Urticarial Vasculitis: Clinical Presentation and Images
Visual guide to urticarial vasculitis: Understanding clinical presentation through diagnostic imagery.

Urticarial vasculitis is a rare form of vasculitis characterized by inflamed blood vessels that produce recurrent wheal-like lesions on the skin. This condition represents a unique subset of cutaneous small-vessel vasculitis that often presents diagnostic challenges due to its variable clinical manifestations and overlap with other dermatological conditions. Understanding the clinical presentation and visual characteristics of urticarial vasculitis is essential for accurate diagnosis and appropriate management. This article provides a comprehensive guide to the clinical features and diagnostic imagery associated with this condition.
Understanding Urticarial Vasculitis
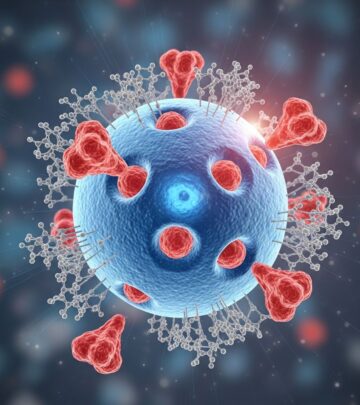
Urticarial vasculitis is distinguished by the presence of urticarial lesions that persist longer than 24 hours, differentiating it from typical urticaria where individual lesions resolve within this timeframe. The condition results from complement activation, which generates anaphylatoxins C3a and C5a that trigger mast cell degranulation, releasing histamine, cytokines, and chemokines. These substances recruit eosinophils and neutrophils to the affected sites. Neutrophils generate extracellular traps that directly damage blood vessel walls, leading to histologic signs of leukocytoclasia and the characteristic symptoms of urticarial vasculitis.
The disease can be either idiopathic or associated with underlying conditions such as infections, autoimmune disorders, malignancies, or certain medications. When a specific trigger is identified, addressing the underlying cause becomes the primary treatment focus before implementing symptomatic therapies.
Clinical Presentation Patterns
The clinical presentation of urticarial vasculitis varies considerably among affected individuals. Skin manifestations serve as the primary diagnostic feature, though systemic involvement may occur in more severe cases. The following characteristics define typical presentations:
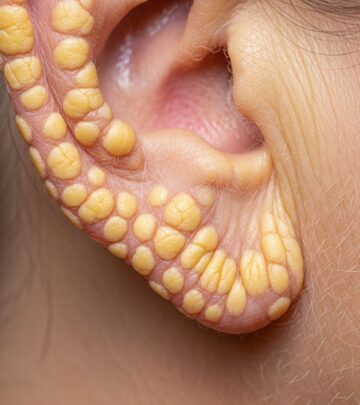
- Cutaneous Lesions: Persistent wheals and urticarial eruptions that do not resolve within 24 hours, often accompanied by erythema and induration
- Distribution Patterns: Lesions frequently appear on pressure-prone areas, lower extremities, and trunk regions
- Associated Symptoms: Pruritus, burning sensation, and occasionally pain at lesion sites
- Systemic Manifestations: Fatigue, joint pain, abdominal pain, fever, and lymphedema may accompany skin lesions in more severe presentations
- Ocular Involvement: Red eye and conjunctival changes may occur in systemic disease
Diagnostic Imaging and Visual Features
Visual examination of urticarial vasculitis lesions reveals characteristic patterns that assist in clinical diagnosis. The lesions typically appear as urticarial papules and plaques with variable morphology. Early lesions present as erythematous wheals, often with central clearing and surrounding erythema. As the condition progresses, lesions may develop purpuric or hemorrhagic components, particularly in more severe cases. The presence of persistent urticarial lesions that fail to blanch completely and demonstrate leukocytoclastic changes on histopathology provides diagnostic confirmation.
Photographic documentation of lesions aids in monitoring disease progression and treatment response. Serial imaging over time demonstrates the characteristic cyclical nature of urticarial vasculitis, with periods of relative quiescence interrupted by acute flares. The arrangement of lesions in groups or crops, along with the presence of both active and resolving lesions at different stages simultaneously, represents a hallmark presentation pattern.
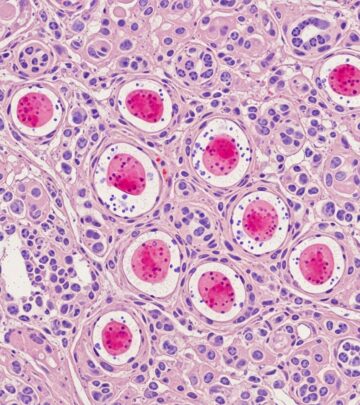
Histopathologic Features
While clinical presentation provides initial diagnostic clues, histopathologic examination offers definitive confirmation. Features of leukocytoclastic vasculitis observed on histopathologic examination are diagnostic of urticarial vasculitis, though not always present in every biopsy specimen. Key histologic findings include:
- Infiltration of small vessels with neutrophils and eosinophils
- Nuclear debris from fragmented neutrophils (leukocytoclasia)
- Endothelial swelling and cell damage
- Fibrin deposition within and around vessel walls
- Red blood cell extravasation into surrounding tissue
- Variable degree of dermal edema
Immunofluorescence studies may reveal immunoglobulin and complement deposits at the dermal-epidermal junction, particularly in cases with systemic involvement or complement depletion patterns.
Clinical Variants and Presentations
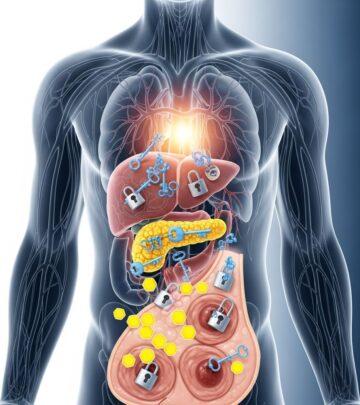
Urticarial vasculitis presents with variable clinical patterns that influence management strategies. Cutaneous-limited disease confined to skin manifestations generally follows a more favorable course with better response to topical and systemic therapies. In contrast, systemic urticarial vasculitis involving multiple organ systems requires more aggressive immunosuppressive approaches.
Hypocomplementemic urticarial vasculitis represents a distinct subset characterized by low serum complement levels, often associated with more severe systemic manifestations. This variant frequently involves additional organ systems and demonstrates a more chronic, relapsing course requiring prolonged immunosuppressive therapy.
Triggers and Associations
While many cases of urticarial vasculitis remain idiopathic, recognizable triggers include infections, autoimmune conditions, malignancies, and specific medications. Understanding potential precipitating factors guides investigation and influences treatment planning. Common associations include:
- Systemic lupus erythematosus and other connective tissue diseases
- Hepatitis and other infectious agents
- Underlying malignancies
- Certain medications including antibiotics and NSAIDs
- Environmental antigens and allergen exposures
Identifying and addressing underlying conditions, when present, represents a crucial component of comprehensive disease management and often leads to significant clinical improvement.
Treatment Approaches
Treatment strategies for urticarial vasculitis depend on disease severity and extent of organ involvement. For cutaneous-limited disease, initial management may include antihistamines and NSAIDs such as ibuprofen or naproxen to relieve symptoms. However, antihistamines alone fail to address the underlying pathogenic mechanism and prove ineffective in most patients.
First-line therapies for persistent disease include dapsone, colchicine, and hydroxychloroquine. These medications address the underlying immune activation without the significant side effects associated with prolonged corticosteroid use. Corticosteroids such as prednisone prove effective in resolving cutaneous disease in approximately 80% of patients and significantly decrease systemic symptoms, though corticosteroids are generally reserved for moderate-to-severe cases or when other treatments fail due to potential long-term complications.
For severe systemic disease, immunosuppressive agents including methotrexate, mycophenolate mofetil, azathioprine, and cyclophosphamide may be necessary. Recent advances include biologic therapies such as rituximab, omalizumab, and interleukin-1 inhibitors, which show promise for recalcitrant or refractory cases. IL-1 inhibitors (anakinra and canakinumab) demonstrate particular efficacy with concurrent improvement in serological markers and clinical disease.
Patient Monitoring and Long-term Management
Comprehensive patient evaluation should include assessment of vital organs, particularly the kidneys and lungs, especially when blood complement levels are low. Initial laboratory investigations typically include complete blood count, comprehensive metabolic panel, complement levels, and serologic markers for underlying systemic disease.
Many patients experience a cyclical pattern of disease activity characterized by quiet periods interspersed with acute flares that may be triggered by intercurrent infections or other precipitating factors. Long-term monitoring remains essential to detect emergence of systemic disease or unmasking of underlying diagnoses. Treatment strategies should be individualized based on disease response patterns, with ongoing adjustments to optimize clinical outcomes while minimizing medication side effects.
Frequently Asked Questions
Q: How does urticarial vasculitis differ from typical urticaria?
A: The primary distinction lies in lesion duration. Urticarial vasculitis produces wheals that persist longer than 24 hours and demonstrate leukocytoclastic changes on histology, whereas typical urticaria lesions resolve within 24 hours without significant vasculitis.
Q: Is urticarial vasculitis contagious?
A: No, urticarial vasculitis is not contagious. It results from immune system dysfunction and vascular inflammation rather than infectious transmission.
Q: Can urticarial vasculitis resolve spontaneously?
A: Skin-limited disease may resolve on its own in some cases, particularly when identifiable triggers are removed or underlying conditions are treated. However, many patients require ongoing medical management for disease control.
Q: What organs are commonly affected in systemic urticarial vasculitis?
A: The kidneys, lungs, gastrointestinal tract, and eyes are frequently involved in systemic disease. Joint involvement causing arthralgias is also common.
Q: How long does urticarial vasculitis typically last?
A: Disease duration varies considerably. Some patients experience resolution within months, while others develop chronic or relapsing-remitting patterns requiring treatment for several years.
Q: Are there specific triggers I should avoid?
A: If specific triggers have been identified—such as particular medications, foods, or environmental exposures—these should be avoided when possible. However, many cases remain idiopathic without identifiable triggers.
References
- Urticarial vasculitis — PubMed Central, National Institute of Health. 2021. https://pmc.ncbi.nlm.nih.gov/articles/PMC8243153/
- Urticarial Vasculitis: Symptoms, Causes, Treatment, and More — Healthline Media. 2024. https://www.healthline.com/health/urticarial-vasculitis
- Urticarial Vasculitis — Dermatology Advisor. 2024. https://www.dermatologyadvisor.com/ddi/urticarial-vasculitis/
- Urticarial Vasculitis — Vasculitis Foundation. 2024. https://vasculitisfoundation.org/education/vasculitis-types/urticarial-vasculitis/
- Urticarial Vasculitis Brochure — Vasculitis Foundation. 2024. https://vasculitisfoundation.org/wp-content/uploads/2024/03/2024-VF_Urticarial-Vasculitis-Brochure.pdf
- Urticarial Vasculitis — DermNet. 2024. https://dermnetnz.org/topics/urticarial-vasculitis
- Urticarial Vasculitis — Vasculitis UK. 2024. https://www.vasculitis.org.uk/about-vasculitis/urticarial-vasculitis
Read full bio of medha deb