carcinoma in situ typically manifests as one or more irregular scaly plaques affecting the nail unit and periungual tissues. The clinical appearance varies depending on the specific location within the nail complex and the chronicity of the lesion.
Common clinical features include:
- Red or orange-red colored plaques, though brown variants also occur
- Irregular borders with scaling or crusting
- Size ranging from a few millimeters to several centimeters in diameter
- Nail dystrophy, including ridging, thickening, or discoloration
- Erosion or ulceration of the nail plate or nail bed
- Paronychia-like inflammation affecting the nail folds
- Bleeding or drainage from the affected nail unit
The lesions typically develop slowly over weeks to months, though rapid progression can occasionally occur, particularly in immunocompromised patients. Many patients report a preceding history of chronic irritation, trauma, or a long-standing lesion that previously remained stable before undergoing change or growth acceleration.
Ungual SCCIS most commonly affects the thumb and index fingers of middle-aged to elderly patients, though any digit can be involved. The condition is rare in children and young adults, reflecting the cumulative nature of UV damage and the age-related decline in cellular repair mechanisms.
Diagnostic Evaluation
Accurate diagnosis of ungual squamous cell carcinoma in situ requires integration of clinical, dermoscopic, and histopathological findings. A complete diagnostic approach should include the following components:
Clinical Examination
A thorough clinical examination of the nail unit should assess the specific location of the lesion (nail bed, nail matrix, nail fold, or adjacent skin), the extent of involvement, associated nail dystrophy, and the presence of ulceration or drainage. Careful inspection of the surrounding periungual tissue and the contralateral nail unit provides valuable comparative information. General examination of the skin should exclude other concurrent keratinocytic malignancies, which occur in approximately half of patients with ungual SCCIS.
Dermoscopic Evaluation
Dermoscopy of ungual SCCIS may reveal crops of rounded and coiled blood vessels within the lesion, which supports the diagnosis when present. This vascular pattern represents capillary proliferation associated with the inflammatory response to neoplastic keratinocytes. The dermoscopic appearance varies with the lesion’s maturity and pigmentation but typically shows irregular patterns consistent with dysplasia.
Biopsy and Histopathology
Skin biopsy represents the gold standard for definitive diagnosis of ungual squamous cell carcinoma in situ. Both punch and shave biopsies are appropriate for ungual SCCIS, though punch biopsies may provide better depth assessment of the stromal-epidermal relationship. Biopsy specimens should be obtained from the lesion itself and include adjacent clinically normal-appearing tissue to assess margins and exclude dermal invasion.
Samples should be sent to an experienced dermatopathologist familiar with nail unit pathology, as accurate assessment of invasion and proper interpretation of the nail unit architecture are essential for treatment planning. The histopathological demonstration of full-thickness epidermal dysplasia confined above the basement membrane confirms the diagnosis of SCCIS.
Differential Diagnosis
Several conditions may mimic ungual squamous cell carcinoma in situ clinically and histopathologically, necessitating careful diagnostic discrimination:
- Melanoma in situ: May present with similar pigmentation and dysplastic features; immunohistochemistry readily distinguishes this diagnosis
- Paget disease: Characterized by pagetoid spread of cells with pale cytoplasm; immunostaining confirms Paget disease
- Actinic keratosis: Limited thickness dysplasia confined to lower epidermis, without full-thickness involvement
- Bowenoid papulosis: Typically affects younger patients in genital regions; often HPV-associated with better prognosis
- Atypical fibroxanthoma: Demonstrates dermal mesenchymal origin rather than epithelial derivation
- Paronychia: Inflammatory nail fold condition without dysplasia on histopathology
Treatment Options
The management of ungual squamous cell carcinoma in situ requires individualized treatment planning based on lesion size, location, depth of involvement, patient age, and functional considerations regarding nail preservation. Multiple treatment modalities are available, each with distinct advantages and limitations:
Surgical Excision
Histological mapping with local excision represents the standard treatment approach for ungual SCCIS. This technique involves complete excision of the lesion with adequate margins (typically 3-5mm of clinically normal tissue) and complete histopathological examination of the margins to ensure complete removal. Excision should extend to the reticular dermis to ensure complete elimination of the lesion and exclude any invasive component.
Surgical reconstruction of the nail unit after excision varies depending on the lesion’s location and extent. Small lesions confined to the nail bed may be managed with simple closure. Larger defects may require nail bed grafting, local flap reconstruction, or partial nail ablation to preserve function and appearance. The thumb and index finger carry higher functional importance, making nail preservation a priority when feasible.
Topical Therapy
Topical treatment options include imiquimod, a topical immune response modifier that enhances cellular and humoral immune responses to dysplastic keratinocytes, and 5-fluorouracil (5-FU), a topical antineoplastic agent that inhibits thymidylate synthase and disrupts nucleotide synthesis. These topical agents are typically reserved for early-stage lesions, lesions where surgical intervention poses significant functional compromise, or patients who refuse surgical treatment.
Topical therapy requires prolonged application (typically 4-12 weeks) and careful monitoring for local irritation. Success rates with topical therapy are variable, ranging from 60-80% for favorable lesions, with recurrence rates higher than surgical approaches. Combination therapy with topical agents may improve efficacy in some cases.
Other Treatment Modalities
Alternative treatments, including laser therapy (carbon dioxide or erbium laser), cryotherapy, and photodynamic therapy, may be considered in select cases, particularly when preserving nail structure is paramount. These modalities are generally reserved for small lesions or cases with significant surgical risk. Long-term recurrence data for these approaches in ungual locations remain limited.
Prognosis and Recurrence
Ungual squamous cell carcinoma in situ has a favorable prognosis when detected early and treated appropriately, as the condition lacks the invasive potential of cutaneous SCC. Metastatic spread is exceptionally rare in true SCCIS, with virtually no risk of distant metastasis or systemic dissemination.
However, recurrence rates are notably high following treatment of ungual SCCIS, particularly in immunocompromised patients. Recurrence rates range from 10-40% depending on the treatment modality employed, with surgical excision generally demonstrating lower recurrence rates (10-20%) compared to topical therapy or non-surgical approaches (30-40%). Recurrence may represent incomplete initial treatment or field change with development of new lesions in the surrounding ungual tissue.
Long-term follow-up with regular clinical and dermoscopic examination is essential for detecting early recurrence. Patients with recurrent SCCIS may require re-excision or alternative treatment strategies. Development of invasive carcinoma from incompletely treated SCCIS, while uncommon, can occur and carries substantially worse prognosis with potential for metastatic spread.
Prevention and Surveillance
Prevention of ungual squamous cell carcinoma in situ focuses on minimizing UV exposure through consistent use of broad-spectrum sunscreen (SPF 30 or higher), protective clothing, and avoidance of peak sun exposure hours. Individuals with risk factors for skin cancer, including fair skin, personal or family history of skin cancer, or immunosuppression, should perform regular self-examination of the nail units and seek prompt evaluation of any changes in appearance, bleeding, or dystrophy.
Patients with ungual SCCIS should undergo complete skin examination by a dermatologist to detect concurrent keratinocytic malignancies elsewhere on the body. Annual follow-up visits are recommended for surveillance of the treated site and early detection of recurrence. Patients with immunosuppression or multiple recurrences may benefit from more frequent monitoring intervals.
Frequently Asked Questions
Q: What is the difference between ungual SCCIS and invasive squamous cell carcinoma of the nail?
A: Ungual SCCIS remains confined to the epidermis above the basement membrane, while invasive SCC extends into the dermis and deeper structures. SCCIS carries no meaningful risk of metastasis, whereas invasive SCC can spread to lymph nodes and distant sites. The distinction is made histopathologically and carries significant prognostic implications.
Q: Why are recurrence rates higher in ungual SCCIS compared to truncal lesions?
A: The nail unit’s specialized anatomy, chronic irritation from nail growth and trauma, and the technical challenges of complete excision while preserving function contribute to higher recurrence rates. Additionally, the periungual region demonstrates significant field cancerization, with surrounding tissue at risk for developing new lesions.
Q: Can topical therapy alone cure ungual SCCIS?
A: Topical therapy achieves complete clearance in approximately 60-80% of early-stage lesions but carries higher recurrence rates than surgical excision. Topical therapy is best reserved for small lesions, patients with significant surgical risk, or as adjunctive therapy following incomplete excision.
Q: How often should patients be followed after treatment of ungual SCCIS?
A: Annual clinical and dermoscopic examination is recommended for surveillance. Patients with recurrent disease, immunosuppression, or large initial lesions may require more frequent monitoring at 3-6 month intervals to detect early recurrence.
Q: Is nail preservation always possible with ungual SCCIS treatment?
A: Small lesions confined to the nail bed or nail folds may be removed while preserving nail structure and function. However, extensive lesions involving the nail matrix or requiring wide margins may necessitate partial nail ablation or nail loss as a trade-off for complete oncologic control and prevention of recurrence.
Q: What signs warrant urgent evaluation of a nail lesion?
A: Bleeding or drainage from the nail unit, rapid growth of a nail lesion, nail dystrophy with color changes, persistent paronychia unresponsive to standard treatment, and ulceration of the nail plate or nail bed all warrant prompt dermatologic evaluation to exclude malignancy.
References
- Squamous Cell Carcinoma in Situ Pathology — DermNet New Zealand. Accessed January 2026. https://dermnetnz.org/topics/squamous-cell-carcinoma-in-situ-pathology
- Intraepidermal Carcinoma — StatPearls, National Center for Biotechnology Information (NCBI). Updated 2024. https://www.ncbi.nlm.nih.gov/books/NBK482474/
- Intraepidermal Squamous Cell Carcinoma — DermNet New Zealand. Accessed January 2026. https://dermnetnz.org/topics/intraepidermal-squamous-cell-carcinoma
- Cutaneous Squamous Cell Carcinoma — DermNet New Zealand. Accessed January 2026. https://dermnetnz.org/topics/cutaneous-squamous-cell-carcinoma
- Dermoscopy of the Nail — DermNet New Zealand. Accessed January 2026. https://dermnetnz.org/cme/dermoscopy-course/dermoscopy-of-the-nail
Read full bio of medha deb